Definition of the disease, possible routes of infection
The disease is classified as an infectious disease, the causative agent of which is chlamydia. According to research, the prevalence of pathology exists among people who are sexually active. Every year the number of infected patients increases. This is often due to the fact that the disease does not manifest itself at all for a long time. A person does not develop immunity to such parasites, even after he has already been ill.
Chlamydial infection most often attacks the genitourinary system. It parasitizes inside cells, receives nutrition from them and reproduces. Low temperatures are considered favorable conditions for it, and in boiling water it quickly loses its activity. For a long time, the pathogen remains in the body in a latent state, since many factors can impede its full functioning. But as soon as the defenses are suppressed, dormant chlamydia begins to awaken and mobilize.
The most common route of transmission of chlamydia is through sexual contact. Unlike other sexually transmitted diseases, infection occurs in only 25% of cases. Women are more susceptible to pathology, which is explained by the anatomical features of the genitourinary system. There are other possibilities of infection:
- household contact (dirty things, common items);
- airborne droplets (through sneezing and coughing);
- vertical path (from mother to fetus).
The incubation period lasts from 14 to 30 days. As a rule, a favorable condition for the spread of infection is the genital area. Sometimes pathogens are localized in the epithelium of the small intestine, which negatively affects the functioning of the entire body.
Chlamydia in women during pregnancy: causes and routes of infection
Chlamydia is considered a sexually transmitted disease that affects the genitourinary system with pronounced consequences for both sexes. The direct route of infection is hidden in contact with mucous membranes. Reasons for the development of chlamydia in women during pregnancy:
- pathogens can be transmitted sexually, through anal or oral sex;
- there is a possibility of infection with chlamydia through contact and household contact, which is extremely rarely diagnosed due to environmental intolerance to the virus.
At the same time, chlamydia, like viruses, can be concentrated, for example, on a towel for 2 days at an environmental temperature of at least 20 degrees. In addition, the fact of infection with chlamydia from domestic and other animals is excluded.
Causes of chlamydia during pregnancy
Pathology often occurs in pregnant women. It is paradoxical that cases of infection occur among those women who lead a healthy lifestyle and have a good social position. Therefore, anyone can face a similar problem.
During pregnancy, women become especially vulnerable to infection. As a result of many physiological changes, the body's defense mechanisms are reduced. Weakened immunity increases the likelihood of infection from the outside or activates parasites that are in a latent state. Chlamydia located in the mother's genital tract penetrates to the child through the amniotic fluid.
The main route of transmission of chlamydia is through sexual contact. The risk increases especially in women who have multiple sexual partners. It is important not to forget that the infected person himself may not know about his disease state for a long time. There are known cases of infection through common objects and non-compliance with personal hygiene rules.
Why does chlamydia often become a problem during pregnancy?
Unfortunately, this sexually transmitted disease very often goes unnoticed precisely because of its ability to proceed latently - without manifesting itself. As a result, we can suspect it only during the period of exacerbation.
As you know, a pregnant woman’s body is temporarily weakened due to stress, giving way to infections - and this is where they try to come out of the shadows.
Soon, while carrying a baby, a woman suddenly finds out about her illness, and may often suspect her husband - be prudent! Remember that chlamydia could live in the body for several years!
Symptoms of chlamydia in pregnant women
In most cases, pathology during pregnancy is asymptomatic. Over time, some signs of the disease still appear, but are not pronounced. These include:
- General weakness.
- Discomfort in the lower abdomen.
- Mild itching or burning of the vulva.
- Low-grade fever.
A similar clinical picture is observed in other pathologies of the genitourinary system. Therefore, in order to differentiate chlamydia, the doctor recommends undergoing a full examination.
The acute form of chlamydia is extremely rare. Since the disease is initially asymptomatic, its chronicity is often revealed upon diagnosis. During exacerbations, the clinical picture depends on where the infection is localized and the extent of its damage. Typically, women are wary of the following signs:
- Mucous vaginal discharge mixed with pus and an unpleasant odor.
- Spasms or pain during urination, reminiscent of cystitis.
- Feeling of heaviness in the bladder area.
- Uterine bleeding.
- Swelling and enlargement of the cervix.
- Burning in the perineum.
- Pain in the lower abdomen, the intensity of which periodically changes.
- Slight increase in body temperature.
Even if the listed signs are present, it cannot be said with certainty that they relate to chlamydia. This is just a reason to visit a doctor who will find out the cause.
The pathology can be simultaneously combined with bacterial vaginosis, gonorrhea, trichomoniasis or ureaplasma, which complicates the symptoms.
Affecting localization of chlamydia
For an adult, detected chlamydia does not actually pose a threat. Treatment with a course of antibiotics eliminates the threat of infection spreading. For women, the bacterium poses a particular danger due to sensitivity to the virus. During pregnancy, the risk increases, since it is quite difficult and fraught with consequences to cure a fetus that is infected from the mother by exposure to antibiotics while still in the womb.
This is how chlamydial urethritis “chooses” its location in the urethra:
- when infected, small, cloudy, whitish discharge may be observed coming from the urethra;
- the advanced form shows discharge with purulent impurities;
- during pregnancy, visits to the toilet are frequent and are accompanied by a burning sensation;
- Pregnant women, in addition to the state of gestation, feel discomfort and a feeling of vague heaviness in the lower abdomen in the area of the bladder during illness.
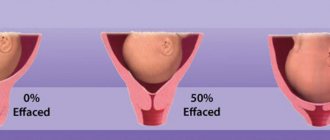
Chlamydia during pregnancy is dangerous for women who can develop the disease cervicitis, which affects the cervix:
- when infected with chlamydia at the location of the cervix, an inflammatory process develops with damage to the epithelium;
- the cervix, upon examination, is hypertrophied;
- when treatment measures are not taken, they cause erosion;
- the danger of an advanced form is hidden in the difficulty of conception, as well as in the threat of spontaneous termination of pregnancy (often in the later stages).
Dangers of chlamydia during pregnancy
Every woman during pregnancy worries about how this or that pathology will turn out for her. After all, how the baby develops in the womb affects his quality of life in the future.
For the expectant mother
If the infection is not treated in a timely manner, the mother’s body suffers first. This provokes the development of such complications:
- salpingitis;
- exacerbation of toxicosis;
- cervical erosion;
- chlamydial conjunctivitis, arthritis, urethritis;
- narrowing of the urethra.
In early pregnancy, the infection is localized in the cervix and vagina. This complicates the period of bearing a child. If the disease becomes chronic, the likelihood of spontaneous miscarriage or premature birth increases.
For a child
Chlamydial infection is no less dangerous for the development of the baby itself. There is a possibility of the following complications occurring in newborns:
- Defects of internal organs.
- Damage to the nervous system.
- Avitaminosis.
- Iron-deficiency anemia.
- Conjunctivitis.
- Encephalopathy.
- Pneumonia.
- Otitis.
Similar complications appear when the presence of chlamydia in the blood is detected during late pregnancy. The infection disrupts labor, stimulating the rapid release of amniotic fluid.
Cases of premature births have been recorded, as a result of which children were born premature or with retarded physical development.
Treatment effectiveness
Of course, you want to be treated once and for all, and moreover, this is possible with strict adherence to the correctly prescribed treatment.
However, how effective the treatment turned out to be must be checked. After all, having destroyed only part of the chlamydia, or received it again from a partner, a woman has a high probability of going through all stages of treatment and experiencing more severe consequences.
You shouldn’t immediately rush to examinations after completing the entire complex. It is necessary to wait a few weeks - 14 days after the last dose of the drug, a culture can be done, but the result can again be deceiving.
Doctors advise again to track chlamydia in several stages and, summing up the results, make sure that they are completely absent. That is, go through PIF and PCR again. These studies will have to wait - they are best done a month after taking antibiotics.
It is necessary to monitor the level of antibody titers in the blood for some time - such observations can take six months or even a year.
Diagnosis of chlamydia
Since the disease is asymptomatic in most cases, diagnosis is carried out already when the infection develops. During the examination, it is revealed which antigens are present in the patient’s blood. Laboratory techniques play a key role in this case:
- Smear to detect chlamydia.
- Bacterial culture.
- Blood test for antibodies.
- Examination of scrapings from mucous membranes.
- Molecular research (the most accurate methods: PCR and ELISA).
All of the above methods have their advantages and disadvantages. Using these methods, you can painlessly and in a short time see not only the presence of chlamydial infection, but also determine at what stage of development it is. Early diagnosis can prevent serious complications. Therefore, to establish an accurate diagnosis, doctors often recommend the use of several laboratory procedures.
By collecting anamnesis, it becomes clear what genitourinary diseases the patient has encountered. Using this data, they take a smear for those types of infections that the woman has had in the past. The reason is that the causative agents of some pathologies have a hidden course. This approach makes it possible to differentiate chlamydia from other currently active parasites.
What is chlamydia
Chlamydia is a pathogenic flora that enters the human body during sexual intercourse, or less commonly through household means. These pathogens have the properties of bacteria and viruses. Just like viruses, they are not able to survive on their own; their vital activity is directly related to the cellular structures of the host body. Thanks to him, they receive energy, since they cannot produce it.
Chlamydia prefers to settle in the deep layers of the mucous membrane of the urinary and genital organs, since they feel best in this environment. They are extremely rarely found in the lower parts of the small intestine. And in a pregnant woman, their growth and development occurs not only in the urinary tract and genitals. The danger is that when the infection spreads, the amniotic membranes and the fetus itself are affected.
Chlamydia under a microscope
The source of infection is a sick person, and the vast majority of carriers of the infection are not even aware of its existence.
Chlamydia is transmitted from mother to child through amniotic fluid.
In this case, the risk of miscarriage or the birth of a baby with pathologies increases many times. Therefore, doctors recommend planning a pregnancy, undergoing all tests and examinations, and, if necessary, treatment.
Treatment tactics for chlamydia in pregnant women
If the pathology was detected during the first trimester, experts do not recommend doing anything. At this stage, any use of drugs can provoke defects in the development of the fetus. Doctors are taking a wait-and-see approach, since the benefits of therapy will be less than the health risks. In special cases (intense vaginal discharge) in the early stages of pregnancy, the use of medications only locally (douching, rinsing, applications, suppositories) is allowed.
Treatment for chlamydia is aimed at reducing as much as possible the impact of the infection on the expectant mother and her baby and preventing the development of serious complications. For this purpose, a complex of medications is used that block the proliferation of parasites and increase the body's resistance to pathogens. In the first two trimesters of pregnancy, the treatment regimen excludes the use of antibiotics. After all, they can slow down the process of formation of the main systems of the fetus.
Chlamydial infection is often accompanied by other diseases.
Therefore, therapy will include the use of the following set of drugs:
- antiseptic;
- antiviral;
- antiallergic;
- antifungal;
- antibacterial (macrolide group);
- enzymatic;
- probiotics;
- vitamins and microelements.
Complex treatment helps to quickly reduce the inflammatory process and eliminate pathogens. In a woman’s pelvic organs, blood circulation increases and immunity increases. In this case, drugs are selected that do not harm the fetus, since they do not penetrate the placental barrier.
Prevention of chlamydia
The best way to bear a normal child is to plan your pregnancy in advance and prevent chlamydia infection. It consists of the following actions:
- use of barrier contraception during casual sex;
- regular visits to the gynecologist and testing for chlamydia;
- immediately seek help if the slightest signs of illness occur;
- undergoing full therapy and recovery after detection of infection.
Pregnancy after infection
According to experts, even with timely treatment of the disease, there is no guarantee that there will be no complications. After an infection, a woman does not always retain reproductive functions. If pregnancy does occur, it is impossible to accurately predict how successful its course will be, because chlamydia may have the following residual effects:
- Changes in hormonal levels.
- Weakening of the immune system.
- The appearance of adhesions in the uterine cavity.
- Attachment of secondary infections.
It is important not to forget that there is always a risk of relapse of chlamydia. After all, the peculiarity of these parasites is that they can live inside cells in a latent form for a long time. As soon as conditions become favorable for them, they become active. Patients who have had an infection do not develop lasting immunity to it. Although antibodies to the disease remain after treatment, after some time they disappear and the person can become infected again.
Researching the disease, doctors come to the conclusion that even after treatment for chlamydia is completed, there are hidden dangers. Therefore, after the infection has been cured, planning to conceive in the next couple of months is not recommended. The body needs to be given time to rehabilitate.
There are cases of patients who underwent long-term therapy, became pregnant and gave birth to a healthy baby.
How to identify chlamydia
It is difficult to identify chlamydia without the use of specialized diagnostic methods, since this parasite is located inside a cell of the human body. Therefore, all kinds of routine blood and urine tests do not directly detect this infection.
For research, scrapings are taken from the mucous membranes of the genitourinary tract (urethra, cervical canal of the cervix) from pregnant women; if chlamydia is located in other organs, scrapings are taken from the rectum, conjunctiva, and oropharynx.
The quality of the material taken depends on the condition of the pregnant woman.
The most informative scraping will be if the conditions for taking smears are met:
- they are taken if there are signs of disease;
- the pregnant woman was treated with local antiseptics (vaginal suppositories) for the last 2–3 days;
- did not shower for 24 hours;
- have not used systemic antibiotics for the last 3–4 weeks.
If the rules and conditions for taking the material were not followed, then the results of the study may be distorted.
To determine chlamydia use:
- Methods that directly detect the pathogen (chlamydia trachomatis) and its antigens: PIF reaction using labeled monoclonal antibodies;
- cultivating the pathogen in cell culture;
- molecular biological methods: DNA hybridization;
- Real-time PCR;
- NASBA in real time and others.
- serological.
Direct immunofluorescence (DIF) method with monoclonal antibodies
Not the most complex and acceptable method for almost any laboratory. Using PIF, chlamydia antigens are directly detected. The basis of the method is that monoclonal sera with antibodies labeled with fluoresces (luminous substances) are added to the biological material - scrapings from the mucous membranes of the genitourinary organs. These smears are examined under ultraviolet light under a fluorescent microscope. With this microscopy of chlamydia, luminous inclusions of green or yellow-green color are visible on the brown-orange background of the cell cytoplasm.
Its sensitivity and specificity are not the highest. This depends on the quality of luminescent sera with antibodies and the skills of laboratory personnel. Mutual fund results are sometimes false positive. This method is not suitable for examining scrapings obtained from the nasopharynx and rectum.
Chlamydia detected using PIF - green inclusions
Cultural method
To diagnose chlamydia, one of the more accurate methods is cultural. This study is based on sowing the taken material onto nutrient media. This is a more specific method than mutual funds. And one of the few methods by which getting rid of chlamydia is determined. It allows you to detect viable microorganisms, although other methods often give distorted results. But due to low sensitivity, its labor intensity, the length of the process of growing chlamydia, as well as strict requirements for the conditions for obtaining, transporting and storing scrapings, as well as the professionalism of the personnel, it is difficult to use it in daily practice. Therefore, this method is carried out only in a few laboratories.
Chlamydia is placed on nutrient media
Molecular biological methods
To recognize chlamydia, it is recommended to use molecular biological methods, one of which is PCR diagnostics (polymerase chain reaction). PCR is based on the amplification of nucleic acids, i.e. increasing the number of certain DNA fragments. This is a test with high sensitivity of up to 98% and specificity of up to 100%. When performing it, not only scrapings from the mucous membranes are used, but also other materials, for example, urine, ejaculate. For diagnosis, it is not important to maintain the viability of chlamydia, but strict adherence to the delivery conditions of the collected material is required, since this significantly affects the results of the analysis.
PCR diagnostics is currently considered the main method for detecting chlamydia.
PCR is a method of increasing the number of certain DNA fragments
These methods also include real-time PCR and a new, improved method - NASBA (Nucleic Acid Sequence-based Amplification), i.e. increasing the number of copies of nucleic acids (RNA) in real time, which makes it possible to identify living chlamydia and replace labor-intensive culture method.
Nowadays it is molecular biological methods for detecting and diagnosing chlamydia that should be given preference in practical healthcare.
Serological method
With the serological method, the pathogen is not directly detected, but the body’s immune response to chlamydial infection is examined, i.e., immunoglobulins (IgM, IgA, IgG) that are produced in the human body to chlamydial antigens are determined. This is important for diagnosing chlamydial inflammation in the fallopian tubes, appendages, pelvic peritoneum and determining its acute or chronic course. Serological methods include microimmunofluorescence (MIF), enzyme-linked immunosorbent assay (ELISA) studies. But to confirm the diagnosis of chlamydia of the genitourinary organs, the diagnostic capabilities of these methods are limited. They cannot be used to control the cure for infection.
According to modern protocols for the management of infectious patients, serological methods (determination of antibodies in blood serum) are not used to diagnose chlamydia of the genitourinary system.
However, the determination of immunoglobulin M is used to confirm chlamydial pneumonia in children from birth to the first three months of life. An increase in the immunoglobulin G titer by 4 times when paired blood sera are examined speaks in favor of the presence of chlamydia in pregnant women with inflammatory diseases of the pelvic organs. An increase in the concentration of IgG to chlamydia is a reason to examine women for the presence of lymphogranuloma venereum. This technique allows you to determine the stage of the disease, evaluate the effectiveness of the treatment, and prove the chlamydial origin of the disease, which develops outside the genital organs.
Not an informative method for pregnant women
How does the disease affect childbirth?
Pregnant women infected with chlamydia give birth just like everyone else, in a regular obstetric ward. Of course, all antiseptic measures are taken to prevent others from becoming infected.
How childbirth will proceed with chlamydia depends on the woman’s body.
If the course of the disease is not complicated, then the woman gives birth naturally. If, as a result of chlamydia, weak labor occurs, then artificial stimulation is used or a cesarean section is performed.
Laboratory diagnostics
Currently, there are several ways to diagnose chlamydial infection. Let's look at the most popular methods in descending order.
7.1. Polymerase chain reaction
Polymerase chain reaction (abbreviated PCR) is a popular and reliable method for detecting chlamydial infection, its sensitivity is 98-100%. The method is expensive.
The essence of PCR is to detect DNA and its fragments, as a result of which the possibility of detecting chlamydial bodies increases many times.
This method is quite specific, gives reliable results in 97-99% of cases, both invasive (scrapings) and non-invasive (excretions, urine) media are used as material.
When carrying out PCR diagnostics, it is necessary to remember that after eradication of chlamydia with antibacterial therapy, a false positive result is possible within 30 days after the therapy.
This is due to the fact that when carrying out PCR, it is not the viability of chlamydial bodies that is assessed, but the direct presence of DNA fragments. Therefore, it is necessary to take these deadlines into account when prescribing a control analysis.
7.2. RNA amplification method (NASBA)
This method is also highly sensitive (98-100%, specificity about 100%). To obtain a reliable result, the collection of material is of particular importance:
- 1Scrapings from the cervical canal in women should be taken outside of menstruation.
- 2Urethral scrapings should be taken no earlier than 3 hours after the last urination.
- 3Sample storage conditions and transportation rules must be observed.
Like PCR, the RNA amplification method can give a false-positive result after treatment of chlamydia with antibacterial drugs, if the material was collected earlier than 14 days after the end of the course.
7.3. Enzyme-linked immunosorbent assay (ELISA)
It is easy to perform, fully automated, gives reliable results in 85% of cases, and is economical. Its essence lies in identifying not the chlamydial particles themselves, but antibodies to them.
At the same time, based on the class of identified antibodies, one can judge the duration and nature of the process. If IgG is detected, one should speak of a previous infection; this is the so-called “immunological scar”.
IgA and IgM indicate a recent process. The combination of all types of immunoglobulins indicates the course of the acute process, and the presence of both IgA and IgG is evidence of reactivation of the infection.
This method is not recommended for confirming the presence of urogenital chlamydia. Its capabilities are limited only by the differentiation of an acute infectious process.
7.4. Cell culture research
This is one of the very first methods for detecting chlamydial bodies inside cells. Its essence lies in the direct study of a preliminary scraping taken and stained for the presence of intracellular inclusions.
The method is effective only in the acute phase of the disease, its reliability is only 10-12%. Specially trained personnel are required to perform this test. Cell culture research is subjective and therefore not widely used in clinical practice.
7.5. Direct fluorescence reaction (DIF)
RIF is based on an antigen-antibody reaction. The material taken (scraping) is treated with “labeled” antibodies, which bind to chlamydia antigens and, when illuminated with a fluorescent lamp, give a light green glow.
This method is also quite subjective and depends on the experience of the laboratory assistant. The reliability of this method does not exceed 70%. A false positive result is also possible in the presence of concomitant infections of the urogenital tract.
Other serological reactions include: complement fixation reaction (CFR); indirect hemagglutination reaction (IRHA). They are used extremely rarely.
During pregnancy, testing for chlamydia must be carried out at any time during registration. In the third trimester, it is advisable to repeat the study to exclude an acute process and prevent intrauterine infection of the fetus and newborn during childbirth.
How does childbirth occur with chlamydia?
A chlamydial infection that occurs during pregnancy is not an indication for a cesarean section. Childbirth can take place vaginally if there are no other reasons for surgery. Chlamydia does not affect the course of the birth process in any way. Doctors only fear that the baby will become infected during childbirth, so they take all measures to ensure that this does not happen.
Termination of pregnancy for chlamydia is not performed. This disease is not an indication for medical abortion. The expectant mother is informed about the possible risks and is offered treatment for chlamydia in the second half of pregnancy.
Principles of treatment of chlamydia during pregnancy
Treatment of the disease during pregnancy should be comprehensive. The sexual partner should also be treated together with the expectant mother so that the infection does not continue in circles. Until complete recovery, it is better to avoid sexual intercourse or use condoms. If these rules are not followed, the disease may become chronic.
Treatment of chlamydia during pregnancy should not be delayed under any circumstances. As in the treatment of any bacterial infection, antibacterial drugs are used that penetrate into the cells
Doctors set themselves the maximum task. They must cure the woman of her illness. At the same time, you need to ensure that the prescribed medications do not affect the baby’s health. There are a number of medications that will not cause much harm to the body of the unborn child.
But still, the bad effect of medications on the child’s body cannot be ruled out. Therefore, courses of therapy should be short.
Self-medication of chlamydia, especially during pregnancy, is strictly prohibited. Treatment should be carried out by a doctor. Usually pregnant women are prescribed: Amoxicillin. Erythromycin and Viferon suppositories.
“Compatibility” of pregnancy with chlamydia
This disease is not an obstacle to conceiving a baby. To give birth to a healthy child, it is better to first undergo all examinations, detect and treat the disease in time.
Note! It is very easy not to notice that chlamydia has appeared due to weak or practically absent symptoms.
Most often, chlamydia and pregnancy are accompanied by the following symptoms:
- discharge similar to purulent, different from normal;
- unpleasant odor from the vagina;
- feeling of mild pain in the lower abdomen or on the genitals - both internal and external;
- itching, burning.
Very rarely, but body temperature may rise and general weakness may occur. At the same time, all symptoms may be evidence of the presence of other diseases of the genitourinary system.
If you detect at least one sign, you should immediately consult a doctor.
Symptoms
Chlamydia can be asymptomatic for a very long time. However, this mostly applies to healthy women. During pregnancy, a woman’s immune system is depressed, so the first signs of the disease may appear 1–2 weeks after infection.
The main symptoms of chlamydia during pregnancy:
- unusual discharge from the genital tract;
- general signs of intoxication (malaise, fever, headache, etc.);
- drowsiness, sharp decrease in performance;
- aching pain in the lower abdomen, which can worsen when exposed to high temperatures (in a bathhouse, sauna, hot bath, etc.);
- frequent false urge to urinate;
- emptying the bladder is accompanied by pain, itching and burning.
In clinical practice, there are cases of Reiter's syndrome in pregnant women, a special form of chlamydia. This disease is caused by the presence of a characteristic symptomatic triad:
- inflammation of the urethra;
- inflammation of the mucous membrane of the eye (conjunctivitis);
- inflammation of the joints (mono- or polyarthritis).
In some cases, the clinical picture of chlamydia during pregnancy may be blurred, that is, at the initial stages of the development of the disease, a woman may not feel any obvious symptoms. In addition, the expectant mother may associate the appearance of certain pathological signs with pregnancy and, because of this, do not immediately seek help from a doctor.
When planning a pregnancy, a woman should be tested in advance for infections of the reproductive system in order to avoid the occurrence of various complications in the future. It is also equally important for the potential father to undergo similar examinations.
If pregnancy does not occur for a long time with regular sexual intercourse, then this is a reason to be tested for chlamydia. Also characteristic signs may be frequent cases of spontaneous abortion in the early stages or the detection of other sexually transmitted infections.
Preventive measures
Those women who have previously had gynecological problems are most susceptible to developing the disease in an acute form. Anyone can become infected with chlamydia. But a healthy body activates its immune defense, which contributes to the rapid destruction of pathogenic microorganisms.
Chlamydia is an infection that is easier to avoid than to get rid of. The main rules for the prevention of chlamydia, as well as other sexually transmitted infections, is to have a regular sexual partner
Preventive measures usually include:
- compliance with personal hygiene rules;
- maintaining a correct lifestyle;
- sexual contacts should be regulated, with one partner.
- The main rule is to take care of your health. Visit a gynecologist once a year and take all necessary tests to help determine the presence of sexually transmitted infections.
Consequences of chlamydia for the fetus
During pregnancy, the fetus may become infected with chlamydia found in the cervical canal and urethra. In the first trimester of pregnancy, infection often causes miscarriage. Even if pregnancy can be maintained, it rarely proceeds well. Formed chorioamnionitis (inflammation of the membranes) subsequently leads to the development of placental insufficiency. In this case, the placenta cannot perform all the required functions and provide the baby with oxygen and nutrients. Hypoxia develops - oxygen starvation of the fetus. This condition most affects the development of the nervous system, leading to the appearance of various neurological disorders in the newborn.
The lack of nutrients supplied through the placenta also affects the formation of all organs of the baby. In the second half of pregnancy, intrauterine growth retardation is often detected. This situation leads to the birth of a child with low body weight, who subsequently requires long-term treatment.
Infection of a child does not only occur in the womb. Very often, chlamydia reaches the newborn as it passes through the birth canal. Caesarean section does not prevent infection. Children born surgically become infected with chlamydia quite often. In this case, damage occurs to the mucous membrane of the eyes and nose. In newborn girls, chlamydia settles in the genital tract, causing the development of colpitis.
Chlamydial infection in newborns is rarely limited to rhinitis and conjunctivitis. The inflammatory process can spread to the lungs, causing the development of pneumonia. Other internal organs are often affected: liver, kidneys, stomach and intestines. The baby's nervous system also suffers. There is increased excitability, frequent crying, profuse regurgitation, and decreased muscle tone. All these symptoms are not specific to chlamydia and can occur with many intrauterine infections.
Diagnosis of chlamydial infection in a pregnant woman
Basic methods for diagnosing chlamydia:
- Examination of discharge from the cervical canal. It is a fairly reliable diagnostic method that allows identifying the pathogen using the polymerase chain reaction method.
- Collection of amniotic fluid. Carry out to detect the penetration of infection to the fetus.
- Blood test to detect antibodies to chlamydia.
- Additional smear sampling to identify concomitant infections.
The polymerase chain reaction method allows you to identify a microorganism by specific DNA
Thanks to an integrated approach to diagnosis, it is possible to detect an infection in the initial stages of its development, preventing a negative impact on the fetus or reducing risks to zero.
In addition, differential diagnosis of chlamydia with other sexually transmitted diseases is carried out.
Is it necessary to treat a baby with chlamydia?
Chlamydia in newborns can also be treated with antibiotic therapy. Erythromycin or other drugs from this group are used to treat babies in the first days of life. If internal organs are damaged, therapy is carried out in a hospital setting. Chlamydia received from the mother can persist in children for three years.
Treatment for chlamydia is carried out not only in the pregnant woman, but also in the father of her child. If both partners are not treated, the infection will return in the near future. The same groups of antibacterial drugs are used to treat men. The selection of dosage and monitoring of the effectiveness of therapy is carried out by a urologist or andrologist.
It happens that during pregnancy a woman never finds out about her disease. This happens to expectant mothers who are not registered at the antenatal clinic or who refuse to be examined for chlamydia. If left untreated, the baby becomes infected in utero or during childbirth. An infection is detected in a newborn, after which pediatricians begin treatment. At the same time, chlamydia therapy is prescribed to a postpartum woman who did not receive medications during pregnancy.