06/07/2018 Category: Childbirth Author: Alena Lomakina
Every expectant mother looks forward to the birth of her baby and wants everything to go well. Natural childbirth is a difficult and exhausting process, requiring a lot of strength and health from the body, and sometimes the condition of the woman in labor or the baby in the womb does not allow her to survive everything from beginning to end without complications. Therefore, many women have to hear from doctors a proposal to perform a caesarean section.
- Indications for planned CS
- Indications for emergency CS
- Possible consequences of a caesarean section
- Reviews about caesarean section
Conditions for the operation
A caesarean section can be elective, planned or emergency. A planned delivery operation is said to occur when it is performed 6 to 15 days before the date of expected birth, with maternal and/or fetal indications available and the first manifestations of labor absent (see calculator for calculating the expected date of birth).
A planned operation means that the indications for it are known in advance, often in the first weeks and even days of bearing the unborn baby. The need for an emergency section arises due to urgent, immediate delivery within approximately one to two hours and is mainly indicated in the process of spontaneous childbirth. A planned caesarean section is spoken of when labor has just begun or the amniotic fluid has leaked prematurely, but there are relative indications for the operation. That is, a woman is allowed to go into labor, but according to the labor management plan, it ends with an operation.
So, the necessary factors for the surgical method of delivery:
- the presence of a living fetus capable of existing outside the womb (considered a relative condition, since in some circumstances the operation is performed in the interests of the woman in order to preserve her life);
- written consent of the woman in labor for a caesarean section;
- empty bladder (it is advisable to install a permanent catheter);
- there are no signs of infection during childbirth (also a very conditional indication);
- availability of an experienced obstetric surgeon and operating room.
What is a caesarean section
A caesarean section in medicine is an operation whose purpose is to remove a baby from a woman's uterus through an incision in the abdomen. Every 8th pregnancy ends with such an operation. Moreover, the risk of complications and other unpleasant symptoms during cesarean section is much lower than during natural childbirth.
Caesarean section is prescribed by the gynecologist leading the pregnancy according to indications. The expectant mother prepares in advance for the operating process. There are emergency cases when a woman experiences difficulties or complications during natural childbirth.
What are the indications for surgery?
All reasons that lead to abdominal delivery can be divided into two subgroups.
- Absolute indications literally force the doctor to give birth to the woman surgically, that is, surgery cannot be avoided.
- Relative indications are spoken of when the situation is analyzed by a council of doctors and a conclusion is approved on one or another method of completing childbirth. That is, a woman can give birth on her own, but the likely risks for her, as well as the baby, are taken into account.
In addition, there are factors that lead to forced surgery during pregnancy or directly during childbirth. Another gradation of indications for surgical delivery is their division into maternal and fetal factors.
Recovery period
After childbirth, the uterus returns to its previous state after 6-8 weeks. But the recovery period after surgical childbirth lasts longer than after natural childbirth. After all, the uterus is injured, and the suture does not always heal safely.
https://www.youtube.com/watch?v=tPN-saQ0ct0
In many ways, the recovery period depends on how the planned caesarean section went and how successfully it was done.
At the end of the operation, the patient is moved to the recovery room or intensive care unit. To prevent the occurrence of infectious complications, antibacterial therapy is carried out.
To relieve pain, anesthetic injections are given. Both general and spinal anesthesia slow down bowel function, so in the first 24 hours after the intervention you are only allowed to drink water.
But already on the second day you can eat chicken broth with crackers, kefir, and yogurt without additives. For 6-7 days you should follow the same diet as after any abdominal surgery: no fatty, fried, or spicy foods. After this period, you can return to your usual diet.
Constipation is highly undesirable. The use of laxative products is recommended, but if this does not help, you will have to resort to the use of laxatives. If a woman is breastfeeding, the annotation should indicate that use during breastfeeding is permitted.
While a woman is in the maternity hospital, her postoperative suture is treated daily.
After discharge, you need to continue to do this yourself with the help of hydrogen peroxide and brilliant green. If the suture festers, ichor comes out of it, or shooting pains appear, you need to tell the doctor about it. Read more: suture care after cesarean section→
In the first weeks, it is not recommended to lift anything heavier than the baby's weight. You can return to fitness activities no earlier than after 8 weeks and only after examination by a doctor. This also applies to resuming sexual activity.
This operation seems simple to many women, but in order for it to go well, the doctor must be highly qualified, and the woman in labor must follow all recommendations regarding the recovery period.
Abdominal delivery: absolute indications
Maternal factors that, if present, cannot be avoided without a cesarean section include:
Anatomically narrow pelvis (the degree of narrowing is taken into account, that is, 3 - 4, in which the true conjugate is 9 cm or less)
The narrow pelvis is divided into 2 groups according to the shape of the narrowing.
- The first group includes: a transversely narrowed pelvis, a flat pelvis (a simple flat pelvis, a flat-rachitic pelvis and a pelvis with a decrease in the wide part of the cavity), and, of course, a generally uniformly narrowed pelvis. These are quite common forms of pelvic contractions.
- The second group (rare forms) includes an oblique pelvis, a constricted pelvis, pelvic deformation due to bone exostoses, bone tumors or due to fractures, a kyphotic pelvis, a funnel-shaped pelvis and other types of narrow pelvises.
An anatomically narrow pelvis with degree 3 or 4 can complicate the course of labor. During labor, almost 40% of women in labor experience:
- weakness of uterine contractions (contractions)
- early rupture of water
- possible prolapse of the umbilical cord or fetal arms/legs
- development of chorioamnionitis, endometritis and infection of the unborn baby
- as well as intrauterine fetal hypoxia
During the pushing period, the following complications may appear:
- secondary weakness of pushing
- intrauterine hypoxia of a child
- birth injury
- uterine rupture
- tissue necrosis with the formation of genitourinary fistulas, entero-genital fistulas
- injury to the pelvic joints and nerve plexuses
- and if childbirth reaches the third period, then subsequent and/or postpartum bleeding cannot be avoided.
Complete placenta previa
As you know, the placenta is the organ that communicates between the organisms of mother and child. In a normal pregnancy, the placenta is located either in the fundus of the uterus, or along the anterior or posterior wall. If the placenta is located in the lower segment of the fetal sac, and completely covers the internal pharynx, then it becomes clear that the child’s exit from the mother’s womb naturally becomes impossible. Moreover, complete placenta previa poses a potential threat not only to the unborn baby, but also to his mother throughout the entire period of pregnancy, because bleeding can occur at any moment, the intensity and duration of which cannot be predicted.
Case study : I saw a 38-year-old woman from the very beginning of her pregnancy. This was not the first pregnancy, but it was very welcome. Despite the absence of any aggravating circumstances in her medical history, her placenta formed in the lower third of the uterus and blocked the internal os (complete presentation). The woman spent almost the entire pregnancy on sick leave, under the supervision of doctors, and did not experience a single bleeding. She successfully progressed to 37 weeks and was admitted to the pathology ward in preparation for a planned caesarean section. Well, as usual, for some reason (or maybe fortunately) her bleeding began in the hospital and on a day off. Of course, we immediately went for an immediate caesarean section; there was no time to waste. This is how a planned operation turned into an emergency - the child was born healthy and of normal weight.
Incomplete placenta previa with severe bleeding
Incomplete placenta previa is said to occur when the placenta only partially covers the internal os. There are regional and lateral presentations.
- When the placenta is located marginally, it only slightly affects the internal os
- Whereas with the side it overlaps by half or 2/3 of the diameter.
Incomplete placenta previa also threatens sudden bleeding, the severity of which is difficult to predict. The peculiarity of this localization of the placenta is interesting in that bloody discharge more often appears during labor, because it is at this time that the internal os opens and the placenta gradually exfoliates. The indication for urgent surgery in case of incomplete presentation is massive blood loss, which poses a danger to the life and health of the mother and child.
Premature abruption of a normally located placenta
The placenta can detach either while you are expecting your baby or during labor (usually). The danger of this condition also lies in the occurrence of bleeding, which can be external (that is, visible) - there is bloody discharge from the vagina, internal or hidden (blood accumulates between the placenta and the uterine wall, forming a retroplacental hematoma), and mixed (there is both visible and hidden bleeding) Depending on the area of placental abruption, there are 3 degrees of severity: with moderate and, of course, severe degrees, it is necessary to give birth to the woman in labor as soon as possible, otherwise you can lose not only the baby, but also the mother.
Impending or incipient uterine rupture
There are a great many reasons leading to the threat of uterine rupture. This may be improper management of labor, incoordination of labor forces, large size of the fetus, and much more. In the absence of timely treatment (massive tocolysis, that is, stopping uterine contractions), the threat or beginning of a rupture will very quickly turn into an accomplished, that is, a completed rupture, and both “participants” of the birth, the woman and the unborn child, will die.
Incompetent scar on the uterus
A suture on the uterine wall occurs not only after abdominal delivery, but also after other gynecological operations (for example, conservative myomectomy). The fullness of the scar is determined by ultrasound, and the thickness of the scar-changed surface should reach 3 mm or more, the contours of the scar are even in the absence of connective tissue. If there was a complicated course in the postoperative period (for example, fever, endometritis or long healing of skin sutures) in the anamnesis, this indicates an inferior scar.
Two or more scars on the uterus
If you have a history of two or more cesarean sections, there is no question of independent delivery, since this condition of the uterus significantly increases the risk of rupture along the scar.
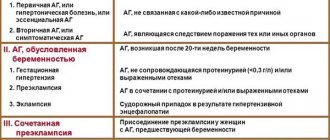
Severe forms of gestosis in the absence of a positive effect from therapy and unprepared birth canal
Eclampsia (convulsive attack) can be fatal for a woman and her child (see gestosis during pregnancy). Therefore, this condition requires immediate relief from the burden. Exactly 2 hours are allotted for the treatment of preeclampsia (preconvulsive stage); if there is no effect, immediate surgery is started. Severe and moderate nephropathy should be treated for no more than two weeks, after which the issue of surgery is decided.
Severe extragenital diseases
The list of indications for surgery includes:
- heart disease in the stage of decompensation
- pathology of the nervous system
- severe thyroid disease
- diabetes
- hypertension and much more
Caesarean section for vision is performed in cases of myopia of the 3rd degree (6 or more), complicated myopia, vision surgery, etc. In case of poor vision, it is necessary to exclude the period of pushing, since significant physical activity can lead to retinal detachment and blindness of the woman.
Anomalies of the structure of the uterus and vagina
In the presence of these defects, the contractile activity of the uterus is disrupted, and the fetus is not able to independently pass through the birth canal during childbirth.
- Tumors of the cervix, ovaries and other pelvic organs
- Such tumors close the birth canal and create an obstacle to the birth of the child.
- Extragenital cancer and malignant tumor of the cervix
- Age-related primigravida
Indications for cesarean section based on age (over 30 years) must be combined with obstetric pathology and extragenital diseases. In older primigravidas, the elasticity of the muscles of the vagina and pelvic floor is reduced, so there is a high risk of perineal ruptures. In addition, such women in labor often develop abnormalities of labor forces that are not relieved by therapy.
Fetal factors requiring surgical delivery:
- Malposition
In a normal pregnancy, the fetus should be positioned longitudinally, with the head towards the pelvis. The incorrect position of the unborn child is indicated when he lies obliquely, transversely, or the pelvic end is presented. Caesarean section for breech presentation is performed when the baby weighs more than 3600 g. or less than 1500 grams, as well as with a male fetus (compression of the testicles during birth of the pelvic end can cause infertility in a boy). Breech presentation (legs, pelvic end present) requires surgery, because the baby's head is larger than the pelvic end, and at the birth of the latter, the birth canal is not widened enough for unhindered advancement and birth of the head.
Case study: A woman was admitted to the maternity ward at night with strong contractions. This was her third birth, but she never had an ultrasound scan during the entire pregnancy. During a vaginal examination, I found that the legs were present, the opening of the cervical canal was 5 cm, and this was an absolute indication for delivery through surgery. When I cut the uterus and removed the fetus, I was stunned - the fetus was anencephalic with spina bifida in the cervical region (congenital deformity). Of course, he died immediately after cutting the umbilical cord. On the one hand, surgery for such a developmental anomaly is contraindicated, but on the other hand, who knew if the woman was not examined?
- Acute fetal hypoxia
This condition means that the child suffers in utero, there is not enough oxygen supplied to him, and each contraction aggravates hypoxia. There is only one treatment - immediate delivery.
Case Study : This was my first solo C-section since my internship. I spent the whole night working with a first-time mother, and in the morning I heard with my ear that the child was suffering - the heartbeat was slow and muffled, bradycardia. But we didn’t have a CTG (cardiotocograph) yet, so there was nothing to check it with. I went for the operation at my own peril and risk. And just in time, because she pulled out a child who didn’t even squeak or move his arms or legs. Due to his youth, I decided that he had died, but, fortunately, the child later recovered and was discharged healthy along with his mother.
- Presentation/prolapse of umbilical cord loop
In this situation, the operation must be performed immediately, since the prolapsed loop is pinched by the presenting part of the baby in the small pelvis, as a result of which the fetus is deprived of oxygen. Unfortunately, it is very rarely possible to operate on a woman and save the child.
- Death of a woman with a living fetus
In cases of ongoing agony, the child remains alive for some time and can be saved by abdominal delivery. The operation in such a situation is carried out in the interests of the fetus.
Relative readings
Maternal factors that decide the need for abdominal delivery (relative):
- Clinically narrow pelvis
This diagnosis is made during childbirth and means that the fetal head does not correlate with the size of the woman’s pelvis (the entrance to the pelvis is smaller than the head). The reasons for the development of this situation are numerous: a large fetus, incoordination of labor forces, incorrect insertion of the head, weak contractions, etc.
- Divergence of the symphysis pubis
During gestation, long before childbirth (observed both 2 weeks and 12 weeks), a woman may experience a divergence of the symphysis or pubic symphysis. This pathology is characterized by pain in the area of the symphysis and when palpating the pubis, clicking during palpation of the joint, swelling and swelling of the pubis forms above the pubis.
A pregnant woman notices discomfort when walking, getting up from a low chair or bed, or climbing stairs. The woman’s gait also changes, she becomes like a duck, waddling. During palpation of the symphysis pubis, a depression is found where the fingertip can freely fit. If the diagnosis is confirmed by ultrasound (pelvic x-ray is harmful to the fetus), the woman is prescribed bed rest, limited physical work and wearing a corset.
When the discrepancy of the symphysis pubis is 10 mm or more, especially if the estimated weight of the fetus reaches 3800 g. and moreover, if there is an anatomical narrowing of the pelvis, then the woman is prepared for planned abdominal delivery in order to prevent rupture of the symphysis pubis during spontaneous childbirth.
- Weakness of generic forces
When it is not possible to stimulate labor by opening the membranes to reduce the intrauterine volume and administering oxytocin, the birth must be completed by cesarean section. Weakness of labor forces leads to fetal hypoxia, postpartum hemorrhage and birth injuries.
- Post-term pregnancy
When deciding on abdominal delivery during post-term pregnancy, the ability of the head to adjust during labor, the intensity of contractions and aggravating factors (presence of extragenital diseases and gynecological pathology, no effect from induction of labor, etc.) are taken into account.
- IVF, artificial insemination or long-term infertility
This indication must be combined with a complicated obstetric-gynecological history (abortion (consequences), stillbirth, gynecological diseases, etc.).
- Chronic fetal hypoxia, intrauterine growth retardation
Considering that the fetus did not receive enough oxygen and nutrients throughout the pregnancy, and the treatment turned out to be ineffective, the question of surgical delivery before term for the benefit of the child is raised.
- Hemolytic disease of the fetus
Caesarean section for this indication is performed in the presence of an unprepared (immature) cervix.
- Large fruit
A fruit is said to be large when its estimated weight exceeds 4 kg, and gigantic if its weight reaches 5 kg or more. Childbirth ends with surgery if there is an existing concomitant pathology (complications during childbirth, gynecological problems and extragenital diseases).
- Multiple pregnancy
Abdominal delivery is performed when the pelvic end of the first fetus is presented or in the presence of three or more fetuses.
- Significant varicose veins in the vulva and vaginal area
There is a certain risk of damage to varicose veins during the pushing period, which is fraught with intense bleeding.
- Pregnant woman's request for surgery
In the West, for example, in England, the expectant mother has the freedom to choose her delivery. That is, it is possible for a pregnant woman to give birth by caesarean section at her request. In Russia, this indication is not officially recognized, but there are no documents prohibiting abdominal delivery at the request of the pregnant woman. Typically, this indication is combined with other relative indications.
Possible complications
A third of women experience complications after surgery.
- infection and inflammation of wounds and endometriosis;
- inflammation of sutures with pain, separation and suppuration;
- strong vaginal discharge;
- peritonitis and sepsis;
- inflammation of the appendages, resulting in disruption of the menstrual cycle, possible miscarriage and infertility;
- anemia is the most common complication after cesarean section due to large blood loss, so a balanced diet after childbirth is important;
- thromboembolism: even before deciding to perform a cesarean section, it is important to identify a predisposition to it in order to bandage the legs for preventive purposes and get up after the operation as early as possible.
Natural childbirth is a normal physiological process that is beneficial for mother and child. They create the preconditions for their psychological intimacy and favorable breastfeeding. There are pros to a cesarean section, but more cons. Experts recommend it only as an extreme and necessary measure.
- The fear of childbirth overcomes almost every expectant mother, and it doesn’t matter whether she has already been through it or not. Therefore, recently, an increasing number of pregnant women are thinking about a caesarean section. This method of delivery has, in a sense, even become fashionable.
- And everything seems to be so simple: no pain, a few hours of sleep - and you wake up next to your baby, snoring peacefully in a newborn cuvette.
But is everything as rosy as it seems at first glance? Of course, only you can make the decision, but it is better to do so knowing all the consequences of a cesarean section.
First, you need to understand what a caesarean section is. In general, this is a regular abdominal operation, during which an incision is made in the abdomen and uterus, after which the child is removed. But, like any surgical intervention, a caesarean section cannot but affect the condition of the woman and, oddly enough, the baby.
To be prepared for “surprises” associated with the proposed operation, we list the negative consequences that may await mothers after surgery:
- Painful sensations. If someone thinks that anesthesia given before the operation will completely relieve pain, then he is very mistaken. The effect of anesthesia will end, after which the “pleasant” sensations will begin. Discomfort will occur for several weeks after surgery. Yes, anesthetics will reduce the pain for a while, but in any case, you won’t be able to live fully during this time. After a caesarean section, the body takes much longer to recover than after a natural birth;
- Risk of infection. As before any operation, on the eve of a cesarean section, pregnant women are prescribed antibiotics to avoid infection, but the risk still exists. If you feel a fever, foul-smelling discharge, or heavy bleeding, tell your doctor or obstetrician immediately;
- Threat of blood clots. To reduce the likelihood of clots forming, blood thinners are usually prescribed before surgery. In addition, after a cesarean section, doctors advise starting to move as soon as possible to restore blood circulation. Wearing compression tights is also helpful;
- Possibility of formation of adhesions. A fairly common consequence of a cesarean section for the mother is the occurrence of internal adhesions. Experts say that this is a specific protective reaction of the body to surgery. Any wound recovers on its own, regardless of your or the doctor’s wishes, and scars often form in its place. Moreover, their occurrence is possible not only at the site of the wound itself, but also in nearby organs. Thus, adhesions between intestinal loops or other pelvic organs are a common consequence of cesarean section. As a result, the woman experiences painful and unpleasant sensations, there is a risk of developing intestinal obstruction, and possible infertility;
- Minimal physical activity. You will be able to get out of bed and approach your baby only six hours after the operation, and in the next few months you will need to take care of your body;
- Prohibition on putting the baby to the breast. All the bright prospects for a painless birth are shattered when you realize that your baby will not be able to receive such healthy colostrum in the first minutes of his life. In women who have undergone a cesarean section, lactation occurs at the same time as in those who give birth naturally, but breastfeeding a newborn is not allowed due to the effects of drugs administered to the mother during anesthesia. At first, the baby is bottle-fed, but if the woman in labor wants to start breastfeeding, she will have to wait until the anesthetic substances are completely removed from the body;
- Psychological discomfort. A factor that cannot be discounted. A common consequence of a caesarean section is difficulty in awakening the maternal instinct, that is, at first the mother does not manage to feel a connection with her baby.
Do not forget that anesthesia also has its side effects. Before undergoing a planned cesarean section, the expectant mother can choose the method of pain relief - epidural anesthesia or general anesthesia.
Any of them affects both the mother and the child. But since during general anesthesia several drugs are simultaneously introduced into a woman’s body, its consequences are much more noticeable.
If you choose an epidural, be prepared for back pain and shaky legs. If an error is made during the administration of the drug, traumatic damage to the spinal cord is possible. Yes, the probability is minimal, but it still exists.
The birth process is started by the child. The cherished moment comes only when the baby is completely ready for birth. A caesarean section operation violates all the laws of nature, and this cannot pass without leaving a trace for the baby:
- According to scientists, children born by cesarean section adapt much worse to the conditions of extrauterine life;
- With this method of birth, many babies retain amniotic fluid in their lungs, which in babies born naturally is pushed out during passage through the birth canal. The presence of fluid in the lungs subsequently provokes various disorders of the respiratory system;
- Anesthetic drugs that enter the child’s bloodstream have a negative effect on his nervous system;
- Increased excitability and muscle hypertonicity in caesarean calves are diagnosed more often than in children born as a result of natural birth.
The psychological consequences of a cesarean section for a child do not have direct evidence, however, experts have noticed that such children grow up infantile and dependent, they are not characterized by persistence in achieving goals and the desire to overcome difficulties, and it is very difficult for them to make decisions.
If the pregnancy is proceeding well, and there are no indications for surgical intervention, the best option for the birth of the baby would be a natural birth. But if, nevertheless, your choice falls on surgery, then it is better to know in advance about the possible consequences of a cesarean section.
Complications may occur during surgical childbirth and in the postoperative period. They do not depend on the period at which a planned caesarean section is performed.
Common complications are the following:
- Major blood loss. If a woman gives birth on her own, 250 ml of blood is considered acceptable blood loss, and during surgical delivery a woman can lose up to one liter of it. If the blood loss is too great, a transfusion will be required. The most dangerous consequence of heavy bleeding that cannot be stopped is the need to remove the uterus.
- Formation of adhesions. This is the name for seals made of connective tissue that “fuse” one organ with another, for example, the uterus with the intestines or intestinal loops with each other. After abdominal surgery, adhesions almost always form, but if there are too many of them, chronic pain in the abdominal area occurs. If adhesions form in the fallopian tubes, the risk of developing an ectopic pregnancy increases.
- Endometritis is an inflammation of the uterine cavity caused by the entry of pathogenic bacteria into it. Symptoms of endometritis can manifest themselves both on the first day after surgery and on the 10th day after childbirth. Read more about endometritis→
- Inflammatory processes in the suture area due to infection entering the suture. If antibiotic therapy is not started promptly, surgery may be required.
- Seam divergence. It can be triggered by a woman lifting weights (over 4 kilograms), and the dehiscence of the seam is a consequence of the development of infection in it.
To prevent complications, doctors take measures even before operations begin. To prevent the development of endometritis, the woman is given an antibiotic injection before the operation.
Antibacterial therapy continues for several days after. You can prevent the formation of adhesions by attending physiotherapy and doing special gymnastics.
Contraindications to abdominal delivery
All contraindications to cesarean section are relative, since the operation is always performed either in the interests of the mother or in the interests of the baby:
- unfavorable condition of the fetus (death in utero, prematurity 3 - 4 degrees, fetal malformations incompatible with life);
- probable or clinically manifested infection (long water-free period - over 12 hours);
- long labor (over 24 hours);
- more than 5 vaginal examinations;
- fever during childbirth (chorioamnionitis, etc.);
- failed attempt at natural delivery (obstetric forceps, vacuum extraction of the fetus).
Author:
Sozinova Anna Vladimirovna obstetrician-gynecologist