Already 33 weeks pregnant! The baby has taken a permanent position, his weight is increasing, the formation of all organs and systems continues, and their improvement. It is becoming more and more difficult for the baby to move, there is less and less freedom of action, so the mother notices that activity is becoming somewhat lower. The baby sleeps longer, and at this stage he begins to have dreams! During REM sleep, active movements of the eyeballs occur. Expectant mothers also note that pregnancy 33, 34 weeks is the time when they have vivid dreams.
A specific skin pattern appears on the baby’s fingers. The layer of fatty tissue increases, thermoregulation improves. Organs and systems are already so well formed that childbirth at 33 weeks of pregnancy is not so dangerous - the chances of a baby from this period are much higher.
At 33 weeks of pregnancy, the baby’s weight approaches two kilograms and his height is 43 centimeters.
33 weeks pregnant: how many months? This is already eight months plus one week. By this gestational age, the baby's body is quite mature. Then the final maturation of the nervous, respiratory and other systems occurs.
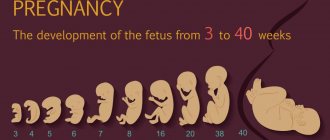
Fetal development
When the period reaches 35 weeks of pregnancy, the weight of the fetus can reach two and a half kilograms. A feature of the child’s development during this period is the formation of muscle tissue and an increase in fat deposits. During this week, the fetus can gain up to 250 g of weight.
During this period, the fetus is already fully developed. The 35th week of pregnancy is characterized by the final stage of the formation of its internal organs.
The baby's height can reach 45 cm. He becomes cramped in the womb, so his every movement causes discomfort in the woman.
All the baby's organs are fully formed. During this period, the development of the genitourinary and central nervous systems is completed.
The child’s body actively secretes hormones that help fully form the exchange of nutrients and minerals in his body.
Why may a child move little or stop doing so?
If a pregnant woman feels less than 10 kicks per day, or the baby does not move for about 3-4 hours, you should consult a doctor. In most cases, a sharp decrease in activity indicates the development of fetal hypoxia, in which embryonic movements may be absent for 12 hours. If the pathology is not detected in time, the fetus freezes.
Physiological reasons
A child may reduce activity for the following reasons:
- the woman is in a noisy room, loud sounds can frighten the embryo;
- the fetus is in a state of sleep;
- a pregnant woman goes in for sports - with active movements, vibrations of the amniotic fluid are created, and the child may fall asleep;
- childbirth is approaching.
Starting from week 28, the fetus increases in size, occupying free space inside the placenta. It becomes difficult for him to move and roll over. The cramped space limits his activity.
Symptoms
The alarming clinical picture begins with the appearance of sharp and severe pain in the lower abdomen after 12-24 hours from the moment the fetus freezes. The pain syndrome is caused by increased peristalsis of the uterus, which seeks to get rid of the dead embryo. Other symptoms include:
- increased body temperature above +39°C;
- weakness;
- pale skin;
- increased sweating;
- uterine bleeding;
- thready pulse and drop in blood pressure;
- at a later stage, the breasts return to their natural size.
If your general health worsens, you should consult your doctor for a diagnosis.
Diagnostics
Cardiotocography and ultrasound with Doppler measurements allow hypoxia to be diagnosed in a timely manner. CTG helps to count the number of heartbeats of the embryo and record them in the form of a graph. Cardiotocography additionally determines the tone of the uterus. The procedure lasts about 20-40 minutes, during which the woman presses a button when she feels the embryo kicking.
To clarify the diagnosis, the doctor performs Doppler sonography, with which he establishes the speed of blood flow in the arterial vessels of the uterus and umbilical cord. Ultrasound allows you to evaluate the movements of the embryo, the volume of amniotic fluid, and the muscle tone of the uterus. If the data obtained indicates a serious condition of the child, the doctor decides to initiate premature labor or hospitalize the woman.
Causes for concern
The first cause for alarm is the absence of tremors for 2-3 hours. If movement does not resume after 6 hours, you must call an ambulance. The baby should move at least 10 times in 3 hours before the 26th week of pregnancy. At later stages, up to 12 shocks per day can be considered normal activity. If the movements do not correspond to the norm, it is necessary to undergo an instrumental examination.
What to do if there is no movement
It is not recommended to stay home if your health worsens. If the expectant mother becomes ill or does not feel fetal kicks for more than 6 hours, urgent hospitalization and examination using ultrasound and CTG are required.
Child's appearance
The fetus at 35 weeks of pregnancy already looks like a fully formed person, because during this period there is an active accumulation of fat deposits, the baby’s skin becomes soft and smooth. Its color takes on a pink tint.
The child's figure is actively rounded. Angularity disappears. Infantile swelling appears.
The baby's weight at 35 weeks of pregnancy can reach 3 kg. You may notice the appearance of folds on the joints of the arms and legs. Active formation of the feet occurs. You can also notice baby folds in the neck area.
Each child develops individually during this period. Some babies already have hair, while others do not.
Often the child’s nails are already formed at this time. They can reach great lengths. Therefore, small scratches may appear on the baby’s cheeks.
magnesium for tone
Tell me, how much magnesium can be used to tone up? I was in the hospital, magnesium was given intramuscularly 2 times a day, then intravenously once a day for a total of 10 days. For a week everything was ok. Now at home I have the tone again 10 times a day, I asked the doctor if I could inject magnesium at home. The answer is no, it’s dangerous, it may be too much and then the uterus will completely relax. But if I go to the hospital, they give me magnesium there. Does anyone experience an overdose? Duration 5 months.
| 06.01.12 17:13 |
| Tell me, how much magnesium can be used to tone up? I was in the hospital, magnesium was given intramuscularly 2 times a day, then intravenously once a day for a total of 10 days. For a week everything was ok. Now at home I have the tone again 10 times a day, I asked the doctor if I could inject magnesium at home. The answer is no, it’s dangerous, it may be too much and then the uterus will completely relax. But if I go to the hospital, they give me magnesium there. Does anyone experience an overdose? Duration 5 months. | |
| 01/06/12 17:58 Reply to message: 72166863 |
| You no longer need magnesium, you need to ask your doctor what to use in your case. In addition to the fact that there is now a huge selection of magnesium preparations and it is absolutely not necessary to mock the fillet, in addition to magnesium, there are means to relieve hypertension. But it doesn’t happen 10 times a day - these are most likely training contractions for you, you don’t need to fight them at all. In general, interact more actively with your doctor and let everything go well! | |
| 01/06/12 18:44 Reply to message: 72167518 |
| Why so categorical? In my opinion, nothing other than magnesia has yet been invented to relieve tone (we are not talking about ginipral, of course). I was in the hospital, I was given magnesium drops 2 times a day. At home, I also did IVs twice in courses of 7 days. 10 cubes per 250 ml, yes, with the blessing of the doctor ALSO for the 6th month. In principle, there cannot be an overdose if you react normally (head does not hurt, blood pressure does not drop critically), you can take 5 cubes 2 times a day. But or 1 time - 10. They did this to me too. Forgive. Magnesium tablets have zero effect, at least for me. And, of course, you need to identify the situation, how much it hurts, whether it can be tolerated. Since yesterday I’ve been having an exacerbation again - I can’t bend or straighten, despite the gynepral. I think that most likely tomorrow I will invite the nurse to drip. | |
BUY GOJI BERRIES IN THE MOSCOW REGION |
I would argue about the benefits of magnesia
do you have anything to compare with? grown children? I don’t see the point in convincing, arguing or persuading someone)) it’s human nature to learn from one’s mistakes)) I’m talking exclusively about my own experience, and not just “reading” the Internet))) with my first child, I categorically resisted all prescriptions and treatments in pregnancy. she was all for “natural” pregnancy and the non-interference of doctors %) she didn’t drink chimes, she refused to go to the hospital, she had gained 25 kg and had swelling. Now he’s a second grader, it’s hard for him and for us. In infancy it was difficult with neurology, but by school everything blossomed like a bright bouquet. and now we are registered with a neurologist. I continued to bear children without showing off and have never regretted it! My clear conviction is that everything that can be done to support the child must be done. If it’s useful for him, then you can be patient and adapt yourself. Moreover, the process of childbirth itself is unpredictable and at least not to reproach yourself later for what you could have done, but did while the child was in the womb. The message was modified by the user on 03/09/2012 at 12:26
All comments to the page “Magnesia during pregnancy” (46)01/07/2015 13:37 Hello! I wanted to share the experience of “not our” medicine. Because Now we live in Dubai. I’m 9 weeks pregnant, yesterday I had an examination, an ultrasound showed the tone of the uterus, they prescribed magnesia with vitamin B6, in tablets! Today, after taking 2 tablets, I feel much better! Is it true! Did not expect! The nagging pain in the lower abdomen is gone! 01/06/2014 1:17 pm I have uterine hypertonicity for 23 weeks, an ultrasound shows a slight opening of the internal os of the uterus, everything is normal on the chair, pressure 100/60 90/60, but I always have low blood pressure during pregnancy, the third pregnancy, two printed. Because On December 30, we agreed to administer a magnesium drip and an intramuscular noshpa at the day hospital. After the drip, I’m a little foggy and the baby moves less, but the hypertonicity is gone, I feel great! I restore my blood pressure with freshly brewed coffee; the doctors said that high-quality coffee is better than pills. Good luck to all!!! 12/19/2013 23:49 my wife had high blood pressure a month ago, she was in bed for 2 weeks, she was prescribed a lot of pills, she ate 1, then 3 and 4 at a time, the pressure did not drop, so they wrote me out on receipt, they didn’t do anything and weren’t prescribed, and so I went to the hospital again antenatal clinic 150120 was put in again and they didn’t prescribe anything - why did we already read that we need to at least drip some magnesium - they’re in no hurry - what kind of specialists are these? 09.22.2013 19:04 After giving birth, do you experience allergies when using magnesium? 08/22/2013 12:09 Now I am in the sixth week of pregnancy, there is a threat of miscarriage. The doctor prescribed magnesium for a blood pressure of 90/60, she says that this is possible. Because of low blood pressure, I constantly sleep and feel “broken.” I didn’t argue, because the doctor knows best , how to save a child... 07/08/2013 09:49 why is fluid not removed from the body when taking magnesium? 01/14/2013 12:32 I myself received both injections and a magnesium drip during my first pregnancy. As far as I remember, the drip did not help with edema at all. 01/02/2013 21:36 Damn, why don’t the symbols go through? one fourth tablet of ginipral!!!!!!!!!! 01/02/2013 21:32 correction: 14 ginipral 01/02/2013 21:29 article is useful, reviews too...... ended up in the hospital with tone in the 21st week... drank magnev6, but didn’t take the tablets the day before... forgot.... came by ambulance, the doctor prescribed magnesium dropper…. As soon as I heard the verdict, I signed a waiver and ran home... I drank 14 gyneprals, slept and everything went away... a week later, swelling began: I excluded flour, sweets, potatoes, salty and poultry from my diet only plain water, no tea, no juices, no fruit drinks... the swelling went away after 2 days... I stuck to the diet for 5 days, everything is fine, my blood pressure is normal... I continue to drink Magnev6, 2 tablets at night and 2 in the morning. 16.11.2012 21:51 Magnesia is not suitable for everyone, each body reacts in its own way. I am now 37 weeks pregnant and my body cannot cope without magnesia, because... very severe swelling (preeclampsia), and because of this, increased blood pressure. They give me intravenous injection. The drug is a little difficult to tolerate, but tolerable. 10/19/2012 11:39 Damn, my blood pressure is 90/60, the highest is 105/60. Yesterday the pain started, I was afraid that there was a threat again (2 times already!!), I was so worried, my blood pressure rose to 120/80 - so all over me I was shaking, nauseous, my legs were cramping!! Ehh, I shouldn’t be an astronaut)) they wanted to give me magnesium, but then they decided to Baralgin. It helped me, but now I read that it is generally dangerous!!! O_o and I can’t take magnesia!! (so what’s better in case of a threat: baralgin or magnesia?? I don’t have any edema, I’m 22 weeks, papaerin is no longer helping... 10/19/2012 11:37 Damn, my blood pressure is 90/60, the highest is 105/60. Yesterday the pain started, I was afraid that there was a threat again (2 times already!!), I was so worried, my blood pressure rose to 120/80 - so I’m all over I was shaking, nauseous, my legs were cramped!! Ehh, I don’t want to be an astronaut)) they wanted to give me magnesium, but then they decided to Baralgin. It helped me, but now I read that it is generally dangerous!!! O_o and I can’t take magnesia!! (so what’s better in case of a threat: baralgin or magnesia?? I don’t have any edema, I’m 22 weeks, papaerin is no longer helping... 09.26.2012 17:38 I don’t give 5 stars because I don’t know if it’s really that safe. Although I haven’t had any problems yet. Many people write that intramuscular injection is very painful. NOT TRUE, GIRLS. If you know how to put it. My husband gives it to me (and he studied with me). first I warm up the magnesium under a hot water tap, then dilute it with novocaine, release the air from the syringe and give it to my husband. then the magic begins under which I even managed to fall asleep several times - my husband sharply inserts the needle and slowly, very slowly injects the solution into the muscle (about 7-10 minutes). Believe me, there is no pain, you don’t even feel how the medicine penetrates the tissue. And there are no bruises. The small bump at the injection site goes away after 6 hours. That’s it. Maybe my advice will help someone. 26.09. 2012 17:38 I don’t give 5 stars because I don’t know if it’s really that safe. although I haven't had any problems yet. many write that intramuscular injection is very painful. NOT TRUE, GIRLS. If you know how to put it. My husband puts it on me (and he learned from me). first I heat the magnesia under a hot water tap, then I dilute it with novocaine, release the air from the syringe and give it to my husband. then the magic begins under which I even managed to fall asleep several times - my husband sharply inserts the needle and slowly, very slowly injects the solution into the muscle (about 7-10 minutes). Believe me, there is no pain, you don’t even feel how the medicine penetrates the tissue, and there are no bruises. a small bump at the injection site goes away after 6 hours. like this. Maybe my advice will help someone. 09/14/2012 17:59 I had a miscarriage after magnesia 09/07/2012 16:39 Girls, after magnesia, a drip that was taken for 5 hours, I slowly had a temperature of 38, my intestines ached all night, I thought I was poisoned.... Now I’m 11 weeks, it was like this for 2 days, then the doctor canceled it, saying that such a reaction is not so rare…. Now I inject intramuscularly, everything is fine. 07/26/2012 12:09 Immediately during the administration of magnesia I began to experience bleeding, what is it? 06/11/2012 08:17 Hello. I am 22 weeks pregnant. They put me on magnesium. After the IV, my fetus is actively moving and kicking vigorously. Is there a threat to my fetus??? 06/06/2012 16:45 And in general, after magnesium at 29 weeks of pregnancy, I started having a terrible allergy... And I had to be treated for it in the hospital for a whole month... Like this... 05/30/2012 01:02 My beloved is given magnesium drops and she has low blood pressure, those bastards (((! And what should I do? high blood pressure 150110 and swelling! doctors are giving her magnesium drips! are there any other methods of treatment!? please help! 05/01/2012 20:54 I was prescribed magnesium drips at the 23rd week of pregnancy, now already the 30th, during this time I've already been given 10-15 droppers (I don't remember exactly) it's 2-3 mg each! To be honest I didn't see any changes, my uterus was often getting toned like that!!! 04/23/2012 09:35 a rare disgusting thing. injected at 30 weeks pregnancy. I thought I was going to die. I felt sick after the first injection, but the doctor said it was necessary, so they gave me a second one. I stood in the corridor all night because... I couldn’t breathe or lie down, my temperature and blood pressure rose. Immediately after the round, the doctor sent me home... And I’m glad, even though I was shaking from side to side, I got out of the hospital alive. my son was born, everything would be fine, but my heart is noisy: I think that magnesia “helped” so much, there were no more troubles 03/27/2012 19:07 A good drug, but after withdrawal the magical effect ends.ALS. 02/17/2012 23:41 I was prescribed magnesia at the 3rd week of pregnancy, if it weren’t for these injections, I would have lost the baby a long time ago, as there was constant tone and bleeding, the injections were very painful, but other than that I didn’t feel any side effects (maybe because sometimes The blood pressure increased very much, but magnesium lowers it) Now it persisted again, at week 17 there was not just a threat, but a miscarriage that began - thank God we were treated and now everything is fine, this time I couldn’t withstand the injections into the muscle, but so on. By the 2nd trimester, they were allowed to administer it along with novocaine, having done a test before that. Everything helped me and there is nothing wrong with it, except for bruises on the butt) 12/25/2011 00:07 Oksana, I have a guess: most likely, it is impossible in the 1st trimester because in the early stages of pregnancy there is a risk of fetal rejection with increased immunity, and magnesia actually improves immunity... 12/19/2011 18:50 of course I have a typo - they weren’t neglected, but they weren’t carried out. There are a lot of drugs that have the same problem, but doctors can prescribe 12/19/2011 18:32 the studies weren’t neglected - you can’t do this on pregnant women, so all such drugs are not officially prescribed in the 1st trimester, but in fact, in practice they are used 12/19/2011 17:28 useful article. I am now in a day hospital, I am 9 weeks old, so I am receiving magnesium drops. But it turns out it’s impossible. I just didn’t understand, I didn’t see in the article why it can’t be taken in the 1st trimester? 12/19/2011 11:19 thank you! very useful article. everything is clear. no questions! :-) 12/17/2011 12:04 Found answers to questions. thank you 11/17/2011 14:38 thank you girls for your feedback, we are glad that our work is useful for you 11/17/2011 13:55 You don’t always find an article as clear as this one 10/26/2011 20:34 thank you very much, in the article I found answers to all the questions that concern me 10/26/2011 07:35 I really liked the article - everything is clearly explained, the material is quite complete. Thanks a lot! 10.10.2011 18:45 I think with a sister as caring as you, everything will be fine with your older sister 10.10.2011 18:20 Thank you very much! Very informative article. The fact is that I am only 16 years old, and my sister is pregnant. Therefore, I am worried about the health of my sister and future nephew! =) 08/25/2011 20:48 It’s a shame that I didn’t know all this while bearing a child. The memories are not pleasant: I fainted after a magnesium injection (my blood pressure dropped 30 to 60), they pumped me out and the injections continued while I was lying in bed. Dizziness and weakness up to vomiting after the injection and pain in the lower abdomen. They told me to eat chocolate and drink coffee. Requests to cancel did not yield anything, and I am an experienced allergy sufferer. 07/31/2011 11:51 Thank you for the complete, interesting answers!!!!! 10.06.2011 13:33 |
Characteristics of parameters
The 35th week of pregnancy is characterized by the baby's readiness for birth. Its height can range from 45 to 50 cm.
The fetal head is almost completely formed and is about 9 cm in circumference. The diameter of the chest can be from 8 to 8.5 cm. The circumference of the tummy is just over 9 cm.
At 35 weeks of pregnancy, the weight of the fetus can be from 2 to 3 kg. The main function of the child’s body during this period is to actively gain fat for further development.
In the middle of the third trimester, the baby's development is almost complete. Therefore, childbirth at 35 weeks of pregnancy is not dangerous and usually occurs without risks to the life of the mother and child.
General information about pregnancy
To calculate the duration of pregnancy, a specific indicator is used: the absence of menstruation on time. The beginning of gestation is usually counted from the first day of the last menstruation.
The difficulty of the calculation lies in the fact that there is no data on the exact time of ovulation and fertilization. Ovulation can be:
- early;
- late;
- average.
Presumably, pregnancy occurs in the middle of the menstrual cycle or within 24 to 48 hours after ovulation.
As a result, obstetric and calendar months have differences.
The average period from conception to delivery is 266 days or 38 weeks.
In this case, deviations of 14 days upward are accepted, which is associated with the possibility of changing the date of conception. As a result, a full-term pregnancy can last 266 - 280 days or 38 - 40 obstetric weeks.
If data on the date of the last menstruation is not available, the gestational age is determined based on a comprehensive study.
- From the moment of the first movement of the fetus. The average period for primiparous women is 20 weeks, multiparous women - 18 weeks. The indicator is inaccurate.
- Uterine size and UMR. Until 12 weeks of pregnancy, the fundus of the uterus is located below the pubic bone; the gestational age is determined by vaginal examination. After the 12th week, the fundus of the uterus extends beyond the pubis and the period is determined by measuring the UMR.
- Ultrasound of the fetus. It is considered the most reliable. It is based on measuring the size of the fetus and its correlation with normal indicators for the duration of pregnancy.
Number of obstetric and calendar months
Normally, pregnancy lasts 10 obstetric months or 9 calendar months.
The difference arises when calculating:
- 1 obstetric month = 28 days;
- 10 obstetric months = 40 weeks.
When calculating calendar months, the period depends on the number of days in the month, which can range from 28 to 31.
Different names contain the same number of days. The expected due date is the same.
Thus, a fetus at the 8th week of embryogenesis corresponds to 10 weeks of pregnancy, at 31 - 33 weeks, at 38 - 40 weeks.
Woman's condition
At this time, the baby may completely roll over in his stomach. He begins his preparations for birth. Some babies begin to descend in the womb. If the baby has already changed its position, the expectant mother’s breathing becomes much easier. However, some babies are in no hurry to change their location until the very beginning of labor.
The size of the expectant mother's belly reaches its peak. Sometimes it seems that the belly at 35 weeks of pregnancy is simply huge. Indeed, over the entire period, the woman’s uterus increased more than 1000 times. In 8 months, the woman’s body has completely changed. Now all organs are working in enhanced mode to ensure normal delivery.
Despite the child’s sufficient weight, the 35th week of pregnancy is not the final stage for the birth process. The baby should gain strength in the mother’s womb for another 1 month. However, if premature birth occurs during this period, it will not pose a threat to his life.
It becomes more and more difficult for the expectant mother to move every day. Every movement is difficult. By this time, a woman can gain from 10 to 15 kg of weight.
Why does the baby begin to move less in the stomach?
The baby doesn’t move much in the stomach - what are the dangers? Every expectant mother listens very carefully to the movements of her baby and always worries if their frequency and intensity go beyond the norm. What can cause a child to become less active in the womb?
First you need to learn how to determine whether the number of movements is normal. Pregnant women usually begin to feel tremors at 18-20 weeks.
Fetal movements during pregnancy are not always regular, that is, they are not felt at any certain time period every day. Much depends on the daily routine of the mother herself.
Plentiful nutrition increases the child’s activity, and quiet everyday life can lull him to sleep and reduce the number of movements.
And yet, how often should a child move in the womb? Typically, obstetricians and gynecologists recommend counting a series of kicks from 9 a.m. It is necessary to count not only distinct movements, but also episodes of barely noticeable tremors.
If there are not even ten such series or episodes before 21 o'clock, then you should pay attention to this. Why a child moves little is a well-known fact.
Low physical activity may be due to a lack of oxygen in the child’s blood.
Inactivity for several hours requires immediate medical attention. Delay can lead to severe metabolic disorders and death of the tissues of the child’s heart and brain, which are most sensitive to lack of oxygen. The doctor must make sure that the baby's heart is working normally.
Listening with a stethoscope in such circumstances will be clearly insufficient. Auscultation cannot provide enough information about the activity of the child’s heart, so it is necessary to use more accurate examination methods. Cardiotocography (CTG) is usually used, which records the child’s heart rate for half an hour.
The permissible heart rate is from 120 to 170 beats per minute. If the rhythm is maintained at a lower level or there is no response to movements, then we can talk about pathological hypoxia. If such problems occur, a caesarean section is usually prescribed. If deviations from the norm are insignificant, then there is a chance to correct everything with therapeutic methods.
Interesting: Back pain 27 weeks pregnant
Today, cardiotocography is performed on women regularly starting from the 34th week of pregnancy.
If there are no insurmountable obstacles, and even more so if the child begins to move less, then you should not refuse this medical service.
Condition of the uterus
The 35th week of pregnancy is characterized by the highest state of the uterine muscle. It reaches a significant size and puts pressure on the woman’s bladder and stomach. There is a frequent urge to urinate. Therefore, walks that take a long time are not recommended for the expectant mother. Also, don't go on a trip.
The uterus also puts pressure on the diaphragm. The woman's breathing becomes difficult. This causes some discomfort during a night's rest. To alleviate her condition, a woman is recommended to lie on her side.
At this time, the uterus begins to intensively prepare for childbirth. She acquires special sensitivity. Her tone reaches its peak. Now every movement of a woman responds with painful sensations in her.
Also at 35 weeks, the cervix begins to actively develop. The birth canal is formed.
Belly at 33 weeks pregnant
An enlarged belly causes anxiety to the mother and can cause discomfort in the area of the costal arch and pelvis. The uterus at 33 weeks of pregnancy is 33 centimeters above the womb and 13 centimeters above the navel. During this period, the mother’s normal weight increased by 12.5 kilograms. The uterus pressing on the bladder causes frequent urination. There is no way to cope with these phenomena, you just need to be patient a little longer, because there is very little left before the birth.
The fundus of the uterus is very high, and this is in most cases accompanied by heartburn and shortness of breath. You can alleviate your condition somewhat by adjusting your diet. Try to eat often, in small portions. Be sure to include fiber-rich foods in your diet to improve digestion. This will help cope with constipation, which often accompanies pregnancy. It's nice to know that heartburn and shortness of breath will very soon decrease - the uterus will drop slightly lower before childbirth.
The appearance of contractions
If a woman has a stomach ache at 35 weeks of pregnancy, this indicates that the body is beginning to prepare for childbirth. The first training contractions appear. Usually the pain from them is quite minor.
Contractions can occur at any time. They have not yet become permanent. During a normal pregnancy, pain should subside in a short period of time.
If the contractions are prolonged and the pain from them is significant, the expectant mother is advised to seek advice from a specialist.
How often should a baby move?
A woman often begins to perceive herself as truly pregnant only when she feels the first movements of her unborn baby.
Fetal movements begin much earlier than is commonly thought. At the end of the eighth week of intrauterine development, the first unconscious and uncoordinated movements of the embryo begin.
The muscles around the mouth and cheeks begin to move first, which is probably why the sucking reflex is the main one in a newborn baby.
Gradually, the movements cover all muscle groups and movements become more conscious.
By about the twentieth week of its intrauterine development, it is no longer the embryo, but the fetus, which begins to move so actively that its movements are already noticed by the expectant mother. It happens that it’s already twenty weeks and the fetus is still not moving. There are several explanations for this:
- perhaps this is an individual characteristic of the fetus, and therefore it is considered normal if movements begin at 22–23 weeks;
- if the placenta of the expectant mother is located on the anterior wall, this may be the reason that still weak movements are simply not felt until they become more active;
- It happens that the mother herself has reduced sensitivity due to the peculiar structure of the nerve endings.
If you felt movements much earlier - at 15-17 weeks, this is also a variant of the norm. It is generally accepted that in multiparous women, movements begin a little earlier with each subsequent pregnancy. This is not entirely true. Since even among mothers with many children, it happens that the first-born began to move earlier than, for example, the last child.
But now the time for the first movements has come, and you don’t know how to understand that it is the fetus that is moving, and not confuse it with the motor activity of the intestines. For some, the movements of the child are similar to bursting bubbles, for others it seems that a fish is swimming inside and touching the walls of the uterus, this happens differently for everyone.
It is believed that if the mother feels the first movements on the right, then there will be a boy, and if on the left, there will be a girl.
How much and how often should the fetus move?
At first, movements may be irregular: every other day, or even two. But over time, the child improves his motor activity more and more, and the baby will move more and more often.
For a period of 28 weeks or more, according to the standards, there should be at least ten movements per day. A child's activity becomes the main indicator of his health. If the fetus moves actively and regularly, this is a good sign.
And if movements for no apparent reason suddenly become violent, this is a reason to consult a doctor, get tested, do fetal cardiotocography, or an unscheduled ultrasound.
Very active movements may indicate a lack of oxygen.
If the diagnosis is confirmed, the expectant mother will be prescribed a course of supportive therapy and more walks in the fresh air.
After the middle of pregnancy, violent movements can be caused by the fact that the pregnant woman, as before, rests lying on her back. In this position, the inferior vena cava is compressed, blood suddenly stops flowing to the fetus, and it begins to protest.
How long can a fetus not move?
There are situations when, on the contrary, the fetus begins to move less or stops altogether. Think about it, perhaps you spent the whole day on your feet, and therefore, with constant movement, you simply did not hear any movements.
There are several ways to make the fetus move. Lie on your side and listen. Within 15 minutes the fruit will make itself known. You can drink sweet tea or eat something sweet. The blood glucose level will rise and the baby will react immediately.
It is considered normal if the fetus does not move for 3-4 hours. But if all your tricks lead to nothing, and within 12 hours you do not hear any movements, this is a reason to immediately seek medical help.
Night rest period
Often expectant mothers complain that at 35 weeks of pregnancy they experience sleep disturbances. Insomnia takes away the last of the strength from expectant mothers.
It is difficult for a pregnant woman to find a comfortable sleeping position. Large belly size does not allow you to relax. Special pillows for pregnant women help partially solve the problem.
Frequent urge to urinate also contributes to insomnia. To alleviate a woman’s condition, it is not recommended to drink liquid before bed.
You can also take a valerian tablet. It will help the expectant mother relax and get some rest.
It is useful to perform simple physical exercises before going to bed. They consist of circular movements of the hips. This will slightly reduce the tone of the uterus and relax its muscles.
Side effects
Most patients who are prescribed droppers with Magnesia for uterine tone tolerate the treatment well. Already after the first administration, a noticeable improvement in well-being is noted. The activity of the reproductive organ decreases, as a result of which the pain disappears. When using Magnesia, blood circulation in the placenta is normalized and the supply of oxygen to the fetus is increased. This may be accompanied by an increase in the motor activity of the unborn child.
Adverse reactions to treatment are extremely rare. Many years of experience in using this drug allows us to create a list of the most common complaints:
- dysfunction of the digestive tract;
- feeling weak and dizzy;
- headache;
- increased anxiety and restlessness;
- flushed face;
- feeling of heat;
- decrease in body temperature;
- changes in blood pressure;
- increased thirst.
Usually these signs do not become a reason to discontinue the medication. If a woman’s condition continues to worsen, doctors change the treatment regimen and prescribe other methods of combating uterine tone. To reduce the activity of the reproductive organ, along with Magnesia injections, the following are also used: antispasmodics, tocolytics, painkillers, hormones, vitamin complexes and homeopathy.
The appearance of heartburn
Heartburn is a common companion of all pregnant women. This is explained by the fact that the fruit, which has increased in size, puts active pressure on the digestive system. This is why many pregnant women experience heartburn.
You may also feel a feeling of heaviness in your stomach. This is due to the active development of the baby.
To alleviate the condition, a woman is recommended to eat light foods; meals should be fractional. The diet of the expectant mother is rich in useful minerals and vitamins.
Use of the drug in the first trimester
Hypertonicity of the uterus in the first three months of pregnancy causes pain and a feeling of heaviness in the lower abdomen. This disorder can also be suspected by the appearance of bloody discharge. A tense uterus can be felt by lying on your back and feeling your stomach with your hand.
information Tension of the uterine muscles can lead to spontaneous abortion and therefore requires urgent treatment. A dropper with magnesium has a tocolytic effect. This means that when using the medicine, the tone of the uterus is normalized, and the threat of early miscarriage recedes.
The appearance of discharge. Is it dangerous?
The 35th week of pregnancy is coming to an end. The stomach pulls, contractions appear, the child sinks lower and lower. The woman is almost ready to give birth. However, during this period mucous discharge may occur. Are they dangerous for the expectant mother?
To understand this, it is necessary to characterize the secretions. If they look mucus, milky or clear, there is no cause for concern. This is how the woman’s body begins its preparation for the birth process.
It is worth paying attention if there is blood in the mucus. Most likely, the baby's placenta has separated. To avoid the risk of miscarriage, you need to seek help as soon as possible.
Also at this time the traffic jam may come out. It can be mistaken for mucous discharge. The removal of the plug is a sure sign of the onset of labor. It is also necessary to take care of hospitalization.
Indications for caesarean section
Among the indications for caesarean section at the 33rd week of pregnancy are:
- severe intrauterine condition of the fetus;
- Rhesus conflict;
- placental abruption;
- acute fetal hypoxia;
- concomitant diseases of the mother in the stage of decompensation;
- transverse or breech presentation of the fetus;
- anatomically narrow pelvis;
- malignant neoplasms in women.
Indications for a cesarean section are determined individually for each patient. At the same time, the condition of the woman and child is at the core.
Sex
Sex at 33 weeks of pregnancy is possible in the absence of pathological changes in the woman and child.
Reasons for refusing sex include:
- reluctance of sexual partners;
- active fetal movements;
- discharge of mucus plug or amniotic fluid.
It is not recommended for sperm to enter the vagina, which can lead to softening of the cervix and the threat of miscarriage. During sexual intercourse, you should use a condom or avoid ejaculating in the vagina.
During sexual intercourse, sudden movements and deep penetrations should be avoided. Preferred positions include penetration from behind with the woman lying on her side.
Nutrition
The nutrition of a pregnant woman at the thirty-third week should be balanced and correct.
Restrictions apply to salt, smoked, spicy and sour foods.
The drinking regime includes drinking up to 2 liters of liquid per day.
The 34th week of pregnancy has arrived and the baby’s movements are becoming very strong and noticeable.
How quickly time flies - just a little more and your baby will be born.
Woman's experiences
During this period, a woman feels her connection with her child more than ever. He is ready to be born. This time can be called a rest period. Concern about the baby's viability passes.
A child at 35 weeks of pregnancy actively shows that he hears his parents. He may push when you touch his stomach or, conversely, calm down.
To achieve favorable contact at this time, the expectant mother is recommended to talk with the child more often, read fairy tales to him, and sing children's songs.
If the pregnant woman’s condition allows, you can take short walks, breathe fresh air, and watch animals and birds.
The closer the due date approaches, the more anxious the mother feels. This is also facilitated by stories from friends and relatives. Try to protect yourself from unnecessary information at this time.
Important points
The dosage of the drug during pregnancy varies and depends on the woman’s health condition. A 25% solution is calculated so that about 0.5-1 grams of the active substance enters the patient’s body. In severe conditions, the dose increases greatly. For example, for a seizure caused by eclampsia, magnesia is administered at a rate of 5 grams per hour.
information When administering a drip, the patient lies on a couch or bed. The dropper is fixed next to the bed on a special tripod. A magnesium solution is injected through a needle inserted into a vein. The procedure usually lasts no more than 2 hours. You need to get up after a drip gradually, carefully, because the decrease in pressure causes dizziness and fainting.
A course of treatment with magnesium for pregnant women lasts no longer than 5 days. Sometimes only one dropper is needed (for example, to reduce blood pressure). Every woman has the right to refuse the procedure, but such a decision must be seriously considered. Remember that the drug is used to maintain pregnancy and the health of the mother and fetus.
What should an expectant mother do?
What should a pregnant woman do at this stage? The middle of the third trimester is the best time to rest. A woman should gain strength before the upcoming birth.
By this time, the expectant mother should already know exactly how and in what institution the baby will be born.
It is worth consulting with your doctor. If a planned cesarean section is scheduled for delivery, the expectant mother needs to prepare for going to the maternity hospital and prepare all the necessary things.
It is worth noting that premature birth may occur this week. Therefore, the expectant mother should have things ready for visiting the maternity hospital.
At this time, you should avoid long walks and travel. Doctors do not recommend flying on an airplane or traveling long distances by car.
Why is magnesium used during pregnancy?
Doctors associate terrible conditions with magnesium deficiency: miscarriage, early and late gestosis, deficiency of fetal weight. Magnesium is used by gynecologists to help in the following situations:
- high tone of the uterine muscles;
- threatened miscarriage;
- premature labor;
- severe edema syndrome;
- preeclampsia, eclampsia;
- convulsive syndrome;
- arterial hypertension;
- impaired blood supply to the placenta.
It is important to know that when using magnesia there is a risk to the child’s health. A newborn may have breathing problems and a low heart rate. Therefore, treatment is canceled one day before the probable date of birth. Doctors use this drug only when they are confident that the benefits will outweigh the likely side effects.
Physical exercise
To prepare her body for childbirth, the expectant mother should not forget about playing sports.
The loads should not be strong. Keep track of their number. At the first occurrence of pain, exercise should be stopped.
Yoga and swimming are suitable exercises. Don't forget about breathing training. Such gymnastics will help in the upcoming birth.
It is useful for a woman’s condition to perform exercises on a gymnastic ball.
Practicing proper breathing will help significantly shorten the labor process and reduce pain during labor.
Contraindications to treatment with magnesium
A pregnant woman should never be prescribed magnesium sulfate in the following situations:
- low blood pressure (hypotension);
- Heart rate less than 60 per minute (bradycardia);
- heart rhythm and conduction disturbances;
- serious kidney disease;
- the appearance of contractions.
When using magnesia, unpleasant sensations may occur: headache, nausea, general weakness, sweating. You should notify your doctor about the occurrence of side effects. He may reduce the dose of the medicine or replace it with another similar drug.
The intimate side of life
Towards the end of pregnancy, all the thoughts of the expectant mother are occupied with the upcoming meeting with the baby. However, you should not forget about your spouse and his needs during this period.
During this time, the woman is allowed to have sex. Only in some cases there are contraindications. The attending physician will definitely warn you about them.
During this period, you do not need to use contraception. Sperm entering the female body has a beneficial effect on the condition of the walls of the uterus and helps prepare it for childbirth.
The large size of the expectant mother’s belly can cause some discomfort during this period. Therefore, it is worth paying attention to poses from the state on the side or behind.
In what cases should you refuse intimate relationships:
- When pain occurs.
- If there is a threat of miscarriage.
- With the discharge of amniotic fluid and plugs.
- During multiple pregnancy.
- With abnormal locations of the placenta.
Changes in the female body
The 33rd week of pregnancy is accompanied by characteristic changes in the female body. The child gains significant weight, which leads to an increase in the size of the abdomen and its circumference.
As a result of active movements of the child, a woman may experience unpleasant symptoms.
- Heartburn. Occurs more often in the evening. The basis is an increase in the acidity of gastric juice or an exacerbation of chronic diseases of the gastrointestinal tract.
- Cramps. Occur periodically. May indicate a lack of calcium or magnesium in the body.
- Heaviness or pain in the lumbar region. They occur when lying on your back due to compression of the femoral nerve.
- Itchy skin and stretch marks in the abdominal area. They occur as a result of rapid stretching of the skin. Symptoms are reduced when wearing a bandage.
- Dyspnea. As a result of the increase in the size of the uterus, pressure occurs on the diaphragm.
- Frequent urination. Appears when the uterus presses on the bladder.
Among the pathological manifestations in the thirty-third week of gestation, the following symptoms may appear.
- Carpal tunnel syndrome. Occurs in the presence of obvious or hidden edema due to impaired blood flow. Manifests itself as numbness or pain in the wrist area.
- Late gestosis. It manifests itself as a triad of symptoms: edema, increased blood pressure and the appearance of protein in the urine. Can lead to serious condition of the woman and fetus. Requires immediate hospital treatment.
Weight gain
Normal weight gain over the entire period of pregnancy is 10 - 12 kg. An increase of 300 to 400 g is allowed per week. If these indicators are exceeded, it is necessary to differentiate with the development of edema.
A woman with excessive weight gain in a week is recommended to do 1 fasting day, and then visit a gynecologist for a control weigh-in.
If there is an effect from the fasting day in the form of a decrease in body weight or no increase, therapy continues on an outpatient basis.
If there is no effect from unloading or edema is detected, the woman is sent to the hospital, which is necessary to prevent the development of late gestosis.
Abdominal circumference and prolapse
Normally, the height of the uterine fundus ranges from 31 to 33 cm, and the uterine fundus is located at the level of the midline between the navel and sternum.
Uterine prolapse can occur with:
- incorrect position of the fetus, located transversely;
- threatening premature birth, accompanied by drooping of the fetal head;
- IUGR or intrauterine growth restriction;
- oligohydramnios.
By the 33rd week of gestation, the abdominal circumference is on average 85 - 90 cm. This figure is considered normal for a woman weighing up to 70 kg. Abdominal circumference can vary individually.
Discharge
Normally, discharge from the genital tract should be clear, white or yellowish in color and not accompanied by itching or burning.
Among the pathological discharges the following are noted.
- Yellow with an unpleasant odor. They may appear with bacterial vaginosis or other inflammatory processes.
- Curd-like with a sour odor. Appears with vaginal candidiasis.
- Bloody. They can occur with premature detachment of a normally located placenta, as well as in the presence of cervical erosion. The condition requires immediate hospitalization.
- Mucous discharge. They may appear when the mucous plug comes out. Hospitalization required.
- Liquid discharge without odor. May appear when amniotic fluid leaks or breaks. Hospitalization required.
Monitoring the condition of the fetus
The 35th week of pregnancy has arrived. How many months are left until the long-awaited meeting? If you count according to the usual calendar, then less than a month. According to obstetrics - 5 weeks. At this time, it is very important to monitor the baby’s developmental status.
Therefore, many experts prescribe the final study at 35 weeks. Usually this is an ultrasound. It is necessary to control the weight and height of the child. The attending physician diagnoses its level of development, excludes or confirms possible complications.
Ultrasound is also recommended to monitor the state of fetal presentation and the entanglement of the umbilical cord. Depending on the condition of the child and the level of amniotic fluid, the doctor chooses the method of delivery.
Also, at 35 weeks of pregnancy, the health status of the expectant mother, her blood pressure level, and heart rate are monitored. Blood and urine tests are also prescribed.
Complications
At the 33rd week of gestation, pregnancy complications may develop, which can lead to premature birth or other abnormalities.
Oligohydramnios and polyhydramnios
Oligohydramnios refers to an insufficient amount of amniotic fluid. May occur with an infectious disease of the mother.
Treatment is carried out in a hospital with drugs that improve uteroplacental blood flow and placental function. If an infectious agent is identified, antibiotic therapy is added.
Polyhydramnios is considered to be excess of the permissible amount of amniotic fluid. Treatment is carried out in a hospital.
If there is pathology in the amniotic fluid, a control ultrasound is necessary after treatment at 36-37 weeks of pregnancy.
Tone
At the 33rd week of pregnancy, the uterus may become toned during training contractions or the threat of premature birth.
Uterine tone is a “petrification” of the muscles of the uterus, which is manifested by the appearance of a firm abdomen with clear outlines.
If the tone does not go away on its own, the intensity increases, or pain appears in the lower abdomen, you should seek medical help.
Breech presentation
Breech presentation at 33 weeks of gestation can be detected normally. The child still has the opportunity to turn his head down.
If the breech presentation of the fetus remains, it is necessary to decide on the possibility of natural childbirth or delivery by cesarean section.
Premature maturation of the placenta
With premature maturation of the placenta, fetal suffering in the form of hypoxia is observed, which can lead to IUGR or other complications.
If there is pathology in the placenta, calcifications are detected, which cease to perform the functions of a child's place.