Threat of miscarriage: ICD-10 code
What does the international classification of diseases say about this problematic situation? This is code O20.0, which in this classification is called threatened abortion. ICD-10: threat of miscarriage (timing) - what can be said about them? In this case, there is a danger of separation of the fetus from the uterine wall. The eighth to tenth week can be considered the most dangerous in this regard.
Ultrasound: threatened miscarriage (MCD) is a reminder that with appropriate ultrasound diagnostics after a woman becomes pregnant, such a problem can be prevented if problems are suspected in time.
Signs of a threatened miscarriage in the early stages
The first symptom that should alert a woman is the appearance of pain. In the lower abdomen, you can feel a sipping painful sensation, which can also be localized in the lumbar region. In the presence of injury or a stressful situation, severe pain may be observed, which quickly turns into cramping. In this case, you may also experience intense bleeding. If bleeding begins, you need to urgently call an ambulance, as in this case you can lose your own pregnancy.
If there is a threat of interruption of pregnancy, you can also see the presence of bloody discharge. Sometimes such secretions may not exist when there is a threat. If you do not take action after the appearance of small bloody discharge, it may intensify and acquire a scarlet bloody color. Why does such discharge appear when there is a threat of miscarriage? The fact is that the fertilized egg gradually begins to peel off from the uterine wall, as a result of which the blood vessels are damaged.
Other symptoms include a decrease in basal temperature and a drop in the level of human chorionic gonadotropin. The woman's basal temperature should be monitored regularly and only when a verdict is reached about the presence of a threat. If a woman has had problems getting pregnant for a long time or has persistent hormonal imbalances, she will be familiar with the basal temperature monitoring schedule.
How to set deadlines?
There are several ways to determine the gestational age during IVF:
- Obstetric. To the first day of the last menstruation, 9 months are added and 2 weeks are subtracted.
- Embryonic. 9 months are counted from the date of fusion of sperm and egg.
- Gynecological. The deadline is set after examining the uterus in a gynecological chair.
- Ultrasound. The method is effective in the first trimester. The doctor takes special measurements that allow you to determine the “age” of the fetus.
- Self-determination of the deadline. In this case, it is determined approximately. When a woman first feels the kicks and movements of the baby, this is considered to be approximately the 20th week for the 1st pregnancy.
Threat of miscarriage in the early stages: treatment
Russian doctors prefer to take an integrated approach to treating women at risk of miscarriage. The sooner treatment is provided, the higher the likelihood that the pregnancy will be saved. The therapy used should be both medicinal and other. You also need to follow a daily routine and proper nutrition.
The first thing that needs to be mentioned is the use of basic therapy. This concept includes adherence to the regime and proper dietary nutrition. Pregnant women should avoid intense physical activity; sometimes it is recommended to remain in bed. It is important to sleep enough hours a day and maintain sexual rest. Moreover, it is important that a woman’s diet contains adequate amounts of proteins, carbohydrates and fats. Sometimes, if a woman is in a nervous state, she will need psychotherapy and auto-training sessions.
As a means of calming, taking valerian or motherwort tincture is indicated.
Treatment of threatened miscarriage with medications
Once the threat of miscarriage and symptoms are known, we can begin to talk about treatment methods with medications.
Threat of abortion: forum - what kind of request is this? Very often, if a woman has been diagnosed with this, she seeks somewhere to find support, both moral and in the form of advice. And very often the source of such support is various kinds of forums.
Threatened miscarriage: what to do in this case? Doctors often decide to prescribe antispasmodics to a woman. They are represented by drotaverine, noshpa, which lead to relaxation of the uterine muscles. However, as a rule, such drugs are administered intramuscularly. An excellent remedy is Magne B6, which contains the vitamin of the same name and magnesium. Rectal suppositories with papaverine are also used. Papaverine is able to quickly cope with pain.
Often, when there is a threat of miscarriage, hormonal agents, namely progesterone, are used. In the early stages, Duphaston is prescribed in a dosage of 40 mg, four tablets at once. After this, you need to take one tablet every eight hours. If it is not possible to stop the threat of miscarriage, then the dosage has to be increased. Another commonly prescribed remedy is Utrozhestan.
O00-O08 Pregnancy with abortion outcome
The ICD code from O00 to O08 contains items where the pregnancy is confirmed, but with an abortive outcome, when the pregnancy is interrupted for one reason or another before the due date:
- O00 Ectopic or otherwise ectopic conception with subsections where ovarian and tubal pregnancy is present, as well as other anomalies of egg implantation.
- O01 Hydatidiform mole, formed extremely rarely with two completely different development paths. In the first case, the egg is not able to divide into an embryo and fetal membranes, and in the second, fertilization occurs with two sperm, which leads to the death of the zygote and the formation of pathology.
- O02 Many different abnormal forms of conception.
- O03 Spontaneous abortion or miscarriage with associated negative consequences.
- O04 Medical planned termination due to the presence of pathological reasons in the viability of the baby and the mother’s body.
- O08 Complications due to abortion, ectopic or molar pregnancy; in addition, any deviation associated with interruption of pregnancy can be indicated here.
Pregnancy after threatened abortion
If a woman does have a miscarriage, she is concerned about what to do next and how long after she can try to conceive a child again. Of course, this is a great tragedy not only for the woman herself, but also for her entire family. That is why the first step on the path to recovery can be considered the normalization of one’s own psycho-emotional state. If a woman is unable to cope with this on her own, then she needs to seek help from a psychologist or psychotherapist. Of course, a woman wants to try to conceive a baby again as soon as possible. But there is no need to rush into this.
Doctors recommend that women wait at least six months before trying to conceive again. During this period, you need to take care of reliable contraception. The fact is that if a subsequent pregnancy occurs immediately after a miscarriage, the likelihood of the situation repeating increases several times. This must be taken into account when planning a subsequent pregnancy if a woman wants to carry it to term.
Causes
Rarely does a single factor lead to a frozen pregnancy; in most cases, it is a whole complex. The role of the following conditions in fetal loss syndrome has been reliably established:
- genetic abnormalities;
- infections;
- endocrine diseases;
- immunological processes;
- thrombophilia.
Some of them can be influenced and eliminated for the next attempt at conception. But not all genetic problems, immune reactions or thrombophilias can be corrected.
Genetics
Genetic problems are the most common cause of early embryo death. Research shows that this is 60-75% of cases. At later stages (at 17-28 weeks), chromosomal abnormalities are detected in only 2-7%. Common deviations:
- autosomal trisomies - Down syndrome, Patau syndrome, Edwards syndrome;
- monosomy 45XO - Shereshevsky-Turner syndrome;
- triploidy - a triple set of chromosomes, karyotype 69ХХХ or 69ХХY;
- tetraploidy - a set of chromosomes that is a multiple of four: 92ХХХ, 92ХХY.
Pregnancy failure due to chromosomal rearrangements occurs in several scenarios:
- cell division is disrupted;
- the development of the embryo and chorion is desynchronized;
- the processes of cell migration in the embryo change;
- the development of the chorion is delayed.
Also, the cause of chromosomal abnormalities is a translocation, the carrier of which is one of the parents. It is suspected in cases where a woman has repeated frozen pregnancies at a short period of time.
Sometimes children with chromosomal abnormalities survive, but are born with malformations of internal organs (including those incompatible with life). The heart and large vessels, brain, digestive tract and genitals are often affected. In some cases, it is possible to perform corrective surgeries. But children do not always live to an age when such manipulations are permitted.
The genetic factor is the main cause of undeveloped pregnancies and early miscarriages. Therefore, in the United States and many European Union countries, clinical tactics do not provide for conservation therapy in the event of a threat of spontaneous abortion.
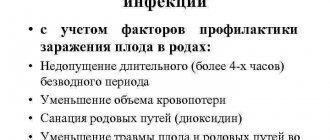
Infections
Inflammatory diseases of the pelvic organs, despite the widespread use of antibiotics and advances in diagnosis, do not tend to decrease. On the contrary, the availability of antibacterial agents has led to a change in the spectrum of pathogens. The cause of inflammatory diseases of the genital organs is often opportunistic flora.
The clinical course also changed. Acute forms often become chronic. But the primary latent course, without pronounced symptoms, fever and with erased pain, has also become widespread.
There are no strictly defined types of microorganisms that lead to non-developing pregnancy. It is not necessary that there be a direct effect of the bacterial flora on the embryo. The presence of microbes in the uterine cavity and the formation of chronic endometritis also lead to disruption of the development of pregnancy. Most often, the following microorganisms act as pathogens:
- staphylococcus;
- Escherichia coli in combination with staphylococcus;
- enterococcus;
- herpes simplex virus;
- gardnerella;
- chlamydia;
- mycoplasma;
- ureaplasma.
Isolated microbial monoinfection is rare; in 70% of cases it is a microbial-viral association. Its long-term presence in the body is caused by the inability of the immune system to completely eliminate the source of infection.
Chronic inflammation increases the migration of macrophages, special forms of leukocytes - natural killer cells, T-helpers - into the lesion. They synthesize cytokines - substances that affect pathological cells and foreign microorganisms. Therefore, instead of the immunosuppression necessary during pregnancy, the immune system actively works in the uterine cavity. And this prevents normal implantation of the embryo.
Viruses, unlike bacteria, are able to directly penetrate the cells of the developing embryo, disrupt their division or cause death. The herpes virus and adenovirus affect the vascular endothelium, causing a state of thrombophilia and local immunological reactions.
Endocrine problems
The fetus freezes under the influence of endocrine factors in 30-70% of cases. They have different development mechanisms, but the last stage is the formation of corpus luteum deficiency. This condition is caused by:
- hypothyroidism;
- polycystic ovary syndrome;
- endometriosis;
- genital infantilism;
- hyperandrogenism;
- diabetes.
Low progesterone levels lead to insufficient preparation of the endometrium for implantation. If the embryo cannot fully attach to the wall of the uterus, the processes of vascular formation and chorion formation are disrupted. With insufficient compensatory reactions, miscarriage occurs in the first trimester. If pregnancy can be maintained, this is fraught with the development of gestosis and fetal death in the second half of gestation.
Immune mechanisms
Autoimmune diseases are the body’s fight against itself; a frozen fetus is formed a second time. The most common pathologies are:
- systemic lupus erythematosus;
- myasthenia gravis;
- autoimmune thyroiditis;
- antiphospholipid syndrome.
Alloimmune reactions are distinguished separately.
- Hemolytic disease. Develops in a newborn (from the first pregnancy) due to incompatibility with the mother’s blood type or Rh factor. With repeated pregnancies, the woman’s body will already have antibodies that will disrupt the development of the embryo.
- Incompatibility of spouses. Each person has a unique set of antigens presented in leukocytes, which are combined into the HLA system. It determines the compatibility of tissues in donors, as well as germ cells in spouses. If there is HLA incompatibility, the mother’s body does not produce antibodies that can protect the developing fetus from her own leukocytes.
- Sensitization to hCG. There is excessive activation of certain types of leukocytes, which begin to produce autoantibodies to their own hormones: estradiol, progesterone, human chorionic gonadotropin. In this case, excessive fibrin deposition and a pattern of thrombophilia are noted.