During pregnancy, a woman becomes more vulnerable to infections and diseases, since her immunity is significantly reduced. Therefore, doctors always strongly recommend that expectant mothers, if they have chronic diseases in their bodies, plan pregnancy. This means a thorough medical examination and identification of possible problems in order to cure them and prepare the body for bearing a child. After all, during pregnancy it will be difficult to treat diseases due to the negative effects of drugs on the fetus. So, what is the threat of thrombophilia to the expectant mother? What kind of disease is this and how to treat it for pregnant women?
Symptoms of thrombophilia
How can you suspect thrombophilia?
- History of thrombosis of arteries and veins.
Here we pay attention to all episodes of thrombosis, ranging from thrombosis of small vessels (hand, foot, retina) to deep vein thrombosis or severe thrombophlebitis and pulmonary embolism (PE). Family history is also important: any vascular accidents in relatives (thrombosis, embolism, thrombophlebitis, atherothrombosis, heart attacks and strokes, thrombosis of the veins and arteries of the retina) and the age of their initial appearance.
If thrombotic complications occur before the age of 40-45 years, the prognosis becomes more serious.
Men are more susceptible to thrombosis, so it would be a good idea to interview male blood relatives. Female relatives should be asked whether the thrombotic condition was provoked by taking combined oral contraceptives or pregnancy.
- Complicated obstetric history.
Within the framework of this topic, we are interested in: recurrent miscarriage, history of more than three frozen pregnancies, premature abruption of a normally located placenta, antenatal fetal death, fetoplacental insufficiency.
Of course, thrombophilia cannot be suspected in all of these situations. In some cases, the cause of miscarriage was an infection, in others a sharp rise in blood pressure provoked placental abruption, and antenatal fetal death occurred for completely different reasons (for example, decompensation of diabetes mellitus or umbilical cord pathology).
But habitual miscarriage in the absence of infections (herpesvirus infection, HIV infection and others) and chronic somatic diseases (hypothyroidism, diabetes, heart defects) is alarming in terms of the diagnostic search for thrombophilia.
Here it is also necessary to clarify the family history. Ask close relatives about problems with pregnancy, this will help in diagnosis.
Features of the disease
Thrombophilia in pregnant women is not detected so often, but there is a certain danger. A woman has a tendency to thicken her blood, which is why these clots or blood clots can linger in the vessels, blocking the gaps. In a normal state, the carrier of this gene (if we are talking about congenital thrombophilia) has an optimal balance of coagulation and anticoagulation systems. But in some situations the balance is disturbed, which leads to illness. There are 2 possible variants of thrombophilia during pregnancy:
- Congenital or genetic. The risk of blood clots is present in a person from birth and is caused by the presence of a genetic predisposition, that is, a special gene. Usually, disturbances in DNA structures do not appear until any serious stress occurs on the female body. Among them are pregnancy or dangerous diseases. In some situations, it is possible to identify the fact of genetic thrombophilia during pregnancy before symptoms appear, using a family history. This is when the medical history of close relatives contains thromboembolism, or cases of strokes and heart attacks, as a result of the formation of blood clots in the vessels.
- Acquired. The presence of the gene is not considered here. You can acquire a tendency to thrombophilia in the case of antiphospholipid syndrome or in various diseases that affect blood vessels. In the first case, the human immune system begins to produce special antibodies, which begin to actively destroy the cell walls of internal organs.
Doctors note that thrombophilia during pregnancy poses a great threat to the mother herself and her fetus. Therefore, it is recommended to first undergo testing and special treatment. This will allow you to get pregnant normally and bear a healthy child.
Risk factors
The mere presence of the gene does not guarantee that a woman will necessarily encounter manifestations of hereditary thrombophilia during pregnancy. Much depends on exposure to risk factors. The likelihood of the disease increases with:
- pregnancy aged 35 years and above;
- presence of obesity;
- diseases of the cardiovascular system and liver;
- chronic smoking 10 cigarettes a day or more;
- varicose veins;
- a large number of pregnancies;
- long-term diseases in a chronic form;
- prolonged stays in the same position;
- use of hormonal contraceptives;
- frequent headaches.
Regardless of the provoking factor, when exposed to any of them, the likelihood of complications developing during pregnancy increases significantly. If you identify the symptoms in a timely manner, make a correct diagnosis and prescribe adequate treatment, there is every chance of saving the fetus and avoiding serious consequences for the baby.
Possible consequences for the child
Mom's belly begins to gradually grow as the fetus develops inside it. But the process may be accompanied by negative changes caused by the manifestation of thrombophilia. Changes caused by the disease lead to vascular damage. The vessels leading to the placenta, through which the fetus receives all the necessary nutrition, are among the first to suffer. The formation of small blood clots in blood vessels can lead to serious and dangerous complications for the baby. The consequences appear as:
- habitual miscarriage;
- frozen pregnancy (FM);
- polyhydramnios or oligohydramnios;
- undeveloped pregnancy;
- small fruit;
- developmental delays;
- congenital malformations;
- premature birth;
- placental abruption, etc.
Missed pregnancy, developmental delays and other complications can negatively affect future health. Although there are also risks due to which a woman may simply lose her baby before his birth. Experts recommend that women come for examinations to check for the presence of genetic or acquired thrombophilia before pregnancy. Already pregnant mothers will be provided with additional support, which will allow them to fully bear the child and avoid negative consequences.
Diagnosis of thrombophilia
What tests should I take if I suspect thrombophilia?
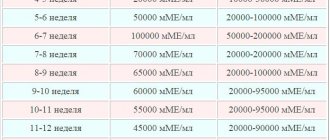
1. UAC. In a general blood test, we see the number of red blood cells, leukocytes and platelets, their sizes and parameters, and the erythrocyte sedimentation rate. All these indicators for thrombophilia may be within normal limits or indirectly indicate pathology.
2. Coagulogram. The parameters of INR, APTT, PTI, PTT, fibrinogen, D-dimer, RFMC, antithrombin III are studied.
We will tell you in more detail about each, so that you understand a little the meaning of the result given to you from the laboratory and are not scared in advance. But in any case, discuss the results with your doctor.
INR (international normalized ratio) is an index that shows the ratio of a patient's prothrombin time to the prothrombin time of a healthy person. The INR norm is from 0.7 to 1.3 (that is, about 1 unit on average).
PTT (prothrombin time) is the time it takes for a clot to form after adding a reagent (tissue factor obtained from animal blood) to a test tube containing the patient’s blood. PTV norms: 9 - 15 seconds.
PTI (prothrombin index) is the ratio of the PTI of control plasma to the PTI of the patient. Expressed as a percentage. The PTI norm is 85 - 110%.
APTT (activated partial thromboplastin time) is a specific blood test that shows the activity of the intrinsic clotting pathway. Calcium is removed from the blood, and then platelets are added, reagents are added, and the time of clot formation is measured. The normal APTT is 25 - 37 seconds.
Fibrinogen is one of the blood clotting factors. There should be 2 - 4 grams in 1 liter (g/l) in the blood. Normally, soluble fibrinogen is converted into insoluble fibrin in the event of vessel damage and bleeding, blood cells settle on the fibrin threads, and a blood clot forms (as artistically represented in the picture). Then, when the clot, having fulfilled its function, resolves, fibrin disintegrates (degrades).
D-dimer is a degradation product of fibrin. Normally, its content is not higher than 500 ng/ml. With increased coagulability, its content increases.
SFMC (soluble fibrin monomer complexes) is a marker of intravascular blood coagulation and microthrombi formation. Normally, this indicator is less than 4 in non-pregnant women and can be up to 9 in pregnant women.
Antithrombin III is a blood regulatory protein that controls the clotting process and prevents excessive blood clot formation. Normally, its content in pregnant women is 70 - 116%.
3. Specific study for thrombophilia.
We will give the names of the studies, but only a doctor (therapist or hematologist) should prescribe them. The cost of tests is very high, and it makes no sense to check everything “just in case.”
3.1. Genetic markers of thrombophilia:
- Plasminogen activator inhibitor - Methylene tetrahydrofolate reductase (MTHFR). Detection of mutations at various levels - Fibrinogen, beta polypeptide (FGB) - Blood clotting factor 13, subunit A1 - Blood clotting factor 7 (F7) - Blood clotting factor 5 (F5) - Blood clotting factor 2, prothrombin (F2). — Integrin beta-3 — Integrin alpha-2
The conclusion will also indicate the heterozygous or homozygous form of the mutation. A homozygous mutation means that the gene encoding the protein is completely damaged and therefore incorrect blood clotting proteins are synthesized. A homozygous mutation indicates inheritance of problems with blood clotting from both parents. A heterozygous mutation suggests that the polymorphism was inherited from one of the parents.
3.2 Resistance to activated protein C (resistance - APS) must be investigated.
3.3 Homocysteine has recently become increasingly important in the problems of miscarriage.
The more studied this indicator is, the more evidence there is of its involvement in obstetric problems.
In pregnant women, homocysteine should be in the range of 3.4-20.4 µmol/l.
Homocysteine itself is a normal participant in metabolism, but in the presence of a genetic mutation in the gene encoding the production of methylenetetrahydrofolate reductase (MTHFR), it is not converted into methionine and hyperhomocysteinemia gradually develops.
Briefly about thrombophilia
Thrombophilia is a disorder in the body that causes it to develop a tendency to form blood clots (blockages). The disease can be triggered by genetic failures or physiological failures. The disease manifests itself in different ways. Very often, it does not make itself felt at all, and in the event of injury, surgery, or pregnancy, dangerous health problems can arise due to this disorder.
There are several types of thrombophilia. It can be acquired or hereditary (congenital). Acquired occurs as a result of injuries and operations, and hereditary is transmitted to a person by inheritance or appears as a result of various mutations. In the latter case, doctors talk about disorders at the genetic level.
In addition to the above division of thrombophilia, depending on the causes of occurrence, there is another classification of the disease:
- Hematogenous thrombophilia. This type of it is the most dangerous, and especially for pregnant women. It can lead to disability or death.
- Vascular thrombophilia. This type includes atherosclerosis and vasculitis.
- Hemodynamic thrombophilia is associated with disorders in the circulatory system.
Preparing for pregnancy with thrombophilia
If you have diagnosed thrombophilia, especially with a homozygous mutation, you have to prepare for pregnancy in advance. As a rule, such patients have problems with conception and pregnancy, so adequate treatment should be selected in advance, thereby protecting both yourself and the unborn child.
Pregnancy is a genetically determined hypercoagulable state. The incidence of thromboembolic complications during pregnancy increases up to 6 times. This is necessary to stop bleeding during childbirth; the highest coagulability is observed in the third trimester, the body prepares for childbirth and blood loss.
To compensate for the condition and increase blood fluidity, the volume of circulating blood/plasma increases, but with thrombophilia this does not matter, since the pathological coagulation mechanism is triggered in plasma proteins, and not in blood cells.
— Consultation with a hematologist. In case of pregnancy due to thrombophilia, a hematologist is an equally important attending physician along with an obstetrician-gynecologist.
— Taking folic acid supplements.
The usual dose of folate in prenatal preparation is 400 mcg. In hypercoagulable states, folate doses are increased up to treatment with megadoses. This is especially true if hyperhomocysteinemia is detected.
Folic acid (vitamin B9) is one of the B vitamins whose properties have been carefully studied and its use has recently expanded.
Folic acid (in the form in which it is sold in tablets) is not absorbed by everyone. The ratio of those who absorb this vitamin and those whose bodies are insensitive to it is approximately the same. To check this, expensive and hard-to-find tests are needed. Currently, drugs are being produced that contain metafolin. Metafolin is an accessible form of folic acid that is absorbed by almost everyone, since its absorption does not require a long chemical process involving enzymes (as in the metabolism of regular folic acid).
It is recommended to start taking most folates 3 months before expected conception and continue until 12 weeks of pregnancy.
Folic acid in 1 mg tablets is the most common and affordable drug. Take 1 tablet per day or every other day under the supervision of a physician.
Folacin contains 5 mg of folic acid, this is a high dose and the drug is usually prescribed in preconception preparation for women with concomitant other pathologies (folate deficiency anemia, inflammatory bowel disease and malabsorption). Prescribed ½ tablet once a day 4 weeks before the expected conception and continues until 12 weeks of pregnancy.
Folio is a drug classified as a dietary supplement (biologically active food supplement) and containing 400 mcg of folic acid and iodine (potassium iodide) 200 mcg. Take 1 tablet per day.
“Folic acid 9 months” contains 400 mcg of folic acid in 1 tablet, take 1 tablet per day.
Femibion Natalcare I is a complex drug, also classified as a dietary supplement, containing folic acid 200 mcg and metafolin 200 mcg, as well as iodine, other B vitamins, calcium and vitamin E. The drug can also be taken
Angiovit is a complex vitamin preparation containing 5 mg of folic acid, as well as vitamins B6 and B12. The drug is prescribed only for treatment, as it contains large doses of vitamins. Take 1 tablet per day for 30 days or longer according to indications.
Positive effects of folic acid:
• Reduced homocysteine levels.
Hyperhomocysteinemia is associated with many pathological conditions, the root cause of which is damage to the internal lining of blood vessels and activation of thrombus formation. With thrombophilia, a small provoking injury is enough to trigger the hypercoagulation mechanism. It is not always possible to predict in which system the pathological process will occur, but vessels of small diameter, including the vessels of the placenta, are at greater risk.
Folic acid (and preferably in combination with other B vitamins) prevents the development of hyperhomocysteinemia. Folates, when included in metabolism, regulate the conversion of relatively toxic homocysteine into harmless cysteine.
• Prevention of neural tube defects of the fetus (the frequency of congenital malformations of the fetus associated with the formation of the nervous system, brain and spinal cord is significantly reduced).
• Prevention of certain types of anemia (folate deficiency) and normalization of hematopoietic processes.
• Strengthening immune defense (positive effect on the functioning of protective blood cells - lymphocytes).
• Reducing the risk of premature birth, premature rupture of membranes and the birth of premature babies.
• Normalization of the emotional background (since folic acid is involved in the process of transmitting nerve impulses, and is also involved in the metabolism of the stress hormone adrenaline) and prevention of postpartum depression.
• Participation in collagen synthesis, reducing the effect of skin photoaging.
- Progesterone preparations. Dydrogesterone (Duphaston) or natural progesterone (Utrozhestan or Prajisan) are used individually.
— Acetylsalicylic acid 75–100 mg per day (usually discontinued with the onset of pregnancy). It is better to use protected forms of enteric-coated aspirin: thromboAss, cardiomagnyl, aspirin-cardio, aspicor.
— Curantil (dipiradamol) 25–600 mg per day, as you can see, the doses vary dramatically in different patients, so only a specialist should select and adjust the dose.
- Preparations of low molecular weight heparins for severe disruption of the hemostatic system. Clexane (enoxparin sodium) is a low molecular weight heparin preparation, which is available in disposable syringes of 0.2, 04, 0.6, 0.8 and 1 ml. It is administered subcutaneously. The dosage, frequency of administration and duration of use are determined individually.
- Preparations of polyunsaturated fatty acids (Vitrum cardio omega - 3, Omegamama 9 months and others). Taking unsaturated fatty acids should be prescribed by a doctor; dosages are individual. An overdose is as harmful as a nutrient deficiency. Some drugs should not be combined with other vitamin complexes. PZhNK preparations have many positive properties, in the case of pregnancy against the background of thrombophilia it is important:
• Reduced platelet aggregation (the ability of platelets to form clots) - protection of the inner surface of blood vessels (any damage or formation, plaque promotes the deposition of platelets on them and activation of the thrombosis process).
• PUFAs are included in the synthesis of active metabolites (anti-inflammatory substances) and thereby reduce the likelihood of premature birth
• Reduce blood pressure by reducing the production of stress hormones (adrenaline, norepinephrine), and by lowering blood pressure, the risk of premature abruption of a normally located placenta is reduced.
— Wessel due f. This is a relatively new drug whose active ingredient is sulodexide. It has analogues, but the analogues do not have data on the safety of use in pregnant women. It is a direct-acting anticoagulant, that is, it reduces the effect of thrombin in the blood and thereby counteracts coagulation.
The drug is available in solution and capsules. For outpatient use, capsules are recommended; the dosage and duration of use are determined by a hematologist. Wessel Due f is not prescribed in the first trimester, and is then used if the expected benefit to the mother is higher than the risk to the fetus. Discontinuation of the drug before childbirth is also under the supervision of a hematologist.
Note: sometimes a combination of drugs with a blood-thinning effect is used, but choosing combinations on your own is strictly contraindicated due to the risk of overdose and bleeding.
Management of pregnancy with thrombophilia
Treatment of thrombophilia during pregnancy involves continuing to take progesterone drugs (doses may vary during pregnancy, different drugs have their own duration of administration) and folate.
— Anticoagulant therapy. During pregnancy, the administration of low molecular weight heparins in various dosages continues. The administration is carried out against the background of regular monitoring of hemostasis indicators. As a rule, the entire range of coagulogram results is initially determined, and then control is carried out based on the level of D - dimer. Periodically, heparins can be discontinued and then taken again. 2 weeks before birth, all anticoagulants should be discontinued.
— Magnesium and B6 preparations. Magne B6 – forte or Magnelis B6, 1 tablet 2 times a day, duration from 1 month, and then under the supervision of your doctor.
— Observation by a hematologist.
— Monitoring the condition of the fetus. Monitoring the condition of the fetus is carried out using standard methods: ultrasound with Dopplerometry from early stages, cardiotocography (CTG) in the third trimester.
In the first trimester, up to 8-10 weeks, it is advisable to undergo three-dimensional echography of the uteroplacental blood flow. Based on the results of this study, reliable conclusions can be drawn about the state of blood flow and the prospects for pregnancy. Unfortunately, the study is not available everywhere.
What to do in case of hemostasis disorders?
A blood clotting disorder is not a death sentence, but a problem that requires correction with special medications. Correction is especially important when planning pregnancy and pregnancy. Miscarriage and infertility are often accompanied by a tendency to increased thrombus formation.
Among women resorting to IVF, this tendency is more common, so the procedure is carried out under the control of hemostasis. Women in the program are often prescribed anti-clotting medications. Of these, the safest and most effective during pregnancy are heparins, which increase the chances of successful delivery after in vitro fertilization by 1.5-2.5 times if used in the early period of gestation.
Drugs and dosage are selected individually, and therapy is carried out under laboratory control, since it is difficult to predict how the drugs will work in each case.
Complications of maternal thrombophilia for the child:
— Frozen pregnancy at short term. This occurs due to a critical disruption of blood flow in the chorionic vessels. The resulting microthrombi clog the vessels and sharply disrupt the nutrition of the embryo, which leads to its death in the earliest stages.
- Spontaneous termination of pregnancy.
- Premature birth.
- Antenatal fetal death.
All of the above conditions are caused by manifestations of hypoxia (acute or decompensation of chronic fetal hypoxia). Constant lack of blood supply to the placenta leads to its cicatricial transformation, placental infarctions and, ultimately, the formation of chronic fetoplacental insufficiency.
— Placental abruption.
The formation of microthrombi in the vessels of the placenta also plays a role here. Usually in this case the situation is complicated by hypertensive disorders in the mother (preeclampsia, gestational arterial hypertension, chronic arterial hypertension).
The occurrence of thrombophilia
If a person has undergone any surgery or been injured, acquired thrombophilia may begin to develop. Genetic thrombophilia is passed from parents to children. There are cases when pathology occurs as a result of a mutation. Genetic thrombophilia cannot be detected in the body because there are no symptoms. Certain symptoms begin to appear when fractures, injuries occur, or when a woman becomes pregnant.
Why does pregnancy provoke the development of pathology? As it turns out, circulatory disorders and bearing a child are strongly interconnected.
Blood clotting increases in the body from the moment of conception. This is how the body reacts to pregnancy so that during childbirth the woman does not die from blood loss. However, there is a negative side to this idea of nature, due to the fact that blood clotting is increased, blood vessels become clogged with clots, which in turn can lead to miscarriage or cause premature birth.
Genetic thrombophilia manifests itself most often during pregnancy. From the moment of conception, another circulatory system appears in a woman’s body – the placental. Of course, this creates additional stress on the body. The formation of a new circulatory system is a prerequisite for the development of genetic thrombophilia.
Congenital thrombophilia
Thrombophilia is not at all dangerous to humans, but changes occur from the moment of pregnancy. If a woman has signs of hereditary thrombophilia, then the likelihood of thrombosis increases significantly. The risk of miscarriage also increases. If a woman experiences symptoms of thrombophilia during pregnancy, she is likely to give birth prematurely. It should be noted that premature birth is a positive end to pregnancy, since in most cases thrombophilia leads to a frozen pregnancy.
The formation of blood clots in the vessels leads to oxygen starvation of the fetus, and its growth and development is suspended. If the child does not receive vital substances during pregnancy, this can lead to processes such as:
- placental abruption;
- development of pathologies in the fetus;
- death of a child;
- miscarriage;
- gestosis;
- premature birth;
- preeclampsia.
Complications for the mother:
— Thrombosis of various localizations. Most often, pregnant women experience thrombosis of the veins of the lower extremities and pulmonary embolism.
Vein thrombosis occurs more often in late pregnancy. The concern is sharp pain in the affected limb (the lesion is initially unilateral), swelling (the diameter of the limbs varies significantly), the limb may be red and hot to the touch. With deep vein thrombosis, the clinical picture is more blurred, mainly pain in the limb. With superficial vein thrombosis, the affected area can be visually determined.
Pulmonary embolism is a serious thromboembolic complication. The clinic consists of complaints of pressing or other pain in the chest/epigastric region, severe shortness of breath, blueness of the lips, nasolabial triangle and nail phalanges of the fingers. The cause of pulmonary embolism is often thrombosis of the deep veins of the legs.
In the case of thromboembolism of small branches of the pulmonary artery, the prognosis is more favorable; with rapid initiation of therapy, it is possible to stop the clinical manifestations and save the patient. With massive pulmonary embolism, the mortality rate is very high and the prognosis is extremely unfavorable.
Other localizations of thrombosis are less common: ischemic stroke, thrombosis of the central artery and/or central vein of the retina, infarction, thrombosis of the hepatic veins, mesenteric thrombosis (thrombosis of the vessels of the mesentery of the small and/or large intestine).
- Preeclampsia.
Symptoms
Symptoms may not appear for a long time and because of this it is difficult to cure the severe form into which the pathology develops.
In pregnant women, the signs are brighter, because when the third circle of blood circulation appears, the load increases sharply and the body cannot cope.
Main features:
- Pain at the site of thrombosis.
- Discomfort when exhaling.
- Sensation disappears from the limbs.
- Pulse is rapid.
- Constant fatigue and apathy.
- Chronic headaches.
- Slow reaction to what is happening around.
Many women perceive these symptoms as simple satellites of gestation, although there is a great danger behind this.
If there are suspicious signs, you need to be tested for hereditary thrombophilia and tested for the genetic type of the disease.
Childbirth with thrombophilia
Childbirth with thrombophilia is a very controversial issue. There are recommendations for delivery at 37 - 38 weeks, and there are recommendations closer to the expected date of birth.
Childbirth through the birth canal is NOT contraindicated if the hemostatic system is fully compensated, ultrasound, Doppler and CTG of the fetus are normal, the woman’s condition is satisfactory and there are no other factors (scar on the uterus after a previous cesarean section or myomectomy, hypertension, etc.).
Pain relief during childbirth is preferably intravenous (narcotic analgesics, for example, promedol). However, epidural anesthesia is sometimes performed. The decision to perform epidural anesthesia is made by an anesthesiologist-resuscitator, based on the data of a coagulogram and a general blood test (platelets). It is also important what treatment regimen the pregnancy was followed. If hemostasis is unstable, combined treatment has a high risk of hemorrhage and epidural anesthesia is not recommended.
Caesarean section is performed according to cumulative indications. Indications are formed closer to full-term pregnancy, but most often not earlier than 36 - 37 weeks. Cancellation of anticoagulants is carried out on the recommendation of a hematologist.
Diagnostic methods
One of the main methods for diagnosing the disease is a blood test, which is examined in several stages:
- The first is screening . Its main goal is to detect pathologies in a certain link of the coagulation system.
- The second stage is a specific analysis for thrombophilia during pregnancy.
Screening tests can detect the following forms of thrombophilia:
- An increase in blood viscosity and an increase in hemocrit indicates a hemorheological form of thrombophilia.
- An increase in platelet aggregation ability indicates the presence of thrombophilia caused by impaired hemostasis.
- Determining the level of antithrombin will indicate the lack of primary anticoagulants.
- The “cuff test” will allow us to judge thrombophilia caused by a violation of the fibrinolysis system.
- The presence of lupus anticoagulant is a sign of autoimmune tombophilia.
If a pregnant woman has the following indicators, it is worth thinking about the development of thrombophilia and its possible consequences - polycythemia, erythrocytosis, decreased ESR, isolated hyperthrombocytosis, increased hematocrit.
Moreover, changes in the shape and size of red blood cells can cause thrombosis.
An indicator of an urgent examination for the detection of thrombophilia during pregnancy is congenital thrombophilia in close relatives, retardation in fetal development or repeated miscarriages, and the presence of symptoms of purpura in the newborn.
Thrombophilia in the postpartum period
Thrombophilia does not go away after childbirth, but now only the mother is at risk of complications. The baby no longer participates in a common metabolism with the mother and is less dependent on her.
A postpartum woman needs control of hemostasis, as she has many risk factors for thrombosis:
- Immobilization. Some mothers believe that it is better to take care and, especially after a cesarean section, do not get out of bed for days. When physical activity resumes, there is a high risk of small blood clots spreading through the vessels. The most dangerous case of thrombosis is PE. In fact, activation as early as possible after childbirth, surgery or injury is the most effective prevention of many complications. This takes into account not only thromboembolic complications, but also hypotonic conditions of the intestine with intestinal obstruction, infectious complications, etc.
- Hemodynamic changes. Changes in blood pressure are always associated with vascular tone. In the presence of small blood clots, changes in vascular tone can contribute to their spread throughout the body.
- Blood loss. Blood loss stimulates the body to take protective actions aimed at stopping bleeding. Excessive activity of the coagulation system in thrombophilia promotes thrombosis.
Treatment of thrombophilia after childbirth
After birth, the administration of low molecular weight heparins continues for 2–6 weeks. During the first days after birth, the previous doses continue to be administered if there were no obstetric complications during childbirth (hypotonic bleeding, placental abruption and others associated with blood loss). Further, the doses of heparins are regulated by a hematologist.
After completion of heparin therapy, antiplatelet agents (chimes, aspirins) or tablet anticoagulants (Wessel Due F) can be continued.
Is it possible to breastfeed?
Breastfeeding should be discontinued during Clexane therapy as the amounts in which the drug is excreted in breast milk are unknown. There is a risk of causing bleeding in the baby.
If you plan to breastfeed after treatment with Clexane, then actively pump and gently massage the mammary glands to maintain lactation.
If after childbirth the use of tableted anticoagulants and antiplatelet agents is indicated, then breastfeeding should be stopped.
Forecast
If you know about your diagnosis, the prognosis for childbirth and life in general is quite favorable. The high detection rate of thrombophilias at present is the result of diagnostic advances, and not at all a newly acquired disease of the 21st century. And using advances in pharmacology, we can minimize all the risks associated with thrombophilia.
As we see, even in the presence of such unusual conditions as thrombophilia, it is possible to select preparation regimens for pregnancy and treatment during pregnancy in order to reduce all risks to a minimum. You are required to be responsible and desire to have a healthy baby, as well as take care of your own health. Take care of yourself and be healthy!
Doctor Petrova A.V.
Treatment
Pregnancy and thrombophilia are not incompatible concepts, but the disease must be treated regardless of the gestation period.
After diagnosis, doctors immediately prescribe treatment. The scheme is approved by a geneticist, gynecologist and hematologist.
Treatment consists of:
- drug therapy;
- diets;
- compliance with the regime.
To reduce blood clotting, a woman needs to take anticoagulants. Dosage and medication are individual for each patient.
The diet involves eating foods that reduce blood clotting. These are seafood, ginger root, dried fruits and berries. The following should be excluded from the diet:
- buckwheat;
- greenery;
- white cabbage, red pepper, beets, turnips, radishes, legumes;
- walnuts;
- bananas and mangoes;
- rose hips, rowan berries;
- offal (liver, heart, kidneys);
- fats of animal origin.
Slow walking is beneficial for a woman, but prolonged sitting or standing in one place will only worsen the condition. Physical therapy and swimming are useful. With your doctor's permission, you can wear compression garments.