Due to various diseases, damage to the nerve endings on the face can develop. The facial nerve is quite vulnerable due to its location on the face, so its inflammation develops quite easily and quickly. One of the common diseases is neuropathy of the facial nerve. It is worth knowing what causes this disease, what the main symptoms are, and what is the treatment for the pathology.
Related articles:
Facial nerve paresis - symptoms and treatment Effective tips for treating facial nerve (neuritis) at home Pinched nerve in the cervical spine: how to treat? Facial nerve paresis - symptoms and treatment We quickly treat the sciatic nerve at home
Neuropathy - what is this disease?
Neuropathy is a disorder in the functioning of the facial nerve that results in paralysis and weakness of the facial muscles. This condition usually occurs on one side of the face, but in rare cases it spreads to both sides. The facial nerve is in a position in which it is easy to compress it or transmit an infection to it, so various injuries and inflammatory processes in it are common.
To find the designation for neuropathy in ICD-10, you should look at the numbers from G50. Depending on the characteristics of the lesion of the facial nerve and the reason for the designation in the registry may be different.
Neuropathy may be primary or secondary. The primary form occurs due to direct infection of the nerve, hypothermia, the secondary form develops against the background of other diseases in which transmission of infection can occur.
Regardless of the cause of the disease, treatment must be started immediately. The more advanced the inflammatory process and dysfunction of the nerve, the more difficult it will be to relieve paralysis of the facial muscles and restore normal mobility and sensitivity.
Development mechanism
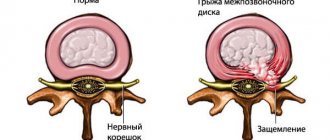
The mechanism of facial nerve development is based on dysfunction in the nerves. Tumors, trauma, and infections gradually destroy myelin and lemmocytes involved in transmitting impulses along the fibers; in complex cases, the axial cylinder is destroyed. As a result, the transmission of impulses from the brain to tissues is disrupted in nerve fibers, which then cease to function.
The most common form of facial paralysis, which occurs as a result of acute neuritis or neuropathy, is idiopathic - Bell's syndrome (or Bell's palsy). The pathology develops sharply. First, uncharacteristic pain behind the ear appears, and after 2-3 days the facial muscles weaken.
Bell's palsy occurs in several stages:
- gradual increase in symptoms (from 48 hours to 8 days), the appearance of edema, ischemia, pinched nerve;
- early recovery – up to 1 month – return to the previous functionality of the facial muscles and elimination of swelling of the fibers;
- late recovery (from 3 to 4 months) – disturbances in the facial muscles are restored slowly and not completely, which indicates severe changes in the facial nerve;
- the final stage, which is characterized by residual signs of paralysis - atrophy of facial muscles, involuntary movements of facial fragments (tip of the mouth, eye).
Causes
The main reason that provokes the development of the disease is hypothermia. You can earn it by being without a hat in the cold for a long time, sitting under a powerful air conditioner running, sitting by an open window in a draft, in a strong cold wind. In this case, the nerve disease will be accompanied by cold symptoms.
Primary neuropathy can also develop as a result of trauma, blows and bruises of various types. The facial nerve is located in a fairly narrow canal, so when an impact occurs, a slight displacement of the bones may occur, resulting in compression of the nerve branches.
Other factors leading to the development of neuropathy include:
- Various systemic infections and diseases. One of the most common causes of damage to the facial nerve is the herpes virus, which causes shingles. In addition to herpes, the disease can be caused by systemic lupus erythematosus, an infection that causes mumps, and others.
- Inflammatory diseases of the nasopharynx and ear. Most often, otitis media can provoke inflammatory damage to the nerve branches on the face; in the advanced form of the disease, the infection spreads deep into the ear, where it can affect the nerve and other tissues.
- Various tumors, consequences of heart disease. In these cases, such pathologies can cause compression of the nerve ending or its damage in another way.
Also, sometimes experts note a hereditary factor. If someone in the family has already had neuropathy, more attention should be paid to preventing the disease. Features of the structure of the skull bones can be inherited, as a result of which the nerve canal may be too narrowed.
Important! If secondary neuropathy develops, it is extremely important to treat the very cause of this disease.
Diagnosis of neuritis
Diagnosis of neuritis of the facial nerve
Diagnosis of neuritis of the facial nerve is carried out on the basis of:
- Complaints and medical history, objective examination of the face and assessment of its symmetry at rest and during articulation and an attempt to smile.
- Special diagnostic tests for neuritis of the facial nerve: closing the eyes simultaneously and alternately, squinting the eyes, moving the eyebrows (symmetrically and asymmetrically), an attempt to frown the nose and eyebrows, and purse the lips into a tube.
- Checking the taste and temperature sensitivity of the tongue (dysgeusia) - a violation of the differentiation of salty and sweet, only the sensation of bitter remains unchanged.
- Identification of pathological symptoms of neuritis of the facial nerve:
- An unpleasant and immediately noticeable sign is Bell's symptom - an upward rotation of the eyeball when trying to close the eyes. As a result, the following symptom becomes noticeable - lagophthalmos or “hare's eye”, this is a gaping of the white area of the sclera of the eye.
- Revillot's sign is eyelid dyskinesia that occurs when trying to close the eyes. On the healthy side, the eye remains slightly open due to lack of control over the orbicularis oculi muscle.
- Symptom of sailing - when you try to take air into your mouth and close your lips tightly, blow out a candle or whistle, the air whistles out of the paralyzed corner of the mouth, and the cheek “sails” at the same time.
- “Racket” symptom – when you try to bare your teeth, their exposure occurs only on the healthy side, as a result of which the mouth gap takes the form of a lying tennis racket.
- Convergent strabismus in strokes.
- Horizontal nystagmus in Hunt's syndrome.
Facial nerve neuropathy in children
If this lesion and paralysis of the facial muscles occurs in a child, attention should be paid to this. In children, the development of this disease can be provoked by improper development and structure of the bones of the skull, so if there is no other obvious cause, you need to make sure that there is no pathology.
Also, nerve damage occurs in a number of autoimmune diseases, some of them are inherited, some develop for other reasons. Some of these diseases first manifest themselves in childhood; during diagnosis, it is extremely important to exclude their occurrence.
Why is neuropathy dangerous?
With this disease, it is important to begin treatment as quickly as possible, because over time, after the lesion, facial contracture begins to develop, the face literally becomes paralyzed, it freezes with a certain expression. Correcting such a consequence of the disease can be quite difficult.
Also, over time, facial sensitivity may begin to be completely lost. The more time passes, the more difficult it will be to restore full motor functions, sensitivity of the skin of the face and tongue.
Do not forget that with improper treatment or insufficient treatment of diseases that provoked nerve damage in secondary neuropathy, the disease can recur.
Important! In most cases, the symptoms of the disease are so obvious that additional diagnostics are not required.
Clinical picture
All manifestations of pathology are usually concentrated along the nerve trunk, which is exposed to pathological effects. We are talking about the following areas:
- Cheeks.
- Brows.
- Forehead.
- Jaw.
As a rule, the points where the nerve approaches the epidermis are the most painful. In this case, we mean the chin and eye socket. Facial neuralgia has a characteristic feature. It usually affects only one side.
Although in some cases there is also a bilateral form. Patients experience different sensations. However, in most cases there are general manifestations that indicate that the patient has facial neuralgia.
Symptoms are most often the following: unbearable, burning pain that can last from a few seconds to several minutes. As a rule, unpleasant sensations appear in the nasolabial triangle.
They then spread over wider areas. In the case of spontaneous neuralgia, a person may suddenly freeze. Sometimes he starts rubbing his face intensely. Sudden pain can radiate to the scalp, teeth, ears and even fingers.
Peak pain is very common. This occurs because the muscles near the affected nerve go into spasm. The clinical picture of the disease is complemented by other symptoms, among which are the following:
- Uncontrollable tearing.
- Burning sensation after intense pain stops.
- Uncontrollable drooling.
- Redness of the facial skin (in the form of spots or general).
- No pain at night.
- Reducing discomfort after strong pressure on the skin.
1 smooth forehead 2 impossible to close the eyelid 3. drooping corner of the mouth 4. facial nerves
Facial neuritis develops slowly.
- At first, only pain behind the ear may appear.
- After a few days, facial asymmetry appears. In this case, there is a smoothing of the nasolabial fold on the affected side, and drooping of the corner of the mouth.
- Also, the patient cannot close the eyelids on the same side, and when trying to do this, Bell’s symptom appears - the eyeball turns upward.
- The patient cannot bare his teeth, smile, raise his eyebrows, close his eyes, or make his lips appear like a tube.
- On the affected side, the eyelids are wide open, the eyeball seems to be pushed forward (lagophthalmos). The symptom of a “hare’s eye” is always present - a white strip of sclera is visible between the iris and the lower eyelid.
We invite you to read: Surgery to remove a coccyx cyst: types, what the neoplasm looks like, how it is done and how long the intervention lasts
Since the facial nerve has several bundles that provide sensory innervation, the following symptoms may occur:
- loss of taste sensitivity in the anterior third of the tongue
- salivation
- dry eye or, conversely, lacrimation
- Some patients exhibit an interesting feature. Dry eyes cause tearing when eating
- A number of patients experience hyperacusis - ordinary sounds seem loud and too harsh to them
Treatment
Treatment of this disease is usually complex; first, it is important to relieve swelling, pain and inflammation, after which mobility begins to return, sensitivity and normal blood circulation are restored. Treatment is usually carried out at home; visiting a clinic or hospital is required only for physiotherapeutic procedures.
Then, after the main treatment, the rehabilitation stage begins, at which it is important to consolidate the results of therapy and finally restore the sensitivity of the nerve endings. The following methods are usually used for treatment:
- Drugs. First of all, anti-inflammatory drugs are used; treatment with prednisolone is usually prescribed. In addition to this drug, diuretics are used to relieve edema, nicotinic acid and its analogues to dilate blood vessels. Vitamin B therapy may also be used.
- Physiotherapy. Procedures are prescribed from the sixth day of treatment if drug therapy has given a good result. Usually UHF, phonoresis, and contact heat are used.
- Treatment with acupuncture and other non-traditional methods. They are not used so often; official medicine does not consider these treatment methods effective. Acupuncture and other alternative treatment methods should be carried out exclusively by a specialist in this field; improper treatment can cause serious harm.
- Treatment with folk remedies. Traditional methods are not so effective for neuropathy of the facial nerve; in addition, in the initial stages of therapy, the affected area cannot be heated. However, towards the end of the course of treatment, herbal compresses can be used. For example, you need to brew sage herb, then squeeze it out, put it on gauze and apply it to the side of your face for 10 - 15 minutes.
By combining techniques, you can achieve better results. However, it is advised to consult a doctor about the admissibility and effectiveness of the chosen methods of therapy.
Ointments
As part of drug therapy, not only tablets and injections are used, but also local remedies - creams and ointments:
- warming drugs (capsicam, menovazin) - warm the skin over the affected nerve, increasing blood flow. This principle of action allows you to reduce pain;
- combined ointments (NSAIDs added to the composition) - have an anti-inflammatory, analgesic and warming effect (finalgon);
- painkillers - have an analgesic effect (Anesthetic ointment, lidocaine ointment).
Treatment of facial neuritis requires an integrated approach: a combination of drug therapy and physiotherapy.
However, the first stage of recovery is always associated with taking medications. Doctors are not limited to one group of drugs and prescribe combined treatment: painkillers, hormonal, neurostimulating, diuretics.
Rehabilitation
To restore all motor functions, facial massage is used. You can do it at home yourself, preferably doing it in front of a mirror. The affected side of the face is gently massaged with stroking movements with slight pressure, trying to warm up the affected muscles.
Another mandatory rehabilitation method is physical therapy for the face. The exercises need to be repeated every day for 10 - 15 minutes, it is better to do this in front of a mirror. Exercises include whistling, pursing lips, wide smiles, winking, and pronouncing individual words, letters and sounds. Therapeutic exercises ensure that the disease does not return.