Symptoms of melanoma are a set of indicators according to which ordinary moles on the body, which everyone has, are beginning to degenerate or have already degenerated into a malignant tumor. The appearance of melanoma depends on its type and stage; superficial spreading, acral lentiginous, nodular melanomas and lentigo are known.
More than 20% of melanomas belong to the superficial spreading variety. However, patients rarely live more than 5 years. However, with timely and high-quality treatment, life expectancy can be significantly increased, and for this it is important to know what melanoma itself looks like in order to recognize it in time.
Manifestations in the early stages
Melanomas can appear on any part of the body, but most often the tumors are located on the legs or back. Melanoma can also appear on the palms, mucous membranes of the mouth, vagina, rectum, and scalp. In aging skin, melanomas often manifest in the facial area.
Subungual or acrolentiginous variety
In 3% of all diagnosed cases of melanoma, specialists identify cancer of the nail plates. This disease has its own specific symptoms, which include the appearance of a tumor on the finger, darkening of the nail or the appearance of a clear dark stripe on it, cracking of the nail plate over time with the release of sanguineous fluid or pus. It is important to know that nail melanoma most often occurs in the area of the thumb. As it grows, the tumor changes color to bluish-red or black and its shape to mushroom-shaped.
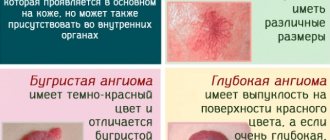
Cutaneous melanoma
The symptoms of cutaneous melanoma are determined by the naked eye, so you should always pay attention to your own health so as not to miss changes in the development of a mole and seek medical help in a timely manner. The main symptom of melanoma manifestation is the degeneration of a mole (nevus). This degeneration can be expressed in different forms, for example, the mole may begin to enlarge, its contour becomes jagged and asymmetrical, the pigmentation color darkens or acquires blue or reddish shades, itching occurs in the area of the formation, as well as swelling or wet discharge. Against the background of the above symptoms, regional lymph nodes may enlarge.
A mole can begin to degenerate after an injury, or for no apparent reason. Most often, hair falls out in the pigmentation zone, the skin begins to peel off and form crusts, and the skin pattern on the surface can no longer be read. It is also possible that melanoma satellites – skin rashes near the tumor site – may occur. The mole becomes very smooth and acquires a mirror-like surface.
Ocular variety
Melanoma of the eye is very common. Its peculiarity is the absence of symptoms in the first stages of pathology, which greatly complicates the course and treatment of the disease. The patient should be alerted to symptoms such as:
- sudden deterioration of vision;
- the appearance of photopsia or colored dots, sparks before the eyes;
- the occurrence of metamorphopsia or distorted perception of spatial and dimensional quantities;
- change in pigmentation in the iris;
- the appearance of “blind spots” in the field of vision;
- swelling in the eye area;
- retinal clouding.
Symptoms of ocular melanoma may occur even before the oncology is fully formed and do not allow an accurate diagnosis to be made. With different localization of this disease, hemorrhages in the eye area, secondary glaucoma, and retinal detachment may also occur.
Course and treatment of the disease in children, pregnant and lactating women, the elderly
Children. Pigmentless melanoma in children is extremely rare - only 0.3% of all cancers. Usually at this age it develops due to congenital nevi, often after injury. The risk group includes children with blond hair and eyes, with many birthmarks on the body. The malignant process progresses rapidly. The stages of the disease depend on the depth of tumor germination and metastases. Early symptoms are mild. The first thing a doctor may notice is inflammation of the lymph nodes. The main treatment method is surgery; as the disease progresses, radiation and chemotherapy are used. The prognosis for recovery is positive only in the initial stages of melanoma.
Pregnancy and lactation. It has been proven that nevus cells, or birthmarks, are sensitive to estrogen, that is, hormonal changes can activate the pigment system. Therefore, during pregnancy and lactation, an increase in melanomas is sometimes observed. If a woman’s mole shape changes, local vasodilation occurs, and the mole itself begins to bleed and peel, you should immediately consult a doctor. Treatment of melanoma in an expectant mother depends on the advanced stage of the cancer process. In stage 1, termination of pregnancy is not indicated—the patient has the tumor excised under anesthesia. Starting from the 2nd stage of malignant lesions, experts strongly recommend induced abortion or childbirth. This is connected not only with the progression of melanoma, but also with a direct danger to the fetus - atypical cells can metastasize through the placental barrier, giving metastases in the body of the unborn child in utero. The principles of treatment and prognosis for survival during this period do not differ from the generally accepted ones.
Advanced age. Most often, amelanotic melanoma is diagnosed in old age. Usually its development begins from acquired nevi. The disease is characterized by a rapid course and a high risk of complications. Each patient needs an individual approach. All therapeutic measures are carried out taking into account the patient’s health restrictions and contraindications. The prognosis for survival is poor.
How does amelanotic melanoma manifest?
Pigmentless or achromatic melanoma is a rare, but no less dangerous disease. Its first signs can be considered the appearance of a small bump on the skin, which quickly begins to grow. Outwardly, such a formation may resemble a wart and does not attract much attention to itself, since its color completely matches the skin tone. As achromatic melanoma grows, it may become slightly pinkish or whitish in color with a rough surface and peeling epithelial scales. The skin at the site of the tumor becomes rougher. Sometimes the appearance of such melanoma resembles a scar without a clear edge. Pressing on the tumor does not cause any discomfort, which makes many patients not pay attention to it.
In shape, non-pigmented melanomas can be flat or dome-shaped. The second form is caused by the vertical proliferation of cells, which leads to a more voluminous size compared to a flat one. The main feature of such a tumor is its uneven growth with obvious asymmetry, uneven edges and compaction of the structure. However, with the nodular form of achromatic melanoma, the symmetry of the neoplasm and evenness of color are preserved.
When such melanoma grows enough, it begins to cause discomfort to a person, which is expressed in pain, itching, swelling, and redness of the tissues. The surface of the neoplasm may crack, bleed, and form ulcers. All this indicates the progression of melanoma to late, severe stages that are practically untreatable.
An alarming sign of a neoplasm is hair loss from its surface, which indicates malignancy of the pathology. It is also dangerous to detect enlarged regional lymph nodes.
Forecasts
Because there are different types of melanomas, prognoses also vary. They are influenced by several factors: location of the tumor, growth pattern, stage of the disease. So, in the first stage the survival rate is 90%, and in the fourth, on the contrary, 90% is fatal. The prognosis for melanoma on the mucous membrane is also disappointing.
Indications for regional lymphadenectomy for primary cutaneous melanoma
Localization of the primary tumor
Risk factors for metastasis
Required number to complete
Rate of expected metastasis
Head and neck
Male gender Age 50-69 Localization in the temporal lobe Thickness 3.0 mm or more IV-V Clark
Upper limbs
Ulceration Tumor thickness 4.0 mm or more V Clark
Torso
Male gender De novo melanoma Ulceration Thickness 2.0 mm or more III-IV Clark
Lower limbs
Male Age 40-59 years Localization on the foot Thickness 3.0 or more Level IV-V Clark
Signs of metastasis in the final stages
Melanoma metastases usually occur in the following cases:
- if the patient is elderly;
- with complications of melanoma by chronic diseases;
- when melanoma cells grow into the walls of other organs;
- with a large size of primary melanoma.
Signs of liver metastases
When metastases are localized in the liver structures, black melanin accumulations form in them, representing the affected areas. In this case, functional or physical disorders occur in the liver, the consequences of which are felt by the entire body.
The main signs that melanoma has metastasized to the liver are:
- tuberosity of the organ;
- increase in liver size;
- sudden weight loss;
- presence of jaundice or ascites;
- pain in the right hypochondrium;
- nausea and vomiting;
- enlarged spleen;
- frequent nosebleeds.
Metastases in the lungs
The initial phase of pulmonary metastases does not have pronounced symptoms. In this case, there will be general signs of cancer problems in the body such as apathy, anemia, weakness, weight loss, decreased appetite, hyperthermia. Signs of metastases may initially include various colds - bronchitis, flu, pneumonia. Sometimes symptoms of lung metastases in melanoma occur only at the final stage of the disease, when nothing can be done to alleviate the patient’s condition. In this case, multiple nodular formations with involvement of the pleura and bronchi are diagnosed in the lungs.
If a large part of the lung is affected or the bronchi are compressed due to metastases, the patient experiences shortness of breath. The cough with metastases is predominantly nocturnal and dry, then gives way to ulcerations of mucopurulent sputum, odorless, but often with traces of blood. As metastases grow, the bronchi narrow and the sputum thickens, becoming purulent. Pulmonary hemorrhage may occur.
Pulmonary metastases, which affect the pleura, spine and ribs, cause pain. If metastases reach the lymph nodes of the left part of the mediastinum, hoarseness and aphonia appear, and with right-sided damage to the lymph nodes, the upper part of the body may swell due to compression of the superior vena cava.
Metastases in lymph nodes
Metastases in melanoma most often occur at stages 2-3 of the disease. The most common site for metastasis is the lymph nodes. Moreover, if a patient has a single metastasis to a lymph node, then, according to doctors’ forecasts, he will live another 5 years in 51% of cases. With 4 metastases in this area, only 17% of patients will overcome the five-year mark.
Signs of lymph node metastasis in melanoma are:
- sudden loss of body weight;
- causeless enlargement of lymph nodes;
- visual impairment;
- constant fatigue and chronic feeling of tiredness.
Metastases in bones
Metastasis to the bones is considered a very common phenomenon in melanoma in medicine, which gives severe pain to patients. The main manifestations of this process can be hypercalcemia, bone fragility, neurological changes, and compression of the bone marrow. Metastases to the bone come from the primary site, but other tumors can also be the cause, such as soft tissue sarcoma, ovarian tumors, etc. Melanoma most often affects the bones of the pelvis, hips, vertebrae, and ribs. Metastases follow from melanoma to the bones of the skull along the venous vertebral plexuses.
Nature has protected the skull bones with the ability to constantly renew themselves through osteoclasts and osteoblasts, but the entry of melanoma cells through the bloodstream into the bone marrow destroys these structures. The result of this is constant fractures of the skeleton in different parts, even under small loads.
Metastasis in the brain
Melanoma causes metastases to the human brain more often than other cancer pathologies. After this, there is no need to wait for a complete cure of the disease. The chances of survival for a patient with such metastases are significantly reduced. However, sometimes modern therapy with monoclonal antibodies helps to stop this process if there are individual characteristics of the human body.
Metastases to the brain area occur in 45% of all patients suffering from late-stage melanoma. This ultimately leads to the death of the patient. The symptoms of such metastasis will depend on the location of the lesion, necessarily including incoordination of the patient’s own body, emotional instability, headaches, fever and fever, memory loss, personality changes, lethargy, changes in pupil size, general weakness and difficulty in speech skills.
If the metastases have affected the frontal part of the brain, then the patient may experience sudden changes in rudeness, he begins to swear, and experience disturbances in visual functions and the musculoskeletal system. The symptoms of such metastases are very individual and sometimes they can completely change the patient’s personality.
When the patient's brain stem metastasizes, bursting or dull intracranial pain occurs in the head, which leads to dizziness and impairs visual functions. Also, such metastasis causes constant nausea and vomiting in the patient, convulsions, which in manifestations resemble epileptic seizures.
Diagnostics
Detection of amelanoma is complicated by its external signs. Diagnosis can be difficult if the malignant process is located in hard-to-reach places, such as on the back. If a neoplasm is detected that visually has common symptoms with melanoma, it is recommended to consult with an oncodermatologist.
To confirm the suspected diagnosis, a specialist may prescribe the following examination methods:
- Dermatoscopy. The doctor examines the affected area with a magnifying glass or dermatoscope, examining the tumor for possible signs of melanoma. If a specialist suspects a malignant process, he will take a scraping from the tumor for further research.
- Histology. Tissues from the lesion must be studied for atypical cells. Based on this technique, a final diagnosis is made.
- Ultrasound, MRI, CT and radiography. Prescribed separately or in combination. Necessary for searching for metastases in the body.
- Tumor markers. Melanoma does not have a specific antigen. Despite this, when diagnosing a tumor, a test for the S-100 protein is prescribed. It is found in elevated concentrations in the blood of people suffering from skin cancer. Its detectable amount directly depends on the stage of the oncological process. At the 1st and 2nd stages of melanoma development, the increase in S-100 may be absent or insignificant; in the 3rd and 4th phases, its concentration in the blood increases by at least 70%. Thus, this tumor marker will not help identify the disease at its very beginning, but in combination with other research methods it contributes to an accurate diagnosis.
Well-being when sick
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Typically, the early stages of melanoma do not cause the patient any inconvenience, discomfort, or pain. After stage 3, when metastases occur, pain begins to appear, and with the onset of stage 4, anemia, weakness, frequent cough, aching bones, exacerbation of chronic pathologies, enlarged lymph nodes, loss of appetite, headaches, nausea, vomiting, and convulsions are added to it. . Depending on the location of metastases, memory loss may occur, vision may deteriorate, and constant pain in the skeleton, right hypochondrium, and chest space may occur.
The danger of melanoma lies precisely in the fact that the patient practically does not feel the most treatment-friendly stages, so he is in no hurry to seek help, and when metastases occur and the melanoma can no longer be cured, the patient begins to be bothered by all sorts of unpleasant symptoms, which have to be dealt with make significant efforts. In general, the state of health in patients with melanoma in late stages is negative, which further depresses already exhausted people faced with oncology.
Symptoms
By knowing the characteristic signs of melanoma that appear in the early stages, you can protect yourself from the consequences of metastatic cancer. The reason for contacting a specialist and initiating diagnostic measures should be any change in the body of a mole, nevus or pigment spot. Symptoms of the beginning of the degeneration of a benign tumor into a malignant tumor can be:
- Changes in the shape of pigmentation (asymmetry).
- An increase in the size of a mole (a mole over 5 mm in diameter should alert you).
- The appearance of unevenness and blurred edges of the problem area.
- Darkening or uneven coloration.
- Itching, burning, redness around the mole, peeling and cracking of the surface.
- Disappearance of skin pattern.
- Compaction or softening of the structure of the formation.
The initial stage of skin cancer is manifested by local changes on the skin and does not yet have a systemic effect on the body. With further development of the disease, symptoms are supplemented by headache, general weakness, fatigue, loss of appetite, and weight loss.
In medicine, the following types of melanoma are distinguished:
- Superficially spreading.
- Nodal.
- Lentiginous.
- Acral-lentiginous.
- Pigmentless.
The situation is more difficult with diagnosing non-pigmented melanoblastoma in the early stages, since the external manifestations of cell degeneration are less noticeable in contrast to pigmented areas.
Signs of a mole degenerating into melanoma
Signs of degeneration of harmless birthmarks into malignant melanoma are such phenomena as itching, burning in the area of the mole, skin tension at the base of the nevus, bleeding of unaffected moles, tingling at the site of the birthmark, cracks in the mole and ulcerations from it.
To determine whether a person has signs of a mole degenerating into melanoma, experts have come up with a special system for assessing the condition of a mole, which is called the “melanoma chord”, where A is the asymmetry of the neoplasm, K is the unevenness of the edge of the birthmark, K is the bleeding of the mole, O is the uniformity color, P – large size of the neoplasm, D – dynamics of the condition of a mole of any nature.
By assessing the above indicators, you can conclude that the mole is unstable and promptly contact an oncologist for qualified help.
Treatment after surgery
For local stages, observation is carried out for 5 years. 10 years – for other forms. This period is considered sufficient to detect the occurrence of a relapse of the disease. The patient is instructed to use appropriate means of protection against UV rays, in conditions of natural and artificial radiation.
Author's publication: IVAN GEORGIEVICH GAFTON, oncologist, National Medical Research Center of Oncology named after N.N. Petrova
Photos from the personal archive: RAJABOVA ZAMIRA AKHMEDOVNA oncologist, head of the surgical department of head and neck tumors, National Medical Research Center of Oncology named after. N.N. Petrova