Fetal development at 22 weeks
The baby’s nervous system is improving, new convolutions are formed on the surface of the brain, additional connections appear between neurons and different segments of the spinal cord and brain. A more mature nervous system provides more opportunities for motor activity. The child no longer moves his arms and legs chaotically, but purposefully.
Now he can take himself by the leg or the other hand, and wrap his palm around the umbilical cord. On an ultrasound, you can see how identical twins at this stage of pregnancy touch each other and even hold hands. It is possible that this happens by accident, but it is very touching to see such interaction. In addition to having a positive effect on the development of movements, the maturing nervous system helps the child to better sense the influence of the world around him. The baby feels a touch on the stomach from the outside, reacts to loud sounds and the bright light of a lamp brought too close.
Fetal parameters:
- Weight – 350-400-450 g;
- Height – 25-27 cm;
- Heart rate – 140-160 beats per minute.
The skeletal system becomes more perfect, which allows the baby to manifest its presence quite noticeably to the mother. Changes occur in the structure of the spine at week 22 - intervertebral discs and vertebrae are formed, and an increasing amount of calcium is deposited.
The heart works actively, pumping blood through the vessels with high intensity. Its beating at this stage can be heard simply by placing your ear to the belly of a pregnant woman. Don’t be upset if your family can’t hear the baby’s heartbeat – clear sensations will appear when the baby takes a certain position.
Nails, hair on the body and head of the fetus, eyebrows and eyelashes also grow. There is still too little melanin in thin and transparent hair, so it is still difficult to determine its color.
The viability of such a baby outside the environment of the mother’s body is extremely low. In medical practice, there are cases where children born at 22 weeks as a result of an interrupted pregnancy, with modern equipment and proper care, still survived.
Future mom
Communication with the baby is very, very important. Talk to him, consult with him, share secrets - he is so soothed by the voice of his mother! Always remember that he feels your mood and experiences all emotions with you. Also learn to capture his mood, feel and study his sleep and wakefulness patterns. In moments of anxiety, try to calm Masik down - sing him a song, stroke his tummy. Some scientific studies show that from this period the fetus not only feels you, but also understands you perfectly. Meanwhile, do not forget about physiology: it is important to walk correctly, stand correctly, sit and lie correctly - everything matters. The load on the spine and lower back is constantly increasing, you feel more and more the heaviness of the “load”, fatigue in your legs, swelling and other complications may have already appeared. Do not cross your legs; try to raise your legs a little higher than usual while resting. You need to sit and lie on hard, flat surfaces, without falling into a chair or mattress. If your legs begin to get more tired and your feet no longer fit in your old shoes, buy yourself another one, a larger one. Walking comfort is very important now. Of course, the legs must breathe, so no rubber or leatherette! It would be good if there was an orthopedic insole inside. If it's winter, be sure to check that your shoes are non-slip. With each subsequent week, your weight will increase, and your health may worsen somewhat. So hurry up to enjoy life now: relax, take a walk, go to nature with your beloved husband, have sex if you have no contraindications to this. But keep in mind that in the second trimester the level of hemoglobin in the blood often drops: if you feel unwell, lie down, sit down, ask for help in a public place.
Feel
Since during this period of pregnancy the volume of blood increases significantly, the formation of some of its cells (red blood cells) may proceed much more slowly than required. Physiological anemia, or lack of iron in the blood, occurs. To treat and prevent this condition, the doctor prescribes iron-containing medications and recommends increasing the proportion of foods such as beef and veal, liver, apples, pomegranates and pomegranate juice in the diet.
Due to the increased consumption of calcium by the fetus, its deficiency may be felt in the mother's body. It manifests itself as cramps in the calf muscles, most often occurring at night. To get rid of these negative feelings, you need to eat lactic acid products, cheese, and cottage cheese more often.
The increased volume of fluid in the body in some women manifests itself as edema. The shoes become tight and it is difficult to remove the ring from your finger. You should definitely tell your pregnancy doctor about these problems. Sometimes edema is a manifestation of gestosis, or late toxicosis of pregnancy, a condition that threatens the mother and child.
How should an expectant mother eat?
Nutrition should be thought through more and more carefully. After all, not so much the condition and development of the baby depends on it, as the condition of the mother. After all, the fetus, if necessary, will take everything from the mother’s body.
At the same time, nutrition can completely correct a number of problems that a woman experiences. And here it is important to work out your menu in very detail. In addition, it is important to remember that the mother during this period is responsible for the formation of the child’s taste preferences. Therefore, it is worth choosing the best.
Doctors recommend giving preference to fresh foods, preferably regional and seasonal – these contain more vitamins. As for heat treatment methods, it is worth choosing options without oil - steaming, stewing and baking.
You should also worry about your drinking regime - you should drink as much clean water as possible. This will allow you to maintain balance, remove toxins, and prevent constipation.
You can share the article with friends via social media. networks:
Abdomen and uterus - how to distinguish training contractions from premature birth?
At week 22, the belly is not yet large enough to limit a woman’s movements. Perhaps she still works, copes well with self-care, and can do special gymnastics for pregnant women. On an ever-expanding belly, the skin stretches more and more. This process is accompanied by severe itching and the appearance of stretch marks. To prevent such phenomena, you should moisturize the skin of the abdomen with special products.
The uterus is located 2 cm above the navel, its bottom reaches the diaphragm, which sometimes brings unpleasant sensations: difficulty breathing, heartburn. Its size is so significant that there is pressure on the intestines, stomach and bladder at the same time. Digestive problems and a tendency to constipation appear.
Light, painless contractions that a woman can feel up to 10-15 times a day are Breston-Higgins training contractions. With their help, the uterus prepares for the upcoming labor. If they are not accompanied by severe pain, there is no need to worry. Severe pain that accompanies frequent contractions may indicate that premature labor has begun. In this case, urgent hospitalization of the pregnant woman is necessary.
What to do?
Getting rid of abdominal pain at 22 weeks is quite difficult. Experts recommend that pregnant women get more rest. In fact, in a supine position the pain noticeably subsides, and may even disappear altogether. On the other hand, in order for the muscles to adapt faster, it is recommended to engage in light sports. And walking is especially important. It is very important to combine sports and rest so that abdominal pain in the 22nd week does not bother you so often.
You should not take painkillers during pregnancy, as they can cause serious harm to the unborn child. If the pain becomes very severe and difficult to endure, then this is already a pathological symptom that requires consultation and examination by a doctor. It is possible that the cause of pain in the lower abdomen or another part of it does not lie in sprained ligaments and muscles.
Movements - what's new?
At this stage of pregnancy, a woman has already learned to distinguish by the nature of her movements whether the baby is sleeping or awake. Often he moves actively just when the mother is about to rest or during a night's sleep. If a child makes a series of sudden movements, perhaps he does not have enough oxygen, and in this way he is trying to activate his cardiac activity.
If movements are not felt throughout the day, it can be assumed that the course of pregnancy has taken a negative turn and it has faded. You should immediately consult a doctor about this problem.
Gestational age
Doctors determine the gestational age in obstetric weeks, which differ from the calendar period. In addition, you can determine the period from conception. In particular, 22 obstetric weeks of pregnancy correspond to 20 weeks from conception. Many women find it convenient to determine the period in months. Twenty-two weeks of pregnancy is the sixth obstetric month. If we consider the calendar period, we can say that 22 weeks of pregnancy correspond to five whole months.
Obstetric gestational age is determined in weeks. Each obstetric month has four weeks. Time is counted from the first day of the last menstruation that preceded conception. The obstetric date is two weeks ahead of the calendar date.
The obstetric gestational age corresponds to 10 months, each of which is defined as four weeks.
Twenty-two weeks of pregnancy means that a little more of the pregnancy is already behind you.
Vaginal discharge is normal
At this stage of pregnancy, the nature of vaginal discharge practically does not change - it is still light and translucent, without an unpleasant odor. If a woman detects inclusions in the discharge that look like cottage cheese, a change in their color and structure, it is quite possible that she has vaginal candidiasis or a bacterial infection. It is necessary to immediately take a smear for urogenital infections to prevent the penetration of pathogenic microorganisms from the vagina into other parts of the reproductive system. Vaginal candidiasis is quite common in pregnant women. This is explained by the fact that local and general immunity decreases during pregnancy, which leads to the activation of the fungus and its proliferation.
Treatment of thrush does not take much time when both partners undergo antifungal therapy at the same time. There are effective drugs for local and general action, specifically designed for the treatment of pregnant women. To prevent candidiasis from returning, you should not eat a lot of sweets, you should wear cotton underwear and carefully observe intimate hygiene.
Changes occurring in the female body
Throughout pregnancy, a woman's body undergoes many amazing changes. First of all, these changes relate to the growth of the uterus and breasts, and weight gain.
At 22 weeks of pregnancy, a decrease in blood pressure is often observed due to an increase in the amount of circulating blood. Weakness, nausea and dizziness may occur. If you experience frequent dizziness, you should consult a doctor to prevent fainting and injury.
In the second trimester of pregnancy, the appearance of so-called stretch marks or stretch marks is sometimes noted. These are areas of connective tissue that form when elastin and collagen fibers break. Stretch marks often appear in women who gain weight quickly.
The woman's gait resembles the movements of a duck. The gait features of pregnant women are associated with the divergence and softening of the pelvic bones. At 22 weeks of pregnancy, you may experience an increase in appetite. Because the sweat glands work under increased stress, you may experience an increase in sweating. The heart rate increases as the heart pumps more blood.
Changes during pregnancy also affect skin conditions. Many women note the appearance of age spots that disappear after childbirth. If gum bleeding occurs, which often occurs during pregnancy, you can use special herbal toothpastes and rinses. We should also not forget about the need to sanitize the oral cavity.
Uterus
At 22 weeks of pregnancy, the uterus is located in the abdominal cavity. The uterine body will no longer interfere in the pelvis. A woman can feel the tone when it occurs. If tone occurs frequently, you should consult a specialist.
The height of the uterine fundus is 20-24 centimeters. Typically, the value of VSDM is approximately equal to the number of weeks.
The average length of the uterine cervix is 4 cm. A shortened cervix usually indicates ICI. Isthmic-cervical insufficiency is dangerous due to premature birth.
Weight gain
Your weight needs to be monitored at any stage of pregnancy. Moreover, at 22 weeks of pregnancy, most women have a good appetite. In general, weight gain is pronounced. Excess weight negatively affects the well-being of mother and child. It should be remembered that a rapid increase in body weight may indicate gestosis.
Women with a fragile physique are allowed to gain up to 7 kilograms. With normal weight, the increase should be no more than 5.5 kilograms. If your mother was overweight or obese before pregnancy, you can gain up to 3.5 kilograms by 22 weeks of pregnancy.
You should weigh yourself in the morning on an empty stomach every week. To obtain objective results, you should weigh yourself with or without the same clothes. If the increase exceeds the permissible norm, it is necessary to analyze the diet. Treatment is indicated for weight gain caused by edema. Such representatives are usually hospitalized and treated in a hospital setting.
Mammary gland
The growth rate of the mammary glands has decreased compared to the first trimester. There is practically no discomfort in the chest. However, due to a change in the center of gravity, lower back pain is sometimes noted.
During pregnancy, you should pay attention to a bra with wide straps that supports your enlarged breasts. At 22 weeks of pregnancy, colostrum may be released from the breasts. This is a nutritious liquid for feeding a newborn in the first days of his life. At this stage, colostrum is yellowish in color and has a thick consistency. Before birth, colostrum becomes more transparent.
At 22 weeks of pregnancy, stretch marks may appear on your breasts. To prevent them, it is necessary to use special cosmetics.
Ultrasound and other tests
If, according to the plan of the antenatal clinic, you have to visit a gynecologist for the 22nd week, you should come to the appointment having previously passed urine tests for the presence of protein, a general blood test for leukocytes and red blood cells, and blood for sugar. Already at the appointment, the midwife will measure the height and weight of the pregnant woman, the level of the uterus, and listen to the baby’s heart sounds.
It is possible that a second ultrasound will have to be performed at this stage of pregnancy.
Parameters determined by the ultrasound diagnostic doctor:
- The ratio of the child’s body proportions;
- The presence or absence of developmental defects;
- The condition of the internal organs, the degree of their formation;
- Volume and condition of amniotic fluid;
- Condition of the uterus, umbilical cord and placenta;
- Gender of the child;
- Monitoring possible oligohydramnios or polyhydramnios.
Based on the results of the ultrasound, the doctor will give the necessary recommendations; if the parents wish, he will record a video of how the baby looks and moves.
Diagnostics
Ultrasound shows the position of the fetus, reveals developmental disorders, determines the method of delivery
To determine the condition of the fetus and identify pathologies, the expectant mother is required to undergo an ultrasound examination. During an ultrasound, the doctor determines the development and functionality of the child’s internal organs and the presence of congenital defects. The presence of a danger of miscarriage or premature birth can be determined based on the amount of amniotic fluid, the condition of the placenta and umbilical cord, and the cervix.
If alarming symptoms develop, a woman is prescribed the following diagnostic procedures and tests:
- Gynecological examination of the cervix. Based on the study, the doctor determines the possibility of premature birth. The degree of dilatation of the uterine pharynx and the condition of the cervix are assessed.
- Instrumental recording of fetal heart rate. Allows you to determine the presence of signs of hypoxia.
- General urine analysis. Based on its results, kidney function and the possibility of developing gestosis, which poses a great danger to the fetus, are assessed.
- Determination of blood pressure, heart rate, body temperature. Allows you to obtain information about the general health of a woman.
To establish the presence or absence of urogenital infections, bacteriological urine culture is performed. In any trimester, chlamydia, ureaplasma, and staphylococcus are very dangerous for a pregnant woman.
Pain and its prevention
The most common cause of pain in the 22nd week of pregnancy is increased stress on the spine and back muscles due to an enlarged abdomen and a shift in the body’s center of gravity.
To relieve and prevent pain, the following measures should be taken:
- Limit long walking and physical activity;
- Choose a comfortable chair with an orthopedic back and use only it;
- Do not wear high-heeled shoes or shoes with completely flat soles;
- Do not sit continuously for more than an hour;
- Perform a daily set of gymnastics exercises for pregnant women.
Lower back pain may be a sign of diseases of the urinary system, which experiences increased stress during this period. These are pyelonephritis, urolithiasis, complications of cystitis. If a woman is seen in a antenatal clinic, the manifestations of these pathologies will certainly be reflected in urine tests. A gynecologist will recommend treatment from a urologist, because kidney problems are extremely dangerous for the normal course of pregnancy and childbirth.
Another problem during this period of pregnancy is hemorrhoids, which arise due to the fact that the pregnant uterus compresses the blood vessels and impairs the blood supply to the pelvic organs. To treat it, suppositories are used, which should be selected by a specialist taking into account the woman’s condition. To stimulate intestinal motility, it is advisable to use foods high in fiber in the diet.
What causes nagging, aching pain during pregnancy?
Often pregnant women feel two types of pain:
- Pulling.
- Aching.
The onset of the first occurs most often due to false contractions (Braxton-Hicks) or, as they are also called, training contractions.
Usually, in the second trimester they begin in second-time women. They are safe for the expectant mother and fetus. The body is preparing for labor. You can distinguish such contractions from real ones by the interval and time.
They last from 20 seconds to two minutes. There may be several short contractions within an hour, then after an hour or half an hour. In most cases, the discomfort goes away when the pregnant woman’s body position changes.
The latter arise due to changes in hormones. The fetus is developing and its volume is increasing. The uterus puts pressure on the organs: stomach, intestines, bladder.
Excessive activity of the baby also affects the condition of the expectant mother. The position of the child in the womb, which is inconvenient for a woman, causes discomfort.
A growing belly increases the load on the lumbar spine, as the center of gravity shifts. This causes a burden in the lower back, often radiating downwards.
It is worth paying attention to the divergence of the symphysis pubis during the second and third trimester - the load on the skeleton is the highest. This is a natural process, but excessive softening of the ligaments causes severe pain. Doctors prescribe a caesarean section. The child is not in any danger from the pathology.
Several options for dysfunction of the symphysis pubis, depending on the width of the gap between the bones:
- Symphysiopathy – distance up to 0.5 cm.
- Symphysiolysis is a gap of more than half a centimeter.
- Symphysitis is inflammation of a semi-joint after its rupture.
If it is impossible to endure, the pain does not go away and is accompanied by the presence of bloody or other discharge, call an ambulance and do not self-medicate. Such symptoms threaten termination of pregnancy. To improve well-being, therapy with hemostatic drugs is prescribed.
The doctor determines the nature of the pain. Any discomfort should be reported to your gynecologist.
Intimate relationships
Due to the increased blood supply to the pelvic organs, a woman at week 22 may experience increased sexual desire. You should not refuse sex out of fear for the health of the fetus. It is reliably protected by the uterus and amniotic fluid from external physical influence.
Contraindications to intimate contacts during this period:
- Low placentation;
- Increased tone of the uterus;
- Pregnancy with twins;
- Inflammatory diseases of the reproductive organs;
- Risk of miscarriage.
The gynecologist will definitely tell you about these contraindications.
What does a baby look like at 22 weeks of pregnancy?
The fetus at 22 weeks is characterized by a height of about 30 cm, but it weighs closer to half a kilogram. The baby’s brain is improving, and a baby at 22 weeks is characterized by active exploration of the world around him. At the same time, he is not at all embarrassed that it is mainly the umbilical cord and amniotic sac. The main way of cognition, naturally, is touch. He actively touches his face, head, body, loves to suck his finger, tilts his head to the sides. Due to the fact that the fetus develops at the 22nd week of pregnancy in an aquatic environment, it is easier for it to literally fold in half in order to reach, for example, its toes.
The baby also continues to actively respond to sounds and tastes. Now the baby’s liver is actively working. At the same time, it performs functions that after childbirth it will no longer be able to do - it processes indirect bilirubin into direct bilirubin. It is important to understand here that the indirect version of the substance is a toxic waste product from the breakdown of hemoglobin. In the fetal liver it is neutralized and converted into a calmer version, and then easily excreted through the placenta.
The development of the fetus at week 22 is also characterized by the fact that its spine is already fully formed.
How to organize proper nutrition
To control your weight, you should properly plan your daily diet. The source of complete protein is lean meat, fish, and dairy products. To replenish calcium reserves, you should more often include kefir, fermented baked milk, hard and soft cheeses, cottage cheese, and natural yogurts in your menu. These same products with the additional consumption of prunes, dried apricots and other dried fruits will help solve the problem of constipation.
To prevent edema, you need to consume less salt, which retains water in the body. Marinades, pickles, and smoked foods should be excluded from the diet, since increased levels of salt are used for their preparation.
Sweets, sugar, and baked goods made from wheat flour are foods high in carbohydrates. They contribute to excessive weight gain and can trigger the development of diabetes mellitus in pregnant women. It is better to include sources of carbohydrates such as cereal, bran bread or whole grain bread in your diet.
An obligatory part of the menu is vegetables and fruits, which are consumed both fresh and stewed, boiled and baked. It is best to eat fractionally - in small portions, but often, including the most high-calorie foods in the breakfast and lunch menu.
Possible complications
Despite the fact that the 22nd week of pregnancy is considered a favorable period, the possibility of complications cannot be ruled out. The main danger is edema, which can be both external and internal. External swelling is visible visually, while internal swelling can be identified by rapidly increasing body weight.
With the development of gestosis, the likelihood of hypoxia and premature birth increases. Ignoring and late diagnosis of gestosis can lead to serious consequences for both mother and fetus.
Rapid weight gain and the appearance of edema require additional diagnostics. If protein is detected in the urine, a diagnosis of gestosis is made. With this pathology, the patient is often hospitalized.
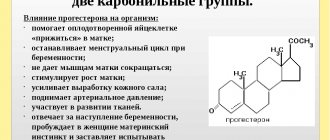
Throughout pregnancy, a physiological decrease in immunity is observed due to the influence of the hormone progesterone. This mechanism is provided by nature to prevent miscarriage. The growing fetus is only half related to the mother's body, which causes a corresponding reaction from the immune system.
Reduced immunity leads to frequent ARVI. This is why it is important to avoid places with large crowds of people. You should visit the clinic only when necessary.
Since all organs and systems of the fetus are already formed, acute respiratory viral infections do not pose a threat. However, high temperature sometimes causes disruption of the blood supply to the placenta.
Medicines should be taken only after they have been prescribed by a doctor. There are medications, including antibiotics, that are approved during pregnancy.
Cervical incompetence often requires taking the drug Utrozhestan, starting in the first trimester. The dosage of the medication at 22 weeks may be reduced.
Symptoms of hemorrhoids often appear in the second trimester. According to statistics, about 70% of women observe signs of hemorrhoids. This pathology is dangerous due to the risk of nodes falling out and bleeding. A sensitive issue cannot be ignored. The doctor will select an adequate treatment regimen that will help quickly and effectively eliminate painful symptoms.
At 22 weeks of pregnancy there is a risk of premature birth. The survival rate at this stage of pregnancy is quite insignificant. That is why a woman needs to be especially attentive to her well-being, undergo timely examinations and follow the doctor’s recommendations. If necessary, there is no need to refuse hospitalization.