What is a saddle uterus? The irregular structure of the female genital organs is increasingly worrying the fair sex. After all, many anomalies in their development prevent a “healthy” conception and carrying a full term pregnancy. For example, one of these irregular organ structures is the saddle-shaped uterus. This irregularly shaped organ can darken the course of pregnancy and negatively affect the condition and development of the embryo. In addition, the saddle shape of the uterus can significantly complicate a woman’s labor. So, is the saddle uterus and pregnancy compatible, as well as the reasons for its occurrence in women.
What does saddle uterus mean? Fortunately, such a diagnosis is now extremely rare. In terms of its form, it is considered the second most common after the normal structure of the genital organ. After it comes the bicornuate uterus, which also brings many health problems. It is important to note that the saddle uterus is often accompanied by other anomalies of the genital organs, so a woman should undergo a full examination of the entire reproductive system in order to know exactly about all the problems in the body.
The uterus, whose shape is saddle-shaped, in appearance practically “merges” with a bicornuate organ. This means that a small recess has formed at its bottom, which in appearance resembles a saddle. In other words, this organ looks like a heart with sharp edges, although normally it should resemble a pear. Today, doctors count 23% of women with a saddle uterus, and most of them are unable to become pregnant. Typically, this form of organ does not cause any symptoms and does not in any way affect the patient’s well-being. In addition, this pathology cannot be diagnosed independently; this can only be done with ultrasound or other modern procedures.
With a strong change in the shape of this reproductive organ, a woman notices the development of some symptoms and signs, which include:
- infertility – a woman is unable to become pregnant for a long time (in this case, even modern medications and vitamins cannot help conception);
- acyclic bleeding, which becomes noticeable as menstruation begins;
- pain during sexual intercourse, which doctors associate with insufficient blood circulation to the organ, as well as severe stretching of its base;
- premature birth, which is accompanied by complications (those who gave birth with a saddle uterus claim that they had certain complications, which often led to a caesarean section);
- the origin of miscarriage at any stage of pregnancy.
This form of the uterus during pregnancy, as well as before conception, is often detected with disorders and anomalies in the development of organs related to the urinary system. Also, the presence of these complications leads to the appearance of a septum in the reproductive organ, which is often caused by a narrow pelvis in a woman.
Therefore, a saddle-shaped uterus and pregnancy can cause serious complications for a woman during pregnancy, as well as lead to the development of injuries during labor.
Is it possible to get pregnant with this pathology? Doctors say that half of women with this disease are considered completely infertile - in this case, even modern treatment and restoration of the normal shape of the organ will not help such patients.
Unfortunately, the saddle-shaped and bicornuate uterus are considered congenital pathologies - in other words, girls are already born with these anomalies. There are many reasons for the development of this phenomenon, however, the main one is the effect of destructive and negative factors on the health of the mother, which negatively affect the general condition of the embryo.
According to doctors, the saddle uterus has the following causes:
- unfavorable heredity in a woman, which is directly related to the development of genetic problems;
- the use of certain drugs during pregnancy that have a negative effect on the condition of the unborn baby;
- the presence of bad habits that a woman “used” during pregnancy: these include smoking, drinking alcoholic beverages, drug addiction, and so on;
- gestosis;
- severe toxicosis;
- development of fetal hypoxia;
- heart defects in women;
- frequent stress during pregnancy;
- working or living conditions unfavorable for a woman’s health;
- transmission of severe viral or bacterial infections during pregnancy;
- lack of vitamins in the body.
All this can develop problems in a child that will negatively affect his life. Therefore, the main condition for a pregnant woman is to monitor her health status, not worry, timely treatment of diseases, and also follow all doctors’ recommendations.
In addition, this deviation is also possible when suffering from certain diseases before the upcoming birth or occurring during gestation. These include diabetes mellitus, frequent disorders that negatively affect the nervous system, endocrine pathologies, the course of vegetative-vascular dystonia, and so on.
Such pathologies can have a detrimental effect on women’s health, as well as negatively affect the developing embryo, which can lead to disruption of the structure of the genital organs.
Before starting treatment, it is necessary to carry out a diagnosis, as well as understand what it means when making a diagnosis. For many years, a woman may not even be aware that she has problems with the genital organs, since they most often do not make themselves felt and are not expressed in symptoms unfavorable to health. Often, representatives of the fair sex find out about the abnormal shape of the reproductive organ only when they become pregnant. Although, before becoming pregnant, any woman should visit a gynecologist to check her health and, if necessary, correct it. After all, not every pregnant woman can boast that she gave birth without complications in the presence of a saddle-shaped uterus.
The saddle uterus and childbirth are often not compatible with each other, since during the onset of labor the pregnant woman may experience serious health problems that can lead to the death of the baby. That is why today childbirth with a saddle uterus is not very common.
Doctors prescribe treatment for pregnant women, with the help of which they can avoid complications and also not encounter them while carrying a child.
It should be noted that it is not always possible for a woman with this form of genital organ to become pregnant easily and quickly, since with a saddle-shaped uterus it is quite difficult for the embryo to penetrate its mucous layer.
To avoid this, it is necessary to carry out a diagnosis before the planned conception, which will tell everything about the condition of the genital organs. It is possible to notice the presence of a saddle uterus in a woman using an ultrasound, which uses a vaginal sensor to assess the condition of the genital organ.
In addition, the doctor may prescribe the following procedures:
- UZGSS;
- hysteroscopy.
The doctor will tell you what each procedure means. In addition, he will explain why a woman should undergo each or one of these diagnostic methods. It is important to note that an examination on a chair is not able to identify this pathology, so a woman should not refuse these diagnostic methods and be sure to carry them out, because not only the condition of the patient herself, but also her unborn child depends on this.
The uterus is precisely the organ in the woman’s reproductive system in which the birth of a new life occurs. Therefore, it is so important that she does not have any pathologies or illnesses. But what if the shape of the uterus has undergone changes?
More likely causes of a saddle uterus, suggested by medicine:
- Hereditary predisposition to mutation of genes responsible for the formation of organs.
- Taking certain medications.
- Abuse by the mother, and other bad habits.
- Stress experienced during pregnancy.
- Heart defect in the expectant mother.
- Past viral and infectious diseases during pregnancy.
- Excessive toxic manifestations during gestation.
- Lack of proteins involved in the normal formation of the fetus.
Diseases that the mother has before and throughout pregnancy also play an important role. These include heart failure, disorders, improper functioning of the endocrine system, vegetative-vascular dystonia and others.
The environmental factor should not be excluded. Quite often, women living in cities with environmental problems give birth to children with one or another health-related pathology.
Also, disruption of the uterus, as well as other organs, may be due to long-term oxygen starvation of the baby in the womb. Asphyxia in the fetus can be caused by a sedentary lifestyle, decreased activity in the first half of pregnancy, poor functioning of the circulatory system, and impaired placental circulation.
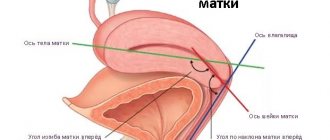
Structure of the uterus
The uterus of an adult woman has an ovoid shape. Women who have not given birth have a pear-shaped uterus. The structure of the organ can be divided into several parts.
- The fundus is the upper part, protruding above the line of confluence of the fallopian tubes.
- The body is the middle, largest part of the organ.
- The isthmus is the junction of the uterine body and the cervix.
- The neck is the lower part. It is divided into two sections: supravaginal and vaginal.
The organ has two surfaces:
- anterior (vesical): located next to the bladder;
- posterior (intestinal): adjacent to the rectum.
The uterus is supported by the ligamentous apparatus, which includes:
- round ligament;
- own ligament of the ovary;
- broad ligament;
- cardinal ligament (paired).
The weight and size of the uterus may vary from woman to woman. On average, the weight is 40 g (for nulliparous women) -100 g (for those who have given birth). The average length is 5.5 cm, and the width is 3.5-4 cm; in women who have given birth, these sizes increase. The volume of the uterine cavity is 5 cm3. During pregnancy, the size of the organ increases significantly.
The thickness of the uterine wall is 1 cm. It consists of three components.
- The endometrium (mucous membrane) lines the inside of the uterine cavity. The endometrium consists of two layers. Functional (superficial) - during menstruation it is almost completely rejected. Basal (located deep): its function is to restore the functional layer.
- The myometrium (muscular membrane) consists of three layers. External: muscle fibers are predominantly located longitudinally and obliquely. Medium: muscle fibers are arranged circularly. This layer is most developed in the cervical area. Otherwise, it is called the vascular zone, due to the location of large blood vessels in it. Internal: the arrangement of muscle fibers is the same as in the outer layer.
- Parametrium (serous membrane) is part of the pelvic tissue.
What size and shape does a normal uterus have?
The uterus is the organ in which the female egg is implanted after fertilization. It is the uterus that becomes the “house” in which the baby lives, develops and grows stronger for 9 months.
The uterus is a muscular organ of the female reproductive system, located in the pelvis between the bladder and rectum. The length of this organ is about 7-8 cm, width - 4-6 cm. The weight of the uterus is on average 60 grams.
The uterus consists of a body (the upper pear-shaped part) and a cervix (the junction of the “pear” with the vagina). The fallopian tubes extend to the sides of the uterus and connect it to the ovaries. The uterus may move backward if the bladder is full, or forward if the rectum is full. During pregnancy, when the uterus grows, it leaves the pelvis and rises upward.
The uterus is formed in a female fetus already at 10-14 weeks of intrauterine development. During this period, the Müllerian ducts (two identical halves) “merge” in the future girl. After fusion, two utero-vaginal cavities are formed, which are separated from each other by a septum. Later, normally, this septum disappears, and the uterus takes on its usual appearance, that is, it becomes single-cavity.
Pear shape
Most women of reproductive age have a round – ovoid uterus. The pear shape is typical for girls. The normal shape allows the fertilized egg to fully consolidate and develop. But in 20% of cases the shape may differ. Among the pathological varieties of the shape of the uterus, there are saddle-shaped, bicornuate, and with a septum.
Norm or pathology
A pear-shaped uterus is normal in childhood and adolescence. By the time a woman reaches puberty, she takes on an ovoid shape.
Classification of pathology
The bicornuate uterus can be of three types:
- incomplete
- full
- saddle
Saddle-shaped is a shape of an organ in which there is an expansion in the cross section, and at the bottom there is a depression, which is shaped like a saddle. The two horns of the organ are not very pronounced; they merge, without capturing the bottom of the organ.
The normal shape of the uterus (without pathologies) is designed by nature. It is ideal for carrying a fetus for 9 months. It is worth knowing that some animals, including dogs, have a bicornuate uterus.
Possible risks
If the shape of a woman’s uterus is not pear-shaped, but saddle-shaped or bicornuate, then this threatens the woman with problems conceiving and bearing a child. Doctors who have encountered anomalies in their practice provide data on the possibility of a normal onset and course of pregnancy in 50% of cases.
The most common problems that may arise in a woman who does not have a pyriform uterus are:
- abnormal placentation;
- pathological presentation of the fetus;
- threat of premature placental abruption;
- risk of premature birth;
- pathologies of labor;
- the occurrence of obstetric bleeding.
Incorrect placentation
A pregnant woman with an abnormal uterine shape (not pear-shaped), due to the specific structure of the organ, has a high risk of developing placenta previa.
- Incomplete: the placenta partially covers the internal os.
- Complete: the placenta completely covers the internal os.
- The placenta does not cover the internal uterine os, but is located too low.
For a woman with an abnormal and non-pyriform uterus, abnormal placentation is at risk of developing complications:
- Bleeding: may occur and be a concern several times throughout pregnancy. The cause is premature placental abruption. It develops due to an increase in the size of the organ and insufficient elasticity of the placental tissue. Premature detachment threatens miscarriage. A feature of bleeding with abnormal placenta previa is the absence of pain;
- fetal hypoxia: the detached area of the placenta stops supplying the fetus with oxygen and other nutrients;
- decreased blood pressure in women;
- delayed fetal development;
- Iron-deficiency anemia.
The abnormal location of the placenta in the bicornuate form is due to the attachment of the egg in an abnormal place. In the pyriform organ, the embryo is able to fully attach.
Malpresentation
Often with a bicornuate form, the growing fetus is located incorrectly in it. This anomaly in the structure of the organ is most characterized by a transverse position and breech presentation. Unlike abnormal forms, pyriform provides longitudinal presentation.
The transverse position is characterized by the fact that the fetus lies across the pelvis. In this case, delivery is possible only by caesarean section.
With a breech presentation, the baby is positioned towards the exit of the uterus with its pelvic end. Theoretically, with proper obstetric care, natural childbirth with this pathology is possible. But, since the bicornuate form can cause discoordination of labor and weakness of labor forces, in most cases the woman is given a surgical delivery. The final decision is made by the doctor delivering the baby, guided by the characteristics of the individual patient.
Reviews from women about how pregnancy proceeded with a saddle uterus
Christina:
“A friend was diagnosed with a saddle uterus; she could not get pregnant for a long time, and when this happened, the doctor immediately warned that there might be problems. She set herself up for a good result, and in the end, at the 7th month, they decided to have a cesarean section, since the uterus was not growing any further. The girl was born prematurely, but healthy, and there were no abnormalities.”
Lyalka:
“I never had any examinations of my uterus, so I didn’t know that I had a saddle uterus. The doctor said that there is no danger, it’s just not the same shape as everyone else’s, but there may be difficulties with pregnancy. As a result, I became pregnant two months after the start of our attempts, I went to the hospital every week, and at the 7th month I had to go to the hospital. At the same time, there was no pain or discomfort, the doctor just had to constantly monitor me. “I gave birth on time, by Caesarean, but after that there were no problems, and everything is fine with the child.”
Natalia:
“Already at 10 weeks of pregnancy, I was diagnosed with a saddle uterus, although initially the doctor thought it was an ectopic pregnancy. I immediately got scared and started to get nervous, I thought that I would have to have an abortion. But then I read the reviews and realized that pregnancy with such a diagnosis is possible, and they even give birth on their own, so I calmed down a little. I found out everything from the doctor, she advised me to still choose a cesarean section, because giving birth on my own is dangerous. But from the 6th month I will have to constantly go to the hospital to be monitored. It doesn’t matter, I’ll endure everything, the main thing is that everything is fine with the baby.”
Elena:
“When I learned from my mother that she had a saddle uterus, I decided to go for an examination. I was also diagnosed with this pathology, I was upset, although my mother gave birth to two, and everything is fine. The doctor simply warned that there may be problems with pregnancy and childbirth, but this is all individual. I decided to find out everything about this diagnosis, and found a photo of a saddle-shaped uterus, it can be seen that it is slightly curved and not the same shape as a regular one. But most women still get pregnant and give birth, even on their own. So I calmed down and just waited for the pregnancy, I can handle it with the help of doctors. Moreover, I have a clear example - my mother: both the pregnancies were normal and she gave birth to two daughters without problems.”
Diagnosis and feasibility of correction
An abnormally shaped uterus can be diagnosed using the following methods:
Type of diagnostic test
The study is carried out during the luteal phase of the menstrual cycle using a vaginal sensor. During this period, the endometrium reaches its greatest thickness. Ultrasound is not a reliable basis for making an accurate diagnosis.
After introducing an X-ray contrast agent into the uterine cavity, several photographs are taken, from which the shape can be assessed: is it pear-shaped or abnormal. The main symptom of the pathology is the presence of a specific depression protruding into the uterine cavity.
MRI of the pelvis
By introducing a special optical device into the uterine cavity, a specialist assesses the condition of the internal genital organs and possible developmental anomalies.
The examination is performed under general anesthesia using a hysteroscope. The goal is to examine the uterine cavity. If necessary, simple surgical intervention can be performed.
The advisability of surgical intervention is determined by the attending physician in each specific case.
Correction of the abnormal shape is carried out strictly according to indications:
- Long-term impossibility of pregnancy.
- Habitual miscarriage.
Plastic surgery involves complete reconstruction of an organ. It is not possible to completely recreate the pear-shaped shape, however, it is possible to correct the defect using modern methods, and the woman gets the opportunity to become pregnant and bear the baby on her own. Surgery is performed using hysteroscopy. This method is characterized by low invasiveness and high efficiency.
If the uterus is not pear-shaped, a woman may have obstacles to implantation of the embryo in the uterine cavity. Ectopic pregnancy often develops.
If necessary, timely and high-quality reconstruction of the organ gives the woman a chance for a normal pregnancy.
Some people are diagnosed with malformations of internal organs. Most often, genital pathologies such as a pyriform uterus are detected.
Diagnostics
It is possible to establish a diagnosis of a saddle uterus and the difficulties associated with this pathology only after conducting the necessary studies.
A standard examination by a gynecologist with the mandatory collection of a family history on the female side will help to suspect the possible likelihood of a woman having this pathology. It is immediately worth noting that it is impossible to diagnose a saddle uterus with a routine visual examination.
If, after collecting a family history, it turns out that the patient has a possibility of a uterine mutation, she is referred for a transvaginal ultrasound examination of the reproductive organs. With the help of such an ultrasound, you can easily establish the clarity of the contours of the uterus and identify the type of deformation. After diagnosing uterine pathology, the condition of the kidneys and ureters should also be examined, especially if the woman suffers from.
Often women with a saddle-shaped uterus cannot become pregnant. Therefore, after establishing the diagnosis, she needs to undergo a study assessing the patency of the fallopian tubes - x-ray hysterosalpingoscopy. This is done with a special contrast that is injected into the reproductive system, and with the help of an X-ray machine or ultrasound sensor, the exact shape of the organ, the presence of adhesions and the condition of the tubes are recorded.
Sometimes, in order to more accurately examine the condition of the uterine cavity, the doctor prescribes hysteroscopy.
This method allows you to examine the organ from the inside, displaying clear images on the monitor screen.
But such a procedure has a number of contraindications that prevent it from being carried out:
- bleeding
- oncology of the uterus
- infectious diseases accompanied by poor health
- narrow cervical canal - stenosis
- inflammatory process in the reproductive system
If after all the studies you still have doubts about the diagnosis, you can undergo an MRI or CT scan.
These diagnostic methods create a three-dimensional picture of the organs of the reproductive system, and establish a diagnosis with 100% accuracy.
What does this mean?
Approximately 22% of women aged 18-35 have a pear-shaped uterus. The main parameters are presented in the table.
| Form | Pear-shaped. The wide part is turned upward. |
| Top part | Referred to as the "bottom". |
| Bottom part | Also called the isthmus, it ends at the uterine cervix. Communication with the vagina occurs using a special rope. |
| Length | 7-8 centimeters. |
| Width | 4-5 centimeters. |
| Weight | 50-60 grams |
What does it mean? A pear-shaped organ cannot be completely called a pathology. This form was laid down by nature. The main purpose is to bear only 1 fetus.
Should you worry?
Is it good when the uterus is pear-shaped, or is there any point in sounding the alarm? According to doctors, this structure of the organ means that a woman may have problems conceiving.
The main threat is the risk of miscarriage.
Other threats include:
- Incorrect placentation.
- Risk of malpresentation.
- Threat of premature placental abruption.
- Risk of premature delivery.
- The presence of an anomaly of generic forces.
- The occurrence of bleeding.
In approximately 50% of cases, pregnancy in women with a pyriform uterus is successful.
Incorrect placentation
This definition means placental presentation or its low location. The organ has a specific shape, so the risk of miscarriage, as well as incorrect placentation, is caused by the attachment of the egg in an inconvenient place.
Risk of malpresentation
As the gestational age increases, fetal malposition occurs. It can be pelvic or transverse. This leads to the risk of premature placental abruption. The result of this is bleeding.
Other risks
If the pregnancy is delivered prematurely, the technology for transmitting nerve impulses during contractions may be disrupted.
This can lead to both incoordination and weakness of labor. As a result, the doctor resorts to a caesarean section.
The risk of bleeding is explained by the fact that the contractile activity of the organ is disrupted.
Causes
Unfortunately, the saddle-shaped and bicornuate uterus are considered congenital pathologies - in other words, girls are already born with these anomalies. There are many reasons for the development of this phenomenon, however, the main one is the effect of destructive and negative factors on the health of the mother, which negatively affect the general condition of the embryo.
According to doctors, the saddle uterus has the following causes:
- unfavorable heredity in a woman, which is directly related to the development of genetic problems;
- the use of certain drugs during pregnancy that have a negative effect on the condition of the unborn baby;
- the presence of bad habits that a woman “used” during pregnancy: these include smoking, drinking alcoholic beverages, drug addiction, and so on;
- gestosis;
- severe toxicosis;
- development of fetal hypoxia;
- heart defects in women;
- frequent stress during pregnancy;
- working or living conditions unfavorable for a woman’s health;
- transmission of severe viral or bacterial infections during pregnancy;
- lack of vitamins in the body.
All this can develop problems in a child that will negatively affect his life. Therefore, the main condition for a pregnant woman is to monitor her health status, not worry, timely treatment of diseases, and also follow all doctors’ recommendations.
In addition, this deviation is also possible when suffering from certain diseases before the upcoming birth or occurring during gestation. These include diabetes mellitus, frequent disorders that negatively affect the nervous system, endocrine pathologies, the course of vegetative-vascular dystonia, and so on.
Such pathologies can have a detrimental effect on women’s health, as well as negatively affect the developing embryo, which can lead to disruption of the structure of the genital organs.
How is this detected?
A pear-shaped uterus looks like this:
The appropriate diagnosis is made after passing:
- ultrasound examination of the uterus;
- ultrasound examination of the appendages;
- hysterography;
- MRI;
- hysteroscopy.
Ultrasound is not an accurate diagnostic method.
The doctor may use a vaginal probe. The study is carried out in the second half of the cycle. At this time, the endometrium is very thick.
Hysterography refers to x-ray studies. A contrast agent is injected into the uterus. Then the specialist takes several pictures.
The main symptom of pear shape should be considered the presence of a specific depression. It is secreted into the uterine cavity.
An MRI takes several pictures of the internal genital organs. During hysteroscopy, an optical device is inserted into the uterine cavity. This helps the specialist examine the organ and identify an abnormality.
Norm and deviations
The uterus is shaped like a pear. The upper part is called the bottom, and the one below smoothly extends into the cervix, and then there is the vagina. It is in this way (from the vagina to the uterus) that pathogenic bacteria and sperm enter during unprotected sexual intercourse.
The uterus is usually from 7 to 8 cm in length, and from 4 to 5 cm in width. Its normal weight ranges from 50 to 60 grams. The uterus has tubes, which in medical language are called fallopian. They have fimbriae at the ends (they look like small brushes). The fimbriae can oscillate, which helps the mature egg after ovulation enter the fallopian tube and connect with sperm, if any.
Anomalies of organ development can be of any kind. Moreover, in some cases, deviations in the form and functions of other internal genital organs are noted. The uterus can be one-horned, two-horned, double, etc. One of the forms of a bicornuate uterus is saddle-shaped.
Anatomy [edit | edit code ]
Parts of the uterus [edit | edit code ]
The uterus consists of the following parts:
- Fundus of the uterus
- This is the upper convex part of the uterus, protruding above the line where the fallopian tubes enter the uterus. - The body of the uterus
is the middle (larger) part of the organ, has a cone shape. - Cervix
- The lower, narrowed, rounded part of the uterus.
The lower part of the cervix protrudes into the vaginal cavity, therefore it is called the vaginal part
, and the upper part of the cervix, lying above the vagina, is called
the supravaginal part
. The vaginal part of the cervix bears the opening of the uterus, leading from the vagina into the canal of the cervix and continuing into its cavity. In nulliparous women, the opening of the uterus has a round or oval shape, and in women who have given birth, it has the shape of a transverse slit. The thick edges of the vaginal part of the cervix, limiting the external opening, are called lips - anterior and posterior. The posterior lip is thinner, the vaginal wall is attached to it higher than to the anterior lip.
Surfaces of the uterus [edit | edit code ]
The uterus has anterior and posterior surfaces. The anterior surface of the uterus, facing the bladder, is called the bladder
, and the back one, facing the rectum, is
intestinal
. The vesical and intestinal surfaces of the uterus are separated from each other by the right and left edges, to which the fallopian tubes approach at the junction of the body with the fundus. The upper corners of the uterine cavity narrow into funnel-shaped depressions into which the uterine openings of the tubes open.
The structure of the uterine wall [edit | edit code ]
The wall of the uterus consists of three layers:
- Perimetry
(
Serous membrane
) - is a direct continuation of the serous cover of the bladder. Over a large area of the anterior and posterior surfaces and fundus of the uterus, it is tightly fused with the myometrium; At the border of the isthmus, the peritoneal cover is attached loosely. - Myometrium
(
Muscular membrane
) - the thickest layer of the uterine wall, consists of three layers of smooth muscle fibers with an admixture of fibrous connective tissue and elastic fibers;
- External longitudinal
(
subserosal
) - with longitudinally located fibers and in a small amount with circular ones, as was said, tightly fused with the serous cover.
Cervix [edit | edit code ]
This is a relatively narrow segment of the uterus, the wall of which consists primarily of dense collagen tissue and only a small amount of smooth muscle and elastic tissue. The cervical canal is flattened, and its mucous membrane consists of a tall columnar epithelium that produces mucus, and the connective tissue lamina propria, which is a fibrous connective tissue containing cells. On the front and back surfaces of the canal there are two longitudinal ridges and smaller palm-shaped folds extending from them at an acute angle. Contacting each other at the confluence of the canal, palm-shaped folds prevent the penetration of contents from the vagina into the uterine cavity. In addition to ridges and folds, the canal contains numerous branching tubular glands. The vaginal part of the cervix is covered with squamous non-keratinizing epithelium, which usually extends a short distance into the cervical canal, where it becomes the characteristic columnar epithelium. Thus, in mature girls and women, the border between the transition of columnar epithelium into flat non-keratinizing epithelium - the histological border - corresponds to the external os of the cervix. In girls under 21 years of age, the cylindrical epithelium can descend below the border of the external os and extend onto the vaginal part of the cervix, creating a picture of cervical erosion, so such a diagnosis is untenable in young people due to natural anatomical features.
Ligaments of the uterus [edit | edit code ]
Along the edges of the uterus, the sheets of peritoneum, covering its vesical and intestinal surfaces, come together and form the right and left broad ligaments of the uterus. The broad ligament of the uterus consists of two layers of peritoneum - anterior and posterior. The right and left broad ligaments of the uterus are directed to the lateral walls of the small pelvis, where they pass into the parietal layer of the peritoneum. In the free upper edge of the broad ligament of the uterus, between its layers, the fallopian tube is located. Somewhat below the attachment of the ovarian ligament to the uterus, the round ligament of the uterus originates from the anterolateral surface of the uterus. This ligament is a dense fibrous cord of round shape, 3-5 mm thick, containing muscle bundles and located between the leaves of the broad ligament of the uterus. The round ligament of the uterus is directed downward and anteriorly to the deep opening of the inguinal canal, passes through it and, in the form of separate fibrous bundles, is woven into the tissue of the labia majora, without touching the pubic symphysis. At the base of the broad ligaments of the uterus, between the uterus and the walls of the pelvis, lie bundles of fibrous fibers and muscle cells that form the cardinal ligaments of the uterus. With their lower edges, the cardinal ligaments of the uterus connect to the fascia of the urogenital diaphragm and keep the uterus from lateral displacement.
Vessels and nerves of the uterus [edit | edit code ]
The blood supply to the uterus occurs due to the paired uterine artery and branches of the internal iliac artery. Each uterine artery passes along the lateral edge of the uterus between the leaves of the broad ligament of the uterus, giving off branches to its anterior and posterior surfaces. Near the fundus of the uterus, the uterine artery divides into branches leading to the fallopian tube and ovary. Venous blood flows into the right and left uterine venous plexus, from which the uterine vein originates, as well as veins flowing into the ovarian, internal iliac veins and venous plexuses of the rectum.
Lymphatic vessels from the fundus of the uterus are directed to the lumbar lymph nodes, from the body and cervix to the internal iliac lymph nodes, as well as to the sacral and inguinal lymph nodes.
The uterus is innervated from the inferior hypogastric plexus along the pelvic splanchnic nerves.
Treatment
Therapy is relevant only for those who are faced with the problem of infertility caused by this particular pathology. They are reconstructing the organ. This is a plastic surgery that is done through hysteroscopy. This means that there will be no long anesthesia, and there will also be no large incisions (which will avoid unsightly scars on the body). After a correctly performed operation, the chances of conceiving a child increase many times over.
During gestation, women with a saddle-shaped uterus may experience obstetric complications. Treatment is individual. A woman should observe bed rest, that is, lie down and not lead an active lifestyle. The doctor selects drugs for the patient from a number of tocolytics and antispasmodics. Hormonal therapy is relevant, the drugs of choice are utrozhestan and duphaston.
To ensure that blood circulates normally in the uterus and in the vessels connecting the organ to the placenta, special medications are used. They affect blood clotting and normalize metabolic processes. These are the following medications:
- troxevasin
- Essentiale Forte
- chime
- Actovegin, etc.
Remember that for girls and women of any age, regular examinations by a gynecologist and passing the tests prescribed by him are important. By neglecting your own health today, you can develop a problem such as infertility. Take care of yourself and be healthy!
Pathologies [edit | edit code]
Developmental anomalies [ edit | edit code ]
- Aplasia (agenesis) of the uterus
- extremely rarely, the uterus may be completely absent. There may be a small infantile uterus, usually with a pronounced anterior incursion. - Duplication of the uterine body
is a defect in the development of the uterus, which is characterized by duplication of the uterus or its body, which occurs due to the incomplete fusion of two Müllerian ducts at the stage of early embryonic development. As a result, a woman with a double uterus may have one or two cervixes and one vagina. With complete nonfusion of these ducts, two uteruses with two cervixes and two vaginas develop. - Intrauterine septum
- incomplete fusion of the embryonic rudiments of the uterus in various variants, can lead to the presence of a septum in the uterus - a “bicornuate” uterus with a clearly visible sagittal depression at the bottom or a “saddle-shaped” uterus without a septum in the cavity, but with a notch at the bottom. With a bicornuate uterus, one of the horns may be very small, rudimentary, and sometimes unlaced. - Hypoplasia is underdevelopment of this organ in a woman. In this case, the uterus is smaller than it should be normally.
What is a saddle uterus?
The saddle uterus is a type of bicornuate uterus (their formation is based on similar reasons), and more precisely, it is an intermediate stage between normal and.
Saddle uterus is a congenital pathology in which a depression similar to a saddle forms in the fundus of the uterus. Hence the name. In general, such a uterus has the shape of a heart. The transverse size of the saddle uterus, compared to the normal uterus, is more expanded. The degree of change in shape with this malformation of the female reproductive system varies.
Many women who have a saddle-shaped uterus do not even suspect that they have such a defect. The diagnosis of “saddle uterus” is made based on the results of hysteroscopy, hysterosalpingography, ultrasound, and magnetic resonance imaging. It happens that doctors find out about the presence of this defect in a woman after the birth has taken place during the process of her cavity. And sometimes - during the next pregnancy, which does not proceed as smoothly as the first.
Diseases[edit | edit code ]
A symptom of many diseases of the uterus can be uterine leucorrhoea.
- Prolapse and prolapse of the uterus
- Prolapse of the uterus or a change in its position in the pelvic cavity and its displacement down the inguinal canal is called complete or partial uterine prolapse. In rare cases, the uterus slips directly into the vagina. In mild cases of uterine prolapse, the cervix protrudes forward at the bottom of the genital opening. In some cases, the cervix prolapses into the genital slit, and in particularly severe cases, the entire uterus prolapses. Uterine prolapse is described based on how much of the uterus protrudes. Patients often complain of the sensation of a foreign body in the genital fissure. Treatment can be either conservative or surgical, depending on the specific case. - Uterine fibroids
are a benign tumor that develops in the muscular lining of the uterus. Consists mainly of elements of muscle tissue, and partly of connective tissue, also called fibromyoma. - Uterine polyps
- Pathological proliferation of the glandular epithelium, endometrium or endocervix against the background of a chronic inflammatory process. Hormonal disorders play a role in the genesis of polyps, especially uterine ones. - Uterine cancer
- Malignant neoplasms in the uterine area.
- Endometrial cancer
- Endometrial cancer refers to cancer of the endometrium (the lining of the uterus) that spreads to the walls of the uterus. - Cervical cancer
is a malignant tumor localized in the area of the cervix.
Endometriosis
is a disease in which cells of the endometrium (the inner layer of the uterine wall) grow outside this layer.
Since endometrioid tissue has receptors for hormones, the same changes occur in it as in normal endometrium, manifested by monthly bleeding. These small bleedings lead to inflammation in the surrounding tissues and cause the main manifestations of the disease: pain, increased organ volume, infertility. Treatment of endometriosis is carried out with gonadotropin-releasing hormone agonists (Decapeptyl depot, Diferelin, Buserelin-depot) Endometritis
- Inflammation of the uterine mucosa.
This disease affects the functional and basal layers of the uterine mucosa. When it is accompanied by inflammation of the muscular layer of the uterus, they speak of endomyometritis. Cervical erosion
is a defect in the epithelial lining of the vaginal part of the cervix.
There are true and false erosions of the cervix: True erosion
- refers to acute inflammatory diseases of the female genital organs and is a frequent companion to cervicitis and vaginitis.
It usually occurs against the background of general inflammation in the cervix, caused by sexually transmitted infections or conditionally pathogenic vaginal flora, under the influence of mechanical factors, malnutrition of the cervical tissue, menstrual cycle disorders, and hormonal imbalance. Ectopia (pseudo-erosion)
- there is a common misconception that ectopia is the body’s response to the appearance of erosion, since the body is trying to replace a defect in the mucous membrane of the vaginal (outer) part of the cervix with columnar epithelium lining the uterine (inner) part of the cervical canal.
Often this confusion arises due to the outdated point of view of some doctors. In fact, ectopia is an independent disease that has little to do with true erosion. The following types of pseudo-erosions are distinguished: Congenital ectopia
- in which the cylindrical epithelium can be located outside the external os of the cervix in newborns or move there during puberty.
Acquired ectopia
- cervical ruptures during abortion lead to deformation of the cervical canal, resulting in post-traumatic ectopia of the columnar epithelium (ectopion). Often (but not always) accompanied by an inflammatory process.
| Uterus | |
| lat. uterus | |
| Parts of the uterus. | |
| Location of the uterus in the pelvic region | |
| Blood supply | uterine artery |
| Venous drainage | veins of the uterus [d] |
| Lymph | internal iliac lymph nodes [d] |
| Precursor | Müllerian duct |
| Catalogs | |
Are pregnancy and childbirth compatible?
Having learned about this diagnosis, it is important to clarify the details - they play a decisive role in this matter.
As mentioned above, a saddle uterus and pregnancy are quite compatible; you just need to make sure there is no inflammation or endocrine problems. As for partial and complete bifurcation, pregnancy most often occurs without problems. Only occasionally do you have to resort to IVF services.
Experienced doctors say that in the process of conception, the psychological attitude of the expectant mother is important. A woman should not worry about an anomaly in her structure, but believe in a successful outcome - then the chances of success are much higher.
However, with pregnancy everything is not so clear.
Find out more about how: uterine fibroids, uterine hypertonicity, uterine flexion, cervical cyst, polyps in the uterus and ovarian dysfunction affect pregnancy.
Depending on the level of bifurcation, as well as the shape of the abnormal organ, there may be various complications:
- if there are horns of different sizes, it is important in which of them the fetus will attach: if attachment occurs in the larger horn, then there is a high probability of a normal pregnancy, but in an underdeveloped horn, tissue rupture by the growing fetus is possible due to weak walls;
- the tissues of the abnormal organ do not stretch well, creating the risk of premature birth;
- possible placenta previa, premature rupture of water;
- due to the smaller size of the bicornuate uterus, there is less space for the baby in the womb, it is difficult for the baby to roll over, so the baby takes the wrong position;
- in the abnormal organ, blood circulation is disrupted, which affects the child and can also cause placental abruption;
- A bicornuate uterus can lead to premature dilatation of the cervix.
Did you know? During the first two months, all embryos are girls. Only in the third month does the development of the brain and organs responsible for the male sex begin.
A pregnant woman with abnormalities in the structure of the uterus must always be under the close supervision of specialists who, based on her condition, make decisions on how to properly organize childbirth with minimal risk for mother and child.
In the last month, a pregnant woman, most often, is already in the hospital in case of premature birth, since most women with this diagnosis still give birth before 40 weeks. In some cases, natural childbirth is possible, but doctors still prefer to plan a cesarean section - it reduces the likelihood of complications in the postpartum period.