If we translate the term “scleroderma” literally, it turns out that this name hides a disease in which the skin becomes sclerotic, that is, thickens, loses its original structure, and the nerve endings inside it die.
Focal scleroderma is a pathology belonging to the class of systemic connective tissue (it also includes lupus erythematosus, Sjogren's syndrome and some others). Unlike systemic scleroderma, in the case of the development of this subtype, internal organs practically do not suffer. Also, this form of pathology has a better response to treatment and may even disappear completely.
The essence of pathology
With focal scleroderma, the “matter” suffers, from which the supporting frames of all organs are built, ligaments, cartilage, tendons, joint capsules, intercellular “layers” and fatty “seals” are formed. Despite the fact that connective tissue can have different states (solid, fibrous or gel-like), the principle of its structure and the functions it performs are approximately the same.
Human skin is also partially composed of connective tissue. Its inner layer, the dermis, allows us not to get burned by ultraviolet rays, not to get blood poisoning when microbes inevitably enter from the air, and not to become covered with ulcers when in contact with aggressive substances. It is the dermis that determines the youth or old age of our skin, makes it possible to make movements in the joints or show our emotions on the face, without then having to deal with the long-term restoration of the appearance from folds and cracks.
The dermis consists of:
- individual cells, some of which are responsible for the formation of local immunity, others for the formation of fibrils and amorphous substance between them;
- fibers (fibrils), which provide the skin with elasticity and tone;
- vessels;
- nerve endings.
Between these components lies a gel-like “filler” - the previously mentioned amorphous substance, which ensures the skin’s ability to immediately return to its original position after the work of facial or skeletal muscles.
Situations may occur when immune cells located in the dermis begin to perceive some other part of it as a foreign structure. Then they begin to produce antibodies here that attack fibroblast cells that synthesize dermal fibers. Moreover, this does not happen everywhere, but in limited areas.
The result of an immune attack is an increased production of one of the fibers by fibroblasts - collagen. Appearing in excess, it makes the skin dense and rough. It also “braids” the vessels inside the affected areas of the dermis, which is why the latter begin to suffer from a lack of oxygen and nutrients. This is what focal scleroderma is.
What is scleroderma?
Scleroderma (also known as systemic sclerosis ) is a chronic disease that causes thick and hard skin, scar tissue, and damage to internal organs such as the heart and blood vessels, lungs, stomach, and kidneys. The symptoms of scleroderma vary widely from minor to life-threatening, depending on how widespread the disease is and what parts of the body are affected.
Dangers of the disease
Existing in a limited area of skin and being promptly diagnosed and treated, the pathology does not pose a threat to life. It only contributes to the formation of a cosmetic defect, which can be eliminated by dermatological and cosmetological methods. But how dangerous is focal scleroderma if you don’t pay attention to it?
This pathology can:
- cause the appearance of dark areas on the skin surface;
- provoke the development of vascular networks (telangiectasia);
- lead to chronic Raynaud's syndrome associated with impaired local microcirculation. It manifests itself in the fact that in the cold a person begins to experience pain in the fingers and toes; at the same time, the skin of these areas sharply turns pale. When warming up, the pain goes away, the fingers first turn purple, then acquire a crimson tint;
- be complicated by calcification, when small and painless “nodules” appear under the skin, having a rocky density. These are deposits of calcium salts;
- spread to extended areas of the skin. In this case, collagen fibers compress the sweat and sebaceous glands located in the dermis, and this leads to disruption of the body’s thermoregulation;
- develop into a systemic form of scleroderma, causing damage to internal organs: the esophagus, heart, eyes and others.
Therefore, if you find symptoms of pathology (they will be described below), contact a rheumatologist to find out how it is treated.
How is the disease diagnosed?
There are no specific tests that can confirm or refute scleroderma. The diagnosis is made based on the results of a comprehensive examination of the body. Data is important:
- general blood test - detect anemia and changes in erythrocyte sedimentation rate;
- immunological studies - antibodies to collagen, vascular epithelium, rheumatoid factor are present;
- Dopplerography – reflects the degree of vascular sclerosis;
- capillaroscopy – allows you to assess peripheral blood supply;
- skin biopsies reveal fibrosis;
- biochemical blood test - reflects the degree of damage to internal organs;
- general urinalysis - provides information about the condition of the kidneys.
The disease is treated by several specialists at once - a rheumatologist, an immunologist, an endocrinologist, with mandatory supervision by doctors of other specializations (orthopedist, gastroenterologist, nephrologist, hepatologist).
Who gets sick more often
Scleroderma, which has only focal manifestations, is more often found in females. Girls get it three times more often than boys; pathology can be detected even in newborns, and by the age of 40, women make up ¾ of all patients with scleroderma. The “love” of scleroderma for the fair sex is connected with the fact that:
- cellular immunity (these are the cells that themselves, not with the help of antibodies, destroy foreign agents) is less active in women;
- the humoral (antibody-mediated) component of immunity has increased activity;
- female hormones have a pronounced effect on the functioning of microcirculation vessels in the dermis of the skin.
Symptoms
Symptoms of scleroderma are quite extensive and depend on the form and severity of the disease. The main manifestations include:
- General weakness
- Shortness of breath
- Increased fatigue
- Dry cough
- Drastic weight loss
- Slight increase in body temperature
- Swelling of the skin, change in color
- The appearance of compactions in the form of pale plaques
- Thinning of the skin
- Atrophy of the mucous membranes
- Joint pain, impaired mobility
- Numbness in fingertips, burning, blueness, or paleness
- Muscle pain
- Curvature of the phalanges of the fingers
- Pain in the heart and limbs
- Arrhythmia
Causes of the disease
The exact cause of the pathology is unknown. The most modern hypothesis states that focal scleroderma occurs as a sum of:
- entry of infectious agents into the body. A significant role is attributed to the measles virus, viruses of the herpes group (herpes simplex, cytomegalovirus, Epstein-Barr virus), papillomatosis virus, as well as staphylococcal bacteria. There is an opinion that you can get scleroderma as a result of having scarlet fever, tonsillitis, or Lyme disease. DNA from Borrelia Burgdorferi, which causes Lyme disease, or antibodies to it are observed in blood tests of most patients with focal scleroderma;
- genetic factors. This is the carriage of certain receptors on immune cells-lymphocytes, which contribute to the chronic course of the above infections;
- endocrine disorders or physiological conditions in which hormonal levels change dramatically (abortion, pregnancy, menopause);
- external environmental factors that most often trigger “dormant” scleroderma or aggravate the disease, which was previously hidden. These are: stress, hypothermia or overheating, excess ultraviolet rays, blood transfusion, trauma (especially traumatic brain injury).
It is also believed that the triggering factor for the appearance of scleroderma is tumors present in the body.
The opinion of domestic scientists led by L.A. Bolotnaya, who studied changes in skin cells that appear during focal scleroderma, is also important. They believe that the development of this pathology can be triggered by a decrease in magnesium content in the blood, which causes calcium to accumulate in red blood cells and disrupt the functioning of a group of enzymes.
Find out more about the disease in the article “What is scleroderma.”
Who is at risk
Women aged 20-50 years are most at risk of developing focal scleroderma, but men are also at risk:
- blacks;
- those who already have other systemic connective tissue diseases;
- whose relatives suffered from one of the systemic connective tissue pathologies (lupus erythematosus, rheumatoid arthritis, dermatomyositis);
- workers of open markets and those people who sell goods from street stalls in winter;
- builders;
- persons who are forced to frequently take refrigerated goods from freezers;
- those who guard food warehouses, as well as representatives of other professions who are often forced to become hypothermic or expose their hands to chemical mixtures.
Etiology of scleroderma
The exact cause of the disease has not yet been established. Presumably, hereditary pathologies play a major role here. Nevertheless, it is reliably known that the following factors have a significant influence on the development of scleroderma:
- Gene mutation. This may include ultraviolet or ionizing radiation, exposure to radioactive substances, working with pesticides, nitrates, etc. The list is quite extensive, it even includes food additives, as well as cytostatics (a group of drugs).
- Infectious factor, that is, the penetration of pathogenic microorganisms, leading to inflammatory diseases.
- Various disorders of the immune system.
- Negative environmental factors, for example, living next to a large plant.
- Exposure to chemicals. This most often occurs due to the use of certain medications, such as heparin, pentazocine or bleomycin.
Classification
Focal scleroderma can be:
1. Plaque (discoid). It has its own division into:
- superficial;
- deep (nodular);
- indurative-atrophic;
- bullous (a bulla is a large bubble filled with fluid);
- generalized (throughout the body).
2. Linear:
- as a “strike with a saber”;
- strip-shaped;
- zosteriform (similar to the blisters of herpes zoster or chickenpox).
3. White spot disease.
4. Idiopathic, Pasini-Pierini, atrophy of the dermis.
Diagnostics
To establish the correct diagnosis, the doctor listens to the patient’s complaints, studies the medical history, and conducts a general examination. Laboratory tests such as blood collection, urine collection, biopsy are prescribed, special immunological studies are carried out, and antibodies are determined. Additionally, capillaroscopy, X-ray, ultrasound, Dopplerography, spirometry, computed tomography, ECG, Holter monitoring are performed. You may need to consult with specialized specialists, namely a rheumatologist, cardiologist, dermatologist and others.
How does the disease manifest itself?
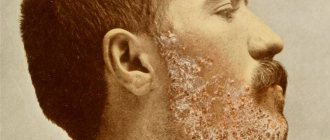
The first symptoms of focal scleroderma appear after Raynaud's syndrome has existed for several years. Also, specific scleroderma signs can be preceded by peeling of the skin of the palms and feet, the appearance of spider veins in the cheek areas (if the lesion appears on the face).
The first symptom of focal scleroderma is the appearance of a lesion:
- looks like a ring;
- small sizes;
- violet-red color.
Further, such a lesion changes and becomes yellow-white, shiny, and cooler to the touch. The “rim” around the perimeter still remains, but the hair begins to fall out and the lines characteristic of the skin disappear (this means that the capillaries are no longer functioning well here). The affected skin surface cannot be folded; she does not sweat and does not become covered with sebaceous gland secretions, even if the surrounding skin is oily.
Gradually, the purple “ring” disappears, the whitish area is pressed in and is located below the healthy skin. At this stage, it is not tense, but soft and pliable to the touch.
Plaque form
The second main type of pathology is linear scleroderma. It occurs most often in children and young women. The difference between linear scleroderma and plaque scleroderma is visible to the naked eye. This:
- a strip of yellowish-white skin;
- shaped like a stripe from a saber strike;
- most often located on the torso and face;
- may cause atrophy (thinning, paleness, hair loss) on half of the face. Both the left and right half of the face may be affected. The skin on the affected half becomes bluish or yellowish, first thickens, and then atrophies, and the subcutaneous tissue and muscles also undergo atrophy. Facial expressions in the affected area become inaccessible; it may seem that the skin is “hanging” on the bones of the skull;
- may occur on the labia, where it looks like whitish-pearl-colored lesions of uneven shape, surrounded by a bluish “rim”.
Linear form
Facial lesions in linear scleroderma
Pasini-Pierini disease is a series of purple-lilac spots with a diameter of about 10 cm or more. Their outlines are irregular, and they are most often located on the back.
The transition from a focal form of scleroderma to a systemic one can be suspected based on the following criteria:
- a person fell ill either before the age of 20, or after 50;
- there is either a linear form of pathology, or there are many plaques;
- foci of scleroderma are located either on the face or in the area of the joints of the legs and arms;
- In a blood test for an immunogram, cellular immunity is impaired, the composition of immunoglobulins and antibodies to lymphocytes is changed.
Fast Facts
- Scleroderma manifests itself differently in each person, but can be very dangerous.
- There are medications as well as steps that people with scleroderma can take to relieve the symptoms of Raynaud's disease, skin problems, and heartburn.
- Effective treatments are available for people with serious illnesses, including acute kidney disease, pulmonary hypertension, pneumonia, and gastrointestinal problems.
- It is important to recognize and treat organ damage early to prevent permanent damage.
- Patients should see a doctor who specializes in treating this complex disease (rheumatologist).
Scleroderma is an autoimmune disease that affects the skin and other organs of the body . This means that the body's immune system causes inflammation and other problems in these tissues.
The main finding with scleroderma is thickening and hardening of the skin, as well as inflammation and scarring of many parts of the body, leading to problems in the lungs, kidneys, heart, intestinal system and other areas. There is no cure for scleroderma yet, but there are effective treatments for some forms of the disease.
Scleroderma is relatively rare. Approximately 75,000 to 100,000 people in Russia have the disease; Most of the patients are women aged 30 to 50 years. Twins and family members with scleroderma or other autoimmune connective tissue diseases such as lupus may have a slightly higher risk of developing scleroderma. Children can also develop scleroderma, but the disease is different in children than in adults.
Although the underlying cause is unknown, promising research is shedding light on the connection between the immune system and scleroderma. There is also a lot of research going on to find the best treatment for scleroderma.
Treatment
First, we will answer the question of whether focal scleroderma is curable, in the affirmative. Before skin atrophy occurs over a large area, the disease can be stopped with several courses of drugs for local and systemic use.
Treatment of focal scleroderma begins with the following systemic medications:
- Antibiotics of the penicillin group. They must be drunk during the first 3 courses.
- Injections of drugs that improve vascular function. First of all, these are products based on nicotinic acid, which dilate capillaries, reduce their thrombosis and the formation of cholesterol plaques in large vessels. The second are drugs that prevent platelets from “clogging” the capillaries: Trental.
- Calcium current blockers (Corinfar, Cinnarizine). These medications relax the smooth muscles of blood vessels, improve the penetration of necessary substances from the vessels into the cells of the skin, muscles and heart.
Also, for focal linear scleroderma, local treatment with ointments is used. It is recommended to apply not one, but several of these local products, with different directions, at different times of the day. So, the following are required for use:
- Solcoseryl or Actovegin are drugs that improve the utilization of oxygen by skin cells, which leads to the normalization of its structure;
- heparin, which reduces thrombus formation in blood vessels;
- Egallohit cream. This is a preparation based on green tea, which, with the help of the catechins it contains, will trigger the formation of new blood vessels at the initial stage of the disease, and in the end it will suppress this process. It also prevents the formation of an increased amount of collagen, has anti-inflammatory and antioxidant effects;
- Troxevasin gel, which strengthens blood vessels;
- Butadione is an anti-inflammatory drug.
The effect is provided by physiotherapeutic methods (phonophoresis with lidase preparations, paraffin applications, radon and mud baths), massage, hyperbaric oxygenation, plasmapheresis, autohemotherapy.
Treatment of scleroderma
Treatment Goals
- stop the progression of the disease;
- reduce the activity of the pathological process;
- reduce the area of skin lesions and the severity of clinical symptoms of the disease;
- prevent the development of complications;
- improve the quality of life of patients.
General notes on therapy
Treatment must be selected individually for each patient, depending on the form, stage and severity of the disease, as well as the location of the lesions.
Patients with plaque, generalized and linear scleroderma, as well as Pasini-Pierini atrophoderma and extragenital lichen sclerosus with shallow lesions of the skin and underlying tissues are recommended to undergo a course of drug treatment (including penicillin, hyaluronidase, vasoactive and external agents) or phototherapy (UVA-1 therapy or PUVA therapy).
For patients with an active, rapidly progressing course of the disease and severe inflammatory phenomena (mainly in the presence of linear or multiple foci of scleroderma), inclusion of systemic glucocorticosteroid drugs in complex treatment is indicated.
Patients with severe forms of localized scleroderma with the formation of deep lesions of the skin and underlying tissues (linear, generalized, pan-sclerotic scleroderma, progressive Parry-Romberg facial hemiatrophy) are prescribed treatment with methotrexate in the form of monotherapy or in combination with systemic glucocorticosteroid drugs.
In the presence of erosive and ulcerative defects and superficial skin atrophy, the use of tissue regeneration stimulators is indicated; in case of dry skin, the use of moisturizing and emollient external agents is indicated.
Sometimes spontaneous regression of skin sclerosis or complete resolution of the lesions may be observed.
Indications for hospitalization
Generalized forms of scleroderma
Treatment regimens for scleroderma:
Drug therapy
Systemic therapy
Methotrexate - For severe forms of localized scleroderma (linear, generalized, pan-sclerotic scleroderma, Parry-Romberg progressive facial hemiatrophy), an effective treatment method is the use of methotrexate as monotherapy or in combination with systemic glucocorticosteroid drugs.
According to published data, the following treatment regimens with methotrexate are effective:
- methotrexate: adults - 15-25 mg, children - 0.3-1 mg per kg body weight
- methotrexate: adults - 15-25 mg, children - 0.3-1 mg per kg body weight (maximum dose 25 mg) + methylprednisolone: adults - 1000 mg per day, children - 30 mg/kg body weight per day (maximum dose 500-1000 mg)
- methotrexate: adults - 15-25 mg, children - 0.3-1 mg per kg body weight (maximum dose 25 mg) + prednisolone 0.5-1 mg per kg body weight per day (maximum dose 60 mg.
Glucocorticosteroid drugs
Oral use of glucocorticosteroid drugs can have a positive effect in active, rapidly progressing localized scleroderma, however, after discontinuation of the drugs, the frequency of relapses is high.
- prednisolone 0.3-1 mg per kg body weight
In some cases, it is recommended to administer glucocorticosteroid drugs directly to the site of scleroderma.
- betamethasone 0.2 ml/cm2 (but not more than 1 ml)
Hyaluronidase
According to published data, the use of hyaluronidase can lead to a decrease in skin induration in scleroderma lesions:
- — hyaluronidase 32-64 UE
Hyaluronidase can also be injected into lesions by ultraphonophoresis or electrophoresis.
- phonophoresis of hyaluronidase 64 UE hyaluronidase is dissolved in 1 ml of 1% novocaine solution, applied to the lesions with a pipette and rubbed in, then covered with a contact medium (vaseline oil, vegetable oil or gel) and sounded with an oscillation frequency of 880 kHz, intensity 0.5-1 .2 W/cm2, exposure for 3-10 minutes on the field using a labile method in continuous mode.
- electrophoresis of hyaluronidase 64 UE lidase is dissolved in 30 ml of distilled water, to acidify the medium to pH 5.2, add 4-6 drops of 0.1 N. hydrochloric acid solution is injected into scleroderma lesions at a current strength of no more than 0.05 mA/cm2, exposure time is 12-20 minutes.
Ultraphonophoresis or hyaluronidase electrophoresis procedures are carried out daily or every other day, 8-12 procedures are prescribed per course. It is possible to conduct 2-3 repeated courses with an interval of 3-4 months.
Penicillamine
Several studies have established a positive effect when treating patients with localized scleroderma with penicillamine [15-17]. However, there is evidence of the absence of any improvement in the skin process when using this drug.
- penicillamine 125-500 mg
Given the fairly large number of side effects and the possibility of toxic effects even with low-dose treatment, penicillamine has been prescribed less frequently in recent years, mainly in cases of lack of effect from other therapeutic agents.
Penicillin
In clinical practice, penicillin has been used to treat localized scleroderma for several decades, although publications on the effectiveness of its use are few [19, 20].
- benzylpenicillin sodium salt 300,000-500,000 units 3-4 times a day or 1 million units 2 times a day intramuscularly
Vasoactive drugs
There is evidence of the effectiveness of using vasoactive drugs in the complex treatment of patients with localized scleroderma:
- pentoxifylline 100-200 mg
- xanthinol nicotinate 75-150 mg
- xanthinol nicotinate, solution for injection 15% (300 mg)
Therapy with vasoactive drugs is recommended in repeated courses at intervals of 3-4 months, a total of 2-3 courses per year.
External therapy
Topical glucocorticosteroid drugs
In the treatment of limited forms of localized scleroderma, the external use of glucocorticosteroids has a certain effect:
- — mometasone furoate, cream, ointment
- - alklometasone dipropionate, cream, ointment
- - methylprednisolone aceponate, cream, ointment
- - betamethasone, cream, ointment
- - clobetasol propionate, cream, ointment
When prescribing topical glucocorticosteroid drugs in the form of applications, the course of treatment is 4-12 weeks, when using them in the form of occlusive dressings - 2-3 weeks.
Topical calcineurin inhibitors.
A randomized, placebo-controlled study demonstrated the effectiveness of 0.1% tacrolimus ointment in localized scleroderma.
- tacrolimus, 0.1% ointment
Dimethyl sulfoxide
Treatment with dimethyl sulfoxide in some cases can lead to a decrease in erythema and induration of the skin in areas of scleroderma.
- dimethyl sulfoxide: the drug is dissolved in water, used in the form of applications of a 25-75% aqueous solution. Dimethyl sulfoxide therapy is carried out in repeated courses at intervals of 1-2 months.
Stimulators of tissue regeneration.
- deproteinized hemoderivative from calf blood, 5% ointment
- deproteinized hemolysate from calf blood, 5% ointment
Non-drug therapy
Physiotherapeutic treatment of scleroderma:
Far-long wave ultraviolet therapy (UVA-1 therapy, wavelength 340-400 nm)
UVA-1 therapy is one of the effective methods of treating plaque, generalized and linear scleroderma, as well as extragenital lichen sclerosus with shallow lesions of the skin and underlying tissues.
- irradiation with UVA-1 light begins with a dose of 5-20 J/cm2, subsequent single doses are increased by 5-15 J/cm2 to a maximum single dose of 20-60 J/cm2. The procedures are carried out 3-5 times a week, the course is 20-60 procedures.
PUVA therapy
PUVA therapy, both with oral and external use of a photosensitizer, can significantly improve the condition of the skin in scleroderma lesions in patients with plaque, linear and generalized forms of the disease, as well as extragenital lichen sclerosus.
PUVA therapy with oral photosensitizer
- Ammi major fruit furocoumarins 0.8 mg per kg body weight orally once 2 hours before irradiation with long-wave ultraviolet light (wavelength 320-400 nm)
- methoxalen 0.6 mg per kg body weight orally once 1.5-2 hours before irradiation with long-wave ultraviolet light (wavelength 320-400 nm).
Irradiation begins with a dose of 0.25-0.5 J/cm2, subsequent single doses are increased every 2-3 sessions by 0.25-0.5 J/cm2 to a maximum dose of 3-6 J/cm2. The procedures are carried out 2-4 times a week, the course of treatment is 20-60 procedures.
PUVA therapy with external application of a photosensitizer
- isopimpinellin/bergapten/xanthotoxin 0.3% alcohol solution applied externally once to the lesions 15-30 minutes before irradiation with long-wave ultraviolet light (wavelength 320-400 nm).
Irradiation begins with a dose of 0.1-0.3 J/cm2, subsequent single doses are increased every 2-3 sessions by 0.1-0.2 J/cm2 to a maximum value of 3.5-5 J/cm2. Procedures are carried out 2-4 times a week, the course is 20-60 procedures.
UVA-1 and PUVA therapy are carried out both as monotherapy and in combination with medications.
Ultrasound therapy for scleroderma:
In the treatment of limited forms of localized scleroderma, the use of ultrasound therapy can help reduce the intensity of clinical symptoms of the disease.
Sounding of lesions is carried out with an oscillation frequency of 880 kHz, intensity of 0.05-0.8 W/cm2, exposure of 5-10 minutes on the field using a labile technique in continuous or pulsed mode. The course is 10-15 daily procedures.
It is possible to conduct repeated courses of ultrasound therapy at intervals of 3-4 months.
Ultrasound therapy
Low-level laser therapy.
It is known that low-intensity laser therapy can improve blood microcirculation in the skin. Some studies have shown the effectiveness of low-intensity laser therapy in the complex treatment of limited forms of localized scleroderma.
- Therapy with laser radiation of the red range (wavelength 0.63-0.65 microns) is carried out using a remote stable technique, a defocused beam with a power density of 3-5 mW/cm2 and an exposure of 5-8 minutes on the field. During the procedure, no more than 4-5 fields are irradiated with a total duration of exposure of no more than 30 minutes.
- Therapy with infrared laser radiation (wavelength 0.89 microns) is carried out using a remote or contact, stable or labile technique, in continuous or pulsed (80-150 Hz) mode. The effects are carried out by field: in continuous mode, the radiation power is no more than 15 mW, exposure to one field is 2-5 minutes, the duration of the procedure is no more than 30 minutes. In pulsed mode, the radiation power is 5-7 W/pulse, exposure is 1-3 minutes per field, total exposure time is no more than 10 minutes. No more than 4-6 fields are irradiated during the procedure.
The course of laser therapy is 10-15 daily procedures. Repeated courses are carried out at intervals of 3-4 months.
Low-level laser therapy.
Therapeutic exercises and massage for scleroderma:
Therapeutic exercises and massage are recommended for patients with a linear form of scleroderma when movements in the joints are limited and contractures form.
Surgical treatment of scleroderma:
Surgical treatment is carried out in some cases in the presence of flexion contractures or cosmetic defects (with localized scleroderma of the “saber blow” type, progressive Parry-Romberg hemiatrophy). Surgical interventions are carried out in the inactive stage of the disease (in the absence of signs of scleroderma activity for several years).
Special situations
Treatment of pregnant women with scleroderma:
Treatment of pregnant women is carried out according to strictly substantiated indications, taking into account the balance of benefits and potential risks for the mother and fetus.
PUVA therapy is contraindicated during pregnancy and lactation.
Treatment of children with scleroderma:
Localized scleroderma, which arose in childhood, often lasts a long time over several years: in 30% of patients, disease activity remains active after reaching adulthood. More than 20% of patients with juvenile localized scleroderma may experience various extracutaneous symptoms (articular, neurological, vascular, ophthalmological, respiratory, etc.).
With juvenile scleroderma, there is a risk of developing a number of complications leading to disability of patients: a decrease in the length and volume of the limbs, the formation of contractures, and facial deformities. In this regard, treatment of localized scleroderma in children should be started as early as possible, with more active therapy. Thus, for patients with severe forms of the disease, it is recommended to prescribe methotrexate as a first-line therapy as monotherapy or in combination with systemic glucocorticosteroid drugs. This treatment makes it possible to achieve long-term remission of the disease (2 years or more) in 74% of patients.
UVA-1 therapy is prescribed to children only in severe forms of the disease (linear, generalized, pansclerotic) in cases where there is no effect from the use of other medications.
The use of PUVA therapy in childhood is contraindicated.
Requirements for treatment results
- reducing the activity of scleroderma;
- preventing the emergence of new and enlargement of existing lesions (cessation of disease progression);
- regression or reduction of symptoms of the disease;
- reducing the affected area;
- preventing the development of complications;
- improving the quality of life of patients.
Tactics in the absence of treatment effect
If there is no effect from the use of drugs, it is recommended to prescribe drugs from other pharmacological groups.
If there is no effect from drug treatment, it is recommended to prescribe UVA-1 therapy or PUVA therapy.
Prevention of scleroderma
Patients are advised to avoid skin trauma, hypothermia and overheating, and stressful situations.
IF YOU HAVE ANY QUESTIONS ABOUT THIS DISEASE, CONTACT DOCTOR DERMATOVENEROLOGIST KH.M. ADAEV:
EMAIL:
INSTAGRAM @DERMATOLOG_95
« Previous entry
Traditional methods
Treatment with folk remedies can complement scleroderma therapy. This:
- compress with aloe juice applied to gauze;
- a compress of dry wormwood mixed with petroleum jelly or wormwood juice mixed 1:5 with pork fat;
- ointment from tarragon mixed 1:5 with interior fat. The fat should be melted in a water bath, and together with the tarragon it should be simmered in the oven for about 6 hours;
- taken orally, 100 ml per day, decoctions of St. John's wort, motherwort, calendula, hawthorn, red clover.
Diagnosis of scleroderma
Scleroderma is diagnosed during a face-to-face consultation with a doctor. The diagnostic criteria for scleroderma are: - characteristic skin lesions that go through the stages inherent in scleroderma and are present mainly on the hands, face, and torso; the presence of persistent joint-muscular contractures; — osteolysis of the phalanges of the fingers; - typical for scleroderma damage to the heart, digestive tract, kidneys, lungs; - weight loss; - low-grade body temperature.
Laboratory diagnostics includes: urine analysis, blood test (rheumatic tests), as well as other tests. To determine heart damage, an electrocardiogram is prescribed. One of the diagnostic methods is cappilaroscopy of the nail bed.
To make an accurate diagnosis, an X-ray examination of internal organs and skin is performed.
Causes
Scleroderma sometimes occurs after severe trauma to the central or peripheral nervous system. Strong cooling is important. Sometimes there is a connection with acute and chronic infectious diseases (rheumatism, diphtheria, typhoid fever, syphilis, tuberculosis, etc.), various types of toxicosis, and severe mental experiences.
The pathogenesis of scleroderma is closely related to the endocrine-vegetative system. There are cases of combination of scleroderma with Graves' disease, less often with myxedema, as well as with lesions of other endocrine organs: adrenal gland, pituitary gland, thymus.