According to statistics, toenail diseases are very widespread: every fourth person suffers from one or another disease. The bulk of these problems are classified as acquired and only 10 percent are congenital. But this is not only an aesthetic problem. Many people experience serious psychological discomfort due to the unsightly appearance of their own feet. Also, some nail diseases are accompanied by severe pain and can lead to serious complications. Therefore, treatment should not be delayed under any circumstances: treatment of the disease should begin when its first signs appear. Specialists in the field will help you cure the disease: a dermatologist and a mycologist.
Causes and signs of toenail problems
What factors provoke toenail diseases? The greatest influence on the development of the disease is exerted by:
- infections (fungal and non-fungal);
- skin diseases;
- improper care;
- mechanical impacts (injuries);
- genetic predisposition;
- aging;
- diseases of the cardiovascular system;
- smoking, lung diseases;
- avitaminosis.
- anemia.
How to identify the disease? Let us repeat: if you suspect a disease, it is better to immediately consult a doctor, but diagnosis can be carried out independently. This diagnosis is simple and consists of an ordinary thorough examination of the lower extremities. So, you have a disease that urgently needs to be treated if, looking at your nails, you observe the following signs.
- Color change: it can turn white, yellow, blue, red, brown.
- Change in density: The nail plate may become very thin and brittle or too thick and stiff.
- Change in structure: if the nail plate has become “wavy” (longitudinal or transverse grooves have appeared on it), cracks have become noticeable.
- The appearance of painful sensations: the nail may hurt, for example, when walking, when pressing, or maybe at rest.
- Detachment of the nail plate from the nail bed.
- Inflammation and pain in the fingers.
- Discharge from under the nail plate of liquid with an unpleasant odor.
Various signs may indicate the presence of diseases of a fungal or non-fungal nature.
We carry out diagnostics ourselves
Ideally, the nail plate should be smooth, without grooves, tubercles, cracks or spots. The nail should not be white or peeling.
Take a closer look at your plates. If they grow poorly or break, it means your diet lacks nutrients and minerals.
Eat foods rich in calcium products.
Along the nail hole
Since ancient times it was believed that each nail is associated with a specific organ.
Diagnosis of health using fingernails begins with the holes: it is the nail holes that will first of all tell you which organ in your body is at risk and which doctor you should make an appointment with.
If at least one hole is absent on the fingers, it indicates a decrease in hemoglobin and red blood cells (anemia, anemia).
If the holes in your nails have become thinner or completely disappeared:
- Thumb – brain and skull. The ancients believed that if the hole on this finger disappeared, it meant that the person had serious problems with his head.
- Index – large intestine, liver and lungs, as well as inflammation and gynecological diseases. If the hole becomes smaller or disappears completely, urgently pay attention to the intestines, liver and pancreas!
- Medium – a disease of the circulatory system. If there is no hole, there is a problem with pressure and blood vessels.
- Unnamed - the hole reflects the state of metabolism and the lymphatic system.
- Little finger – problems with the cardiovascular system or small intestine.
This scheme is confirmed by an interesting observation. For most people, the most noticeable and lightest hole is on the thumbs, and this is no coincidence.
In the process of life, the small intestine is the first to become clogged - the socket on the little finger disappears, the endocrine system suffers - the socket on the ring finger becomes smaller. Problems begin with blood vessels and the heart, and only then does the large intestine give in. The brain holds on until the last.
Moreover, if the holes on all nails are unnaturally enlarged, this may indicate cardiac weakness.
By nail color
Look at your nails more often - diagnosing diseases begins with the smallest changes.
If your nails suddenly begin to change color, this is a sure sign of a problem in the body. A healthy person has beautiful pink nails. You need to listen to your body if:
1. Two-tone nail: the top is darker than the bottom.
Kidney disease, renal failure.
2. Dark stripe along the nail.
May indicate the development of melanoma (a malignant tumor of the human skin).
3. If the plates have turned brown.
Signals about kidney failure, Addison's disease, diabetes mellitus, thyroid disease.
4. The appearance of small white spots (leukonychia).
Reports a lack of iron, zinc and calcium. The body needs vitamins A, C, E.
If the spots grow, they take the form of stripes and appear in the area of the holes.
Symptoms of internal organ problems: protein deficiency, kidney failure, intestinal dysfunction, circulatory dysfunction.
5. Blue on the plates.
Informs a person about problems in the respiratory system. Infectious lung diseases (pneumonia).
If the nail turns blue near the base.
This indicates diabetes.
6. Completely white color of the plates.
It may appear in patients with liver cirrhosis or problems in the gastrointestinal tract.
May indicate poor-quality nail polish or liver and gastrointestinal disease. There may be chronic diseases of the lungs and lymphatic system. Indicate the development of jaundice.
8. Onychomycosis (fungal infection). The nail thickens, turns yellow, becomes cloudy and separates from the bed.
Fungal infections
As already noted, nail diseases are divided into two main types: fungal and non-fungal. Moreover, the former are found twice as often as the latter. The prevalence of fungal nail diseases is due to the fact that conditions are favorable for development: people wear shoes that are warm and humid. It’s interesting that fungus is different from fungus. There are three main types of fungal diseases that affect the nails, and each of them has its own symptoms.
Normotrophic diseases are characterized by the appearance of white or yellow spots, without changing the structure and thickness of the nail plates. Hypertrophic diseases, in addition to color changes (most often, the appearance of yellowness), are characterized by thickening of the nail plate with its subsequent detachment. Onycholytic diseases are similar to hypertrophic ones, but in this case the nail peels off from the skin almost immediately.
In most cases, fungal infections do not affect all nails at once, but separate ones (most often the thumb and little finger are affected). Diseases of the big toe are characterized by discoloration and severe thickening of the nail plate.
It is usually quite difficult to cure, so the disease must be treated by a specialist.
Diagnostic methods
At the first sign of a change in the shade of the nail plate, you should contact a dermatologist or nail specialist. Diagnosis in this case comes down to an external examination and the appointment of examinations aimed at identifying the cause that led to dyschromia. In this case, the patient may require consultations with specialists:
It is necessary to conduct a survey of the patient, it is necessary to find out how long ago the patient noticed changes in the color of the nail plates, find out about the presence of concomitant diseases, and find out whether there have been any injuries to the nail plate recently. In addition, a number of examinations are necessary. As a rule, the following tests are prescribed.
Cultural examination - bacterial culture on nutrient media. The technique is used to determine the type of bacterial or fungal infection and determine their sensitivity. The material for research is a piece of nail. The material is placed in a nutrient medium, and after a certain time measurements are taken and the types of microflora are determined. The analysis usually takes 7-10 days. During the study, the reaction of microflora to drugs is determined, this allows you to select the most effective treatment.
Non-fungal types of nail diseases
Non-fungal diseases arise mainly as a consequence of other diseases (possibly injuries) and affect all nails at the same time, most often on both the hands and feet. So, with psoriasis, the nail plate becomes whitish and peels off from the nail bed. Similar symptoms occur after mechanical impact - any injury. If any of the symptoms described below are present, diagnosis and treatment of the underlying disease and, as a result, nail diseases are necessary.
| Signs | Causes |
| Whitish color of nails (without peeling), white spots. | They may appear against the background of vitamin deficiency or after frequent use of varnishes. |
| Nails become yellow. | This happens in people suffering from lung diseases. |
| Nails turn black. | After mechanical impact and accumulation of blood under the nail plate. |
| They become very thick and also turn yellow. | For lichen ruber and dermatitis of various natures. |
| The nail plates may crack and split into several parts. | This happens with eczema. |
| "Wavy" nails with grooves. | They indicate a lack of calcium in the body. |
The most common non-fungal disease is nail dystrophy (in medicine - onycholysis). Dystrophy of the nail plates develops as a consequence of malfunctions in the digestive system, after a course of antibiotics and the resulting dysbacteriosis; dystrophy can also be of a nervous nature. Dystrophy is characterized by a change in the shape of the nail and its detachment from the nail bed. The nail becomes yellow-brown in color, and over time, if the disease is not treated, it disappears. Treating toenails after this disease and restoring their beauty can be extremely problematic.
If there is a suspicion that you or your loved ones have dystrophy of the nail plates, it is better to start treatment as early as possible.
Delamination
Quite often, parents are faced with the fact that their child’s nails peel and break. Why is this happening?
- This deviation causes:
- improper cutting of nails;
- lack of microelements, vitamins (vitamin A, E, B2, calcium, phosphorus, magnesium, zinc);
- mechanical damage. For example, nails on the hands peel if the child bites them or sucks fingers, on the feet - if he wears shoes that rub or squeeze the tips of the toes;
- health problems (iron deficiency anemia, adrenal dysfunction, onychomycosis).
In most cases, correction of nutrition, taking vitamin-mineral complexes, and rubbing vegetable oils rich in vitamins A and E into the nail plate helps to cope with delamination.
But if its cause is health problems, examination and tests will be needed.
Diagnosis of the disease
You can leave nail problems in the past and cure fungus forever only if you approach this issue comprehensively. It is not enough to treat nails using only antifungal ointments. Anti-inflammatory and immunomodulatory drugs are needed.
It is also not advisable to fix problems yourself. It is better if the treatment is prescribed by a specialist after a special set of tests. The fact is that it is very difficult to eliminate problems on your own, for example, to cure a fungus. You can only “preserve” it, but not cure the disease. Such “treatment” is not only ineffective, it harms the entire body and negatively affects the immune system.
Diagnosis of nail diseases involves interviewing the patient and examining the affected areas by the doctor. In the case of a fungal infection, in order to cure the nail, you will need to accurately determine the type of fungus. Diagnosis involves submitting a scraping and blood test for laboratory tests. In addition, diagnosing a problem (a disease of either fungal or non-fungal origin) is impossible without analyzing the general health of the patient, especially if he has immunological diseases, diseases of the cardiovascular and respiratory systems.
Toenail disease requires careful diagnosis and effective treatment. Otherwise, a careless attitude towards one’s own health can provoke infection and dysfunction of the lower extremities. Let's look at the main toenail diseases, their main causes, symptoms and treatment methods.
Why do marigolds turn black?
Considering that blackness under the nail can appear due to injury, it can be argued that the symptom does not even always indicate dangerous changes in the body. The discoloration itself is caused either by the accumulation of blood or its stagnation in the limbs. A change in the color of the horny tissue also only serves as a sign of trouble in the body.
- whether it is caused by a hematoma on the finger or the tissue of the plate is stained;
- 1 or more fingers are affected;
- what color the stratum corneum has: brownish or reddish or yellow, bluish, greenish;
- whether the child injured his hand (several fingers can be pinched by a door or drawer at once);
- the hematoma did not go away within 1-1.5 months (with or without nail detachment).
If there are concerns that the nails are turning black not due to injury, you should definitely show the child to the local therapist.
Blackening of the big toe nail is a problem that every second person has encountered. It causes aesthetic discomfort, forcing a person to look for ways to hide and disguise the defect. This circumstance makes treatment difficult: the vast majority do not attach any importance to the defect, ignoring it, hiding it under cosmetic varnish or closed shoes.
However, blackness under the nail on the big toe often acts as a harbinger of serious diseases, signaling internal failures and disorders occurring in the body. If you discover a suspicious darkening, do not be lazy to make an appointment with a podiatrist.
After conducting a series of diagnostic measures, he will determine an accurate diagnosis and draw up an effective treatment program.
Causes
Recent research in the field of podology has made it possible to identify the causes that can provoke darkening of the nail plate.
Conventionally, they are divided into two large groups: those that are internal in nature and those caused by external factors. We'll talk more about the nature of the development of the defect later.
Domestic
How to understand that the nail on the thumb has turned black due to failures and disorders occurring in the body? Without prior consultation with a specialist and passing certain tests - no way. If you want to identify the cause of the disease, do not delay going to the doctor - only he will be able to create an effective treatment program.
The toenail has darkened, the reason may be as follows:
- Fungus is one of the most common causes of blackening. During the life of fungal spores, the nail plate acquires a rich blue-violet hue, which begins to rapidly darken. The medical name of the disease is melanonychia. The risk group is represented by people suffering from autoimmune disorders, weakened immunity, and various hormonal imbalances. The disease often affects pregnant women, as well as adolescents during puberty.
- A benign tumor is another reason why the nail on the big toe has darkened. Pathological processes provoke the proliferation of blood vessels, which leads to a gradual change in the color of the plate.
- Excessive sweating is one of the most unobvious factors. Overactive sweat glands provide an atmosphere around the finger that is favorable for the proliferation of pathogenic bacteria. They cause the nail on the big toe to turn black.
- Vascular pathologies, in particular failures of venous outflow. Problems with circulation cause hemorrhage in the area of the nail plate and the formation of unaesthetic blackness.
- Diabetes. People suffering from this disease are most vulnerable and are prone to blackening and darkening.
- Avitaminosis. A lack of vitamins and beneficial microelements negatively affects the health of the nail plates, leading to a change in color, the appearance of dark spots and other defects.
Along with the listed factors, so-called systemic diseases are also distinguished: disorders of the cardiovascular system, renal and liver failure, endocrine pathologies.
External
Most often, the toenails of the big toe darken due to quite obvious and manageable reasons. Having a transient nature and being unrelated to internal failures, they are easily eliminated without causing consequences.
Treatment is limited to eliminating the irritating factor, without involving therapeutic measures. What could provoke the circumstances under which the nails on the big toes would turn black?
- Mechanical damage or injury. A change in the color of the nail to black, brownish or dark gray occurs due to hemorrhage. As a rule, the plate returns to its normal state after two to three weeks.
- Wearing uncomfortable shoes. This is especially true for women who spend a lot of time in narrow high-heeled shoes.
- External painting. If the toenail turns black, but does not hurt, the reasons for such metamorphosis should be sought in external factors. For example, new shoes impregnated with paints and pigments can provoke a chemical reaction on the surface of the plate. This will cause the color to change. To be fair, we note that this happens extremely rarely.
How can you tell if your toenails have turned black due to injury? Certified podiatrist Igor Demyanov answers this question: “Identifying this cause is not difficult. If you notice a slight blue discoloration on the plate, and only then part of the toenail has darkened, the diagnosis is strictly defined: blackening due to mechanical damage.”
Blackening of the toenails often indicates the internal state of the body. Correctly identified causes of darkening of toenails will help to begin treatment in a timely manner and quickly get rid of the problem.
Black toenails should not be hidden, but treated. The sooner the cause of the formation of dark spots is determined, the more effective the treatment will be.
| Factors influencing nail color change | Name of pathology | Description |
| External influence | Coloring or influence of chemical compounds on the skin of the fingers and the condition of the nails | 1. Human nails are naturally transparent. A strong solution of potassium permanganate can permanently color it dark brown or black.2. The use of low-quality varnish or liquid to dissolve it destroys the top layer of the nail plate, which leads to the appearance of dark spots. |
| Damage or bruises | 1. When the toes are bruised, the blood vessels rupture and a bruise forms under the skin.2. The use of tight shoes and excessive physical stress on the lower extremities also leads to ruptured capillaries and blackening of the fingers due to the accumulation of blood clots, clotted from constant compression. | |
| Internal changes | Systemic or chronic diseases | 1. The cause of the appearance of dark spots under the nails is often a disease of the cardiovascular system.2. Blackening of the soft tissue under the nails is also one of the symptoms of kidney failure and diabetes.3. A severe infection that has caused a decrease in immunity can cause black spots to appear. |
| Fungus | If the finger turns black, and after the nail plate grows back, the normal color of the skin is not restored, then a fungal infection has occurred. The disease is called melanonychia and is quickly transmitted from person to person if personal hygiene rules are not followed. | |
| Nail tumor (benign or malignant) | Blackening of the nail, which is accompanied by painful sensations when pressed, may indicate the growth of the vascular network and the formation of a tumor. At the same time, the color of the fingernails remains unchanged. |
We suggest that you familiarize yourself with Miliaria in a newborn baby: symptoms, causes, treatment. What does prickly heat look like?
A toenail has turned black (the causes of a cosmetic defect are often determined only after undergoing a medical examination) - a quick and correct diagnosis will speed up recovery.
| Doctor's specialization | When to contact |
| Therapist | If it is not possible to remember where and under what circumstances the injury occurred. |
| Endocrinologist | If renal failure or diabetes is suspected. |
| Dermatologist | If there are signs of fungal diseases. |
| Surgeon | If surgical intervention is necessary (nail removal, cleansing of purulent formations) |
| Oncologist | If there is a predisposition to tissue proliferation and the appearance of benign formations. |
| Orthopedist | If damage to the toes occurs due to wearing uncomfortable shoes. A specialist will help you choose special orthopedic shoes. |
Treatment methods
The toenail has turned black (the reasons and what to do in this situation, the doctor will tell you after determining the exact diagnosis) - treatment options are determined depending on the complexity of the damage.
For fungal infections, drug treatment consists of two parts: external treatment with ointments and internal administration of medications. Treatment is prescribed by the doctor after research, depending on the type of fungus.
| Name of the drug | Mode of application |
| Lamisil cream (externally). Analogue exifin ointment. | Apply 1 or 2 times a day to the nail bed and skin around the nail. |
| Fluconazole capsules (internal use) | Dosage for dermatophytic onychomycosis: 150 mg of active substance once a week until the nail grows completely. For safety reasons, do not exceed the doses indicated in the instructions. The duration of taking the drug can be from 7 to 12 months. |
| Fluconazole ointment (for external use) | Apply to the skin around the damaged nail and the area between the fingers once a day. |
| Terbinafine tablets | Take 250 mg once a day or 125 mg twice a day. Simultaneously with taking the tablets, externally treat the toes with Terbinafine ointment. |
Foot baths
For injuries and bruises, salt baths help relieve pain.
Preparation of the solution:
- Warm water (45 °C) – 2 l.
- Baking soda – 1 tbsp. l.
- Coarse sea salt - 1 tbsp. l.
- Iodine solution – 1 tsp.
Immerse your feet in a bowl of warm solution for 15-20 minutes. After the procedure, dry your feet. Before applying the medicinal cream, it is also useful to take salt baths.
Salt baths can be alternated with soap and soda solutions. To prepare, you need to take 50 g of crushed laundry soap and 1 full tbsp. l. baking soda. The ingredients are mixed with warm water and baths are made for 20 minutes.
What is the essence of the problem
We often think that only one nail plate belongs to a nail. And that to take care of it, it is enough to wash it and cut it. This is not true at all. Without exaggeration, we can say that the nail is a very complex system. It consists of a bed, a plate and rollers. There is 1 rear cushion and 2 side cushions.
The thickness of such a plate is from 0.5 to 0.7 mm. It consists of keratinized cells overlapping each other. It can only grow when the base (matrix) is intact. Accordingly, when injured, its entire structure changes, and in some cases the nail plate may be lost.
The matrix gradually turns into the cuticle. If it is damaged, the nail plate will not grow either. It can also be damaged as a result of fungal infection. Finally, due to improper growth, it grows into nearby soft tissues, which negatively affects its condition.
If you take poor care of your feet, do not comply with basic hygiene requirements, wear tight shoes, or expose your nails to injury, they will begin to become damaged. If you do not start treating these ailments, you may even lose your nails. Indeed, as a result of its loss, the functioning conditions of the lower extremities change. A person’s gait changes, his legs begin to hurt. All these phenomena affect the health of the spine. And the work of the whole organism depends on it, in turn. And of course, when the toenails are damaged, a constant source of infection is formed.
Diagnosis by fingernails
Even ancient people associated the appearance of nail plates with the condition of a certain internal organ. Today this has been proven by medicine, so it is often used to diagnose the body. Several characteristics are studied: color, structure, shape, hole and spots on the nail plate. Deviations for each of these criteria indicate a number of specific pathologies.
What does a healthy person's nail plate look like?
A nail plate without any cracks, tubercles, grooves, or spots is considered normal. It has an even pink color, a smooth surface, and a slight shine. The plate itself is slightly transparent, and the tips are white or ivory. The nail of a healthy person is moderately flexible, hard, and dense. At its base is a crescent-shaped lunula. Its color ranges from white to pale pink. The shape of the nail plate can be different, as it depends on hereditary factors.
Structure of the nail plate
When diagnosed, the surface of a healthy plate does not have pits, dents or bumps, is smooth, and evenly colored. It consists of dozens of layers of translucent smooth keratinized cells that are located close to each other. Thanks to its porous structure, it absorbs all substances that fall on its surface. This helps treat fungal diseases through local medications. When diagnosing, you can see several parts of the plate:
- eponychium is living skin at the base;
- hyponychium, or subungual plate - consists of spinous and basal cells;
- free leading edge – protrudes beyond the edge of the finger;
- lunula, or lunula, is a white area at the base in the shape of a crescent.
Claw nails
This disease occurs due to flexion of the metatarsophalangeal joint. This pathology occurs when a person wears tight and uncomfortable shoes and often exposes their feet to injury and frostbite. In older people, the claw-shaped form occurs due to progressive circulatory disorders (see photo).
At risk are all persons suffering from diabetes mellitus, inflammation of the joints, psoriasis, flat feet, including those who have suffered injuries to the legs and nail plate.
There are cases when such a pathology is congenital. The density of the plate is stony, there are grooves on it - longitudinal or transverse. They twist, and the petrified ones are somewhat reminiscent of ram's horns. Treatment of the claw form often cannot be done without surgery. The most preferred method of treatment is arthroplasty.
What is the norm
The nails of a healthy person are smooth, shiny, pale pink in color, with a pronounced whitish hole at the base. At the same time, the nail plate is constantly renewed, growing by about one millimeter in a week.
irecommend.ru
With age, the nail plate thickens and becomes more brittle. This is part of the body's natural aging process. Fragility is also characteristic of the nails of pregnant women. But within six months after giving birth, everything usually returns to normal.
It is acceptable if nails break due to a lack of vitamins or turn yellow due to poor-quality varnish. Sometimes the nail plate can even turn black and fall off if the finger is pinched or hit.
In a healthy person, fingernails are completely restored within 4-6 months, and toenails - within 6-8 months.
But there are persistent pathologies that we often don’t even pay attention to. But in vain. Some changes in the shape, color and texture of nails, as well as the skin around them, may indicate disturbances in the functioning of internal organs and the presence of a variety of, sometimes serious, diseases.
Psoriasis and eczema
The causes of psoriasis have not been precisely established today. The most common is to classify this disease as an autoimmune disease. With psoriasis, the plates begin to change long before pathological changes occur in the body. The more matrix is involved in the painful process, the higher the degree of damage to the nail (see photo).
With nail psoriasis, the following signs attract attention:
- recesses on the plates;
- separation of the plate from the bed;
- dryness and brittleness;
- subungual keratosis.
With eczema, the nail plate is also affected and splits. Sometimes, with an intense pathological process, it disappears altogether. Nails peel, become dry, dull and very thin. Transverse and longitudinal splitting of the plate is possible.
How to keep your nails beautiful and healthy
Here are the general recommendations given by Olga Aleynikova.
Proper nutrition, healthy sleep and exercise should be the default. Regularly inspect your nail plates and take care of your hands.
- Get a manicure and pedicure. Trim or file the free edge of the nails in a timely manner, and treat the cuticle.
- Don't bite your nails.
- Wear gloves when working with chemicals and when digging in garden beds.
- Take vitamins.
- Regularly smear your hands and nails with nourishing cream.
- Don't wear tight shoes, don't stick your fingers in cracks, and be careful with the hammer.
When going to places with large crowds of people, use liquid gloves (this is an emulsion). The risk of contracting infectious diseases through your hands is now very high.
If you see signs of illness on the nail plates, use antifungal agents and regenerating drugs. If the pathology is persistent, be sure to get tested and go to the doctor.
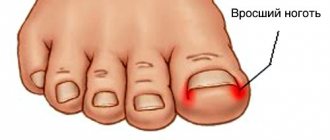
Ingrown nail pathology
An ingrown toenail is a very unpleasant disease. The nail plates cut into the soft tissue, sometimes causing such severe pain that the person cannot walk normally. Injured areas of the skin become swollen and infected as a result of ingrown nail plates (see photo). The incidence of this pathology is impressive: about 20% of people suffer from it. Some patients do not even realize that they are developing this pathology.
The most common cause of an ingrown toenail is improper cutting of the nail plate. The disease occurs when a person cuts corners. The growing plate, under the pressure of tight shoes, begins to grow into the skin. Narrow shoes, which press and compress the ends of the phalanx, are especially harmful to the nail plates. To prevent the development of such a pathology, it is necessary to cut off the overgrown end only in a straight line. The most characteristic signs are the following:
- constant pain that gets worse when wearing tight shoes;
- the presence of a sore on the skin in the place where the nail plate cuts into the skin and begins to put pressure on it;
- tissue proliferation on the affected side (the appearance of so-called wild meat);
- the appearance of wild meat is associated with the discharge of a large amount of purulent contents from the affected nail;
- The patient complains of walking problems.
The danger of an ingrown toenail is that it causes infection. With a pronounced infectious process, a local or even general increase in temperature is observed. The most dangerous complication of such a disease is blood poisoning or sepsis.
You can only cure an ingrown toenail on your own if the disease is in the early stages of development. It will be easy for a person to remove those particles that cut into the skin. It will be much easier to remove them if you place pieces of clean cotton wool under the affected nail. It is better to take a painkiller before this.
If conservative therapy does not bring results, the advisability of surgery is discussed. Traditional excision of the nail plate with a scalpel is gradually becoming a thing of the past. Nowadays, radio wave treatment and laser excision are increasingly used. The latter method is the most preferable because it is painless and does not cause complications.
In severe cases, complete excision of the nail plate may be indicated. The defect can be replaced using autodermoplasty. In this case, the nail will not grow.
How can you improve the condition of your nails?
The appearance of nails depends on many factors. Proper nutrition is of great importance in preserving and maintaining healthy nails. In order for nail plates to grow faster, your diet must contain foods containing calcium. A lot of this mineral is found in fermented milk products. People who want to strengthen their nails should definitely include cottage cheese, kefir and other foods containing calcium in their diet.
Nail care should be comprehensive. Thus, various cosmetic products can be used to treat nail plates in order to improve their appearance. For example, you can improve the color of your nail plates and reduce their fragility using cosmetic nail polishes. Such products, for example, are produced by Phytocosmetic, Eveline Nail Therapy Professional and many others.
Fungal infection
Nail fungus (or onychomycosis) is quite common. The plate is affected by various types of microscopic organisms, including mold and yeast. The most favorable conditions for the proliferation of such microorganisms are in a dark, cramped, damp and dirty environment. The thumb and little finger are most likely to be affected. This is caused by rubbing the nail plate with tight shoes.
Children are less susceptible to fungal infections of the feet. And the older a person is, the greater the risk of developing nail fungus. By the age of 50, almost 70% of people have experienced fungus to one degree or another. In the photo you can see what such a violation looks like. The predisposing causes of fungal infection of toenails are the following factors:
- insufficient foot hygiene;
- use of public swimming pools, baths and saunas;
- diabetes;
- immunodeficiency;
- some cardiovascular diseases.
Symptoms depend on the degree of infection. The lesion gradually begins from the free part of the nail plate. The earliest sign of pathology is the appearance of spots and stripes on the nail. The affected nail crumbles very easily and intensely. With atrophic onychomycosis, it becomes thinner, and keratinized skin is visible underneath. If the nail plate is affected by mold fungi, it gradually takes on a different color - blue, black, brown and even green.
Getting rid of fungus can be very difficult. Contrary to popular belief, it never goes away on its own. If you do not treat the diseased nail, then a large area of the nail plate may be damaged. Ultimately, it may need to be completely removed.
The doctor prescribes antifungal ointments and sprays to his patients, which are applied to the nail plate. All medicinal formulations should be used only for their intended purpose. In severe cases, it is necessary to take antifungal drugs orally. You should be very careful because some antifungal medications can cause side effects.
Features of the course of various nail pathologies and methods of their treatment
Therapy for any disease must begin with an understanding of the cause of its occurrence. Self-medication can be dangerous to your health. If the first symptoms of pathology occur, contact a doctor who can provide you with timely medical assistance.
Onychomycosis
Onychomycosis is a fungal infection of the nail, which is most often caused by fungi of the genus Candida or Trichophyton rubrum. Symptoms appear gradually: first, white or yellowish cloudy spots form, then they merge and the entire nail plate changes color. The nail begins to crumble and may take on the shape of a bird's claw (onychogryphosis).
Nail destruction can be basal, distal (when the nail is affected at the free edge) or can occupy the entire nail surface. When you press on your finger, pain may occur. In addition to the nail plate itself, the soft tissues that surround the nail are also affected: they become dry, itching, cracking and peeling appear.
The fungus can affect one or several fingers at the same time
Onychomycosis has 3 forms:
- hypertrophic;
- normotrophic;
- atrophic.
Depending on the form of the disease, the symptoms will differ from each other:
- with normotrophic, spots and lines of cloudy white, yellow, brown or orange appear, but the shape and thickness of the nail remain normal;
- with hypertrophic nail plate dulls, loses its shine, and may become yellow. Over time, the nail crumbles and becomes deformed;
- with atrophic, most of the nail plate is destroyed, the nail becomes dark in color, and its complete detachment is possible (onycholysis).
Treatment of pathology
Treatment of the disease depends on the degree of damage to the nail and the severity of symptoms. The specialist prescribes complex or local therapy aimed at destroying the fungal outbreak and accelerating the healing of the nail plate. Only a doctor can choose the correct treatment tactics after performing cultures on nutrient media and assessing the results obtained.
Local therapy is used for superficial damage to the nail and includes the use of antimycotic varnishes, ointments and gels. For more serious lesions, complex therapy is used with the prescription of systemic antimicrobial drugs, such as:
- Fluconazole;
- Exoderil;
- Itraconazole;
- Nitrofungin, etc.
Fluconazole inhibits the activity of fungal enzymes, disrupts their growth and reproduction
I applied Nitrofungin for five weeks just to prevent the fungus from returning. The downside is that Nitrofungin contains a high concentration of alcohol, which makes the skin look like tanned. But this disadvantage is offset by high efficiency. Already from the third day of use, the itching disappears and the skin begins to slowly recover. A huge advantage is that you do not need to apply ointment, cream or gel, but simply wipe the skin with a moistened cotton swab.
ek9345
https://otzovik.com/review_978731.html
In advanced stages, when the nail plate is deeply damaged, it is necessary to perform an operation to remove the nail with further antiseptic and antimycotic dressings.
Video: dermatologist about onychomycosis
Nail psoriasis
Nail psoriasis occurs against the background of psoriasis and occurs in 80–90% of patients. The cause of its occurrence has not yet been fully studied, but there are versions that the disease is based on an immune disorder and a genetic predisposition.
Psoriasis can manifest itself with the following symptoms:
- the appearance of pinpoint dents on the nail plate, as if it had been pricked with a thin needle (the “thimble” symptom);
- loosening of the nail plate;
- painless detachment of the nail from the finger.
Often, hemorrhages and dirty yellow spots are observed under the nail plate. The soft tissues surrounding the nail also suffer - peeling and severe itching appear.
When the nail plate separates, a secondary infection, bacterial or fungal, may occur
Treatment of the disease
Psoriasis requires professional comprehensive treatment. In order to correctly diagnose, the doctor needs to collect a history of the disease and take a scraping scraper from the affected area. This study will help distinguish psoriasis from fungus or other nail pathologies. Treatment is prescribed comprehensively, taking into account the individual characteristics of each patient. For external therapy, hormonal and antimicrobial ointments and special healing varnishes are used. Among medications, antihistamines and mineral complexes enriched with zinc and calcium come first. It is recommended to follow a diet high in protein, vitamins A, D, E, C, P and group B (B1, B2, B6, B12, B13, B15). Drinking alcoholic beverages is prohibited; it is advisable to limit the amount of salt, fats and carbohydrates consumed.
Recommended Products:
- fruits (except black currants, prunes, blueberries, cranberries);
- vegetables (except for legumes, sorrel, Brussels sprouts, tomatoes, potatoes, peppers and eggplants);
- freshly squeezed fruit juices (especially pear, apricot, pineapple);
- freshly squeezed vegetable juices (from carrots, spinach, parsley, onions).
Products to exclude:
- berries and fruits: strawberries;
- strawberries;
- currant;
- prunes;
- cranberry;
- tomatoes;
- anchovies;
In the treatment of nail psoriasis, the psycho-emotional state plays an important role: try not to be nervous, be in a positive mood.
Among medications, Losterin cream has proven itself well.
Losterin is a non-hormonal drug intended for daily skin care.
During all this time, I probably tried everything possible. I saw Losterin at the pharmacy by accident. It's obvious that it's non-hormonal. In general, now the hands are certainly not quite ideal, and not like they were before. Although there are no cracks or bubbles and the skin does not peel off. Dry and slightly red, but just a little.
oksankopaev
https://otzovik.com/review_1426468.html
Onychoschisis
Onychoschisis is a transverse separation of the nail. The nail plate becomes significantly thinner and is divided into several sheets. The disease is dystrophic in nature and can be caused by a number of factors, such as:
- poor nutrition;
- nervous overstrain;
- injuries;
- insufficient iron and calcium levels in the blood;
- use of low-quality varnishes;
- injuries;
- systemic diseases (psoriasis, eczema, diabetes);
- fungus and so on.
Onychoschisis can occur in both men and women
Visually, the nail does not change color and retains a healthy shine. It grows normally until the middle, after which it splits into two plates. Today, onychoschisis occurs in people who play keyboard instruments, work with the keyboard for a long time, and keep their hands in alcohol cleaning solutions for a long time. If previously the most common cause of the disease was old age, now it also occurs in young people.
This type of dystrophy is observed mainly in women who often use manicures using varnishes, acetone, and also with frequent contact with synthetic detergents.
Doctor Khoroshev
https://horoshev.ru/letters/izmeneniya-nogtevyx-plastinok/
How to treat the disease
Treatment of onychoschisis begins with eliminating the factor that led to the disease. For example, if the lesion is of a mycotic nature, antifungal drugs are prescribed, and if the cause lies in mechanical damage, then it is necessary to limit the impact of this factor. For the speedy regeneration of the nail plate, vitamin complexes with retinol and cyanocobalamin, a solution of edible gelatin, massages and physiotherapy are used. On average, treatment lasts from 4 to 8 weeks.
Felon
Panaritium is a purulent inflammation of the soft tissues of the fingers, which is most often found on the palmar surface of the hand. The main cause of the disease is the entry of pyogenic bacteria through cuts and abrasions. Usually felon develops quite quickly, and it is almost impossible not to notice this disease, since it is accompanied by local swelling, redness and severe throbbing pain.
The danger of panaritium is that, due to the peculiarities of the anatomical structure of the finger, purulent inflammation can spread deeper, touching the tendons, joints and bone
Depending on the location and degree of tissue damage, the following forms of panaritium are distinguished:
- cutaneous;
- periungual;
- subungual;
- subcutaneous;
- bone;
- articular;
- osteoarticular;
- tendinous.
How to get rid of pathology
If panaritium occurs, you must immediately contact a specialist! Using a button probe and x-ray, the doctor will determine the extent of the damage to the finger. Depending on the severity of the disease, conservative or surgical treatment is used. In mild cases, antibiotic therapy, UHF, and thermal procedures are prescribed in the early stages. In the later stages, the purulent focus is dissected with its further drainage.
Video: suppuration on the finger - felon
Onychocryptosis
Onychocryptosis, also known as ingrown toenails, is a fairly common problem that people consult with doctors. There are several reasons for this disease:
- wearing tight and uncomfortable shoes;
- injury;
- presence of fungus;
- heredity;
- improper manicure (too short, arched nails) and so on.
Onychocryptosis is accompanied by redness of the tissues into which the nail has grown, their swelling, and pain when pressed and touched. With a long course of the disease, the periungual fold can thicken due to the proliferation of connective tissue against the background of chronic inflammation.
When an infection occurs, purulent inflammation of the periungual fold may develop.
Treatment methods
If the nail has grown slightly, then conservative therapy can be used. In the early stages, baths with soda and potassium permanganate are used, and with the help of cotton pads they try to correct the angle of the nail. It is not advisable to cut off the edge of the nail plate; it is best to correct the shape by filing it down. A specialist will be able to install special plates that will change the shape of the nail. In later stages, such therapy will be ineffective, and only surgical treatment will help. The essence of the method will be resection or complete removal of the nail plate.
Nail plate installation is a modern alternative to surgery
Photo gallery: types of nail deformities
Two-tone nails occur in 10% of patients with kidney failure
Blue nails may indicate Wilson's disease or alkaptonuria
This type of deformity (Koenen's tumor) occurs in Bourneville's disease, a hereditary disease that affects the nervous system and skin.
Onycholysis occurs with onychomycosis, nail injuries, after exposure to chemicals, with psoriasis
A concave (spoon-shaped) nail shape may indicate chronic iron deficiency anemia or Plummer-Vinson syndrome
Nails in the form of drumsticks are found in diseases of the cardiovascular system (congenital heart defects) and pulmonary pathologies (bronchiectasis, malignant neoplasms)
Is nail plate injury dangerous?
Toenail injuries occur quite often - due to a fall or unsuccessful movement, as a rule, the main consequence of the injury is a bruise or hematoma. The appearance of a hematoma is caused by crushing of soft tissues.
If any heavy object falls on the nail or a strong blow to the finger occurs, then due to the hematoma the nail plate becomes red, purple and even black. Pain of varying intensity always appears against the background of an injury - from dull to very sharp. A hematoma can be of different sizes - from an inconspicuous spot to a large spot. The nail plate can often become damaged.
In case of nail injuries, you should always contact a traumatologist. In some cases, he prescribes an x-ray examination of the affected area. And only when the specialist describes the x-ray image, the necessary treatment is prescribed. You should immediately consult a doctor in the following cases:
- when hitting the nail causes severe swelling, redness of the nail and pain;
- when discharge appears from the affected nail;
- when the plate falls off;
- if the patient suffers from diabetes, neuropathy or pathology associated with the condition of the arteries.
Injuries do not always lead to the formation of hematomas, plate detachment and other pathologies. However, to rule out any changes in the nail, you should consult a doctor.
Form
Healthy nails usually have a longitudinal shape. In some cases they become spoon-shaped. In this case, the center of the nail seems to bend inward, and the edges rise. Interestingly, these changes are not accompanied by the appearance of adverse symptoms. A person with such nails does not experience pain. And also, the nail plates usually have a shiny appearance. This condition is called koilonychia.
You can suspect her yourself. To do this, place a small drop of water on the nail. If the water calmly rolls off the nail plate, then there is nothing to worry about. If a drop of water seems to “get stuck” on the nail, then this most likely indicates the presence of koilonychia. This condition may be a sign of problems in the endocrine system. Koilonychia can also be caused by anemia, which is accompanied by a decrease in iron concentration in the bloodstream.
This condition can be caused by various traumatic injuries, exposure to chemicals, and even changes in ambient temperature.
Spoon-shaped nails can also be hereditary. So, if a child has such nail plates from birth, and one of his parents also has spoon-shaped nails, then in this case there is no need to worry. This does not mean at all that the baby has any diseases. This is just an individual characteristic of the child.
In some cases, nails may take on the shape of “watch glasses.” In this case, they begin to become thicker. If you look at the nail plates from the side, you can see that they resemble watch glass. Such a change in the shape of the nail plate can be a manifestation of various pathologies. Such changes often occur with various diseases of the respiratory system, accompanied by a decrease in oxygen concentration in the blood.
If your nails change color, this most likely indicates that various changes are occurring in the body. For example, yellowing of the nail plates is more likely to indicate problems with the liver and gallbladder. Biliary dyskinesia, which is accompanied by stagnation of bile, can also lead to such specific changes. The nail plates can be affected by fungus. In this case, they may have a yellow or in some cases even purple color. With a fungal infection, the nail plates begin to crumble severely.
Important! The fungus occurs on both feet and hands.
A black streak may suddenly appear on your nails. Trauma can lead to the appearance of such a clinical sign. So, a dark stripe may appear on the nail after it is pinched, for example, by a door or cabinet door. If there was no factor preceding the appearance of a dark stripe on the nail, then you should definitely consult a doctor.
Other diseases
Toenails can be affected by other pathologies. Some of them require immediate treatment. Here are some of the toenail diseases:
- clouding of the nail plate (leukonychia);
- separation of the plate from the nail bed (onycholysis);
- blackening of the nail (melanonychia);
- thickening of the nail bed (this disease is known as hyperkeratosis);
- yellowing of the nail (chromonychia) due to poisoning or taking certain medications;
- inflammation of the cushion located around the nail (paronychia) as a result of inflammatory processes in the body or an allergic reaction;
- nail separation (often develops if there is not enough calcium in the body, accompanies some cardiovascular pathologies and various endocrine disorders).
If a person has a toenail disease, the first thing to do is consult a doctor to prevent complications from developing. There is no need to try to find any medicine for nails on your own, or carry out various manipulations.
Fingernails and toenails are no less susceptible to various diseases than other parts of the body.
They are fungal and non-fungal in nature, which affects a variety of causes.
In some cases, the state of health of the nails can tell about diseases occurring inside the body.
Therefore, today we will look at common nail diseases, the causes of their appearance and treatment methods.
Diseases of the fingernails or toenails may appear.
Very rarely it affects the nails of all extremities.
What other nail diseases are there: photos and descriptions
Koilonychia
Koilonychia
, ,
is one of the common forms of onychodystrophy. This form of the pathological process is characteristic exclusively of the fingers of the upper extremities.
With the development of this nail disease, the following symptoms are observed:
- the surface of the nail plate becomes concave;
- the nail becomes smooth;
- the thickness of the nail remains unchanged.
Koilonychia occurs as a result of mechanical damage to the surface of the nail body, for example, with prolonged exposure to alkalis and acids. In addition, the development of this nail disease can also be caused by various pathologies - onychomycosis, Addison's disease, typhoid fever. In rare cases, this pathology is congenital and hereditary.
Symptoms of a fingernail disease called koilonychia in the photo.
Platonychia
Platonychia _
)
is a pathological process in which the nails have a completely flat surface.
It is predominantly a congenital anomaly, but can also be acquired through exposure to occupational factors. The occurrence of certain chronic inflammatory processes in the body, for example, liver cirrhosis or psoriasis, also causes such changes in the nail plates.
Transverse grooves
Bo's furrows or Bo-Reilly's furrows are other names for this pathological process. The pathological process is the result of exposure to exogenous and endogenous factors on the nail plate. The depth of the groove (groove) formed on the surface of the matrix indicates the depth of the lesion and the degree of development of the disease.
Bo's furrows do not differ in color from the rest of the nail plate. The depth of such pathological formations can reach up to 1 mm. The reasons for the development of pathology may be different. This nail disease often occurs in children when they receive trauma to the nail body during childbirth. In most cases, transverse furrows are detected between the 20th and 43rd days after the baby is born.
In adults, pathology can occur against the background of severe infectious and skin diseases.
This photo will help you become familiar with the signs of this nail disease, the description of which is provided above.
Longitudinal furrows
This disease occurs mainly in older people with age-related changes in the structure of the nail plate. Sometimes longitudinal grooves are formed in young people with certain diseases, for example, with lichen planus.
This nail disease, described above, is demonstrated in this photo.
Gapalonychia
The term hapalonychia
)
denotes a process in which the nail plates soften, as a result of which they easily break and split at the free edge.
With this disease, the nails become fan-shaped. There may be several causes for hapalonychia. They distinguish true hapalonychia, which occurs as a result of pathological processes occurring in the human body such as endocrine dysfunction, spastic paralysis, and metabolic disorders. Hapalonychia is also known, which occurs with prolonged and regular local exposure of the nail body to alkalis, acids, solvents and other aggressive chemicals.
Onycholysis
Onycholysis _
)
– a disease of the nails, in which their complete or partial separation from the nail bed occurs.
Usually this process occurs from the free edge, but the nail plate can also separate on the sides. The parts that have separated from the nail bed are whitish-gray in color. Experts name several reasons for the development of this pathological process:
- intoxication of the body;
- neurotrophic disorders;
- injuries;
- skin diseases - eczema, congenital epidermolysis;
- bacterial and fungal infections, for example, rubromycosis of nails.
Onychomadesis
Onychomadesis _
)
– complete separation of the plate from the nail bed.
The name of this disease has a synonym – onychoptosis. Unlike onycholysis, onychomadesis is accompanied by separation of the nail plate not from the free edge, but from the posterior - proximal, at its very base. This pathological process occurs in a very short time and may be accompanied by inflammatory phenomena.
Onychorrhexis
Onychorhexis _
)
is a pathological process accompanied by brittleness of nails and their splitting in the longitudinal direction.
Onychorrhexis is often the result of endocrine disorders in the body, various skin dermatoses - eczema, psoriasis, lichen planus. Among the reasons for the development of onychorrhexis, experts also name various types of mechanical damage and occupational injuries. Not all nails may be affected, but only on individual fingers; on the feet, such a pathological process is rarely detected.
Onychoschisis
Onychoschisis _
)
– a disease in which the nail splits in the transverse direction parallel to its free edge. One of the main reasons for the development of this pathology is frequently repeated mechanical damage to the nail. This can happen to musicians who play the violin, and women who are overly keen on manicure.
Common causes of nail disease
Common causes of disease of the nail plates and nearby tissues are:
- Fungal infections
- Non-fungal infections
- Dermatitis
- Injuries
- Improper care
- Bad habits
- Age-related changes
- Genetic predisposition.
Diseases of the circulatory and cardiovascular systems can provoke changes in the nail plates.
In the first case, the nails become bluish in color, and in the second, bright red. With anemia they become pale.
It is worth noting that with diseases of the respiratory tract, in particular the lungs, changes such as thickening and/or the appearance of a yellow tint may appear.
However, this is also possible due to smoking. But yellowish nails with a blue base are a sign of diabetes.
What does nail color say?
Since the nail plate itself is translucent, ideally the color of the nails is pink, uniform, and whitish at the grown tips. The lunula, a moon-shaped spot at the base of the nail, has a lighter shade. The disappearance of lunula indicates a weakened state of health in general, low immunity and lack of energy, possibly a serious illness. With rest, restoration of internal resources and strength, the nail moons return to their nail firmament.
It is normal for nails to become slightly white and even blue when exposed to frost, which quickly disappears in warm conditions. You should be wary if your nail color is:
- pale, whitish as a result of iron deficiency anemia or diseases of the liver, kidneys, spleen; leukemia and other forms of cancer can also lighten the color of the nails; metabolic disorders, unbalanced menu and lack of vitamins can also cause whitening;
- pronounced white color of nails - possibly the result of liver cirrhosis, nephrosis, Addison's disease, poisoning or shock, dysfunction of the adrenal glands;
- yellowish - may indicate poor liver health, jaundice; fungus and long-term use of varnish in women also cause yellowing of nails;
- yellow-greenish - indicates a long-term inflammatory process with the formation of pus, abscesses, for example, sinusitis or tonsillitis; fungal infections give an uneven yellow-green color to the nail;
- redness of the nail plate may be a consequence of overwork, disturbances in the functioning of the heart, kidneys, or blood circulation, when blood stagnates in small vessels or erythremia occurs;
- brown - indicates a fungus, long-term blood stagnation, fever;
- bluish , sometimes with a purple tint - a consequence of tissue hypoxia due to disturbances in the functioning of the cardiovascular system.
Common symptoms of nail disease
Symptoms of nail disease can be different, as they depend on the type of disease.
However, it is worth paying attention to the following signs that signal a pathological process on the nail plates:
When nails are infected with fungi, nearby tissues often suffer. Mostly inflammatory foci are located between the fingers. If not treated promptly, they can spread throughout the entire limb.
Nail diagnostics
Experienced doctors can even use early diagnosis using fingernails to determine the condition of the body, because concave, convex or too flat nail plates cannot be considered healthy. Such deviations indicate certain problems, sometimes requiring serious treatment. Medicine confirms that the condition of the nail plates directly depends on human health. They are used to diagnose fungus, lung problems, anemia and other pathologies. There are several criteria for determining the disease by fingernails.
Non-fungal nail diseases: types, signs and treatment
We can talk about a non-fungal nail disease if there are concomitant diseases, changes affect the nail plates on all extremities and appear simultaneously.
However, this does not provide a 100% guarantee of the absence of fungal microflora. According to static data, every second nail disease is caused by a fungal infection.
Still, you shouldn’t immediately panic, since nail diseases of non-fungal origin have characteristic signs:
It is advisable to entrust the treatment of non-fungal nail diseases to a specialist. Especially if they are caused by concomitant illnesses. This is due to the fact that fungal nail diseases mainly appear as a result of improper treatment of non-fungal ailments.
Untimely treatment can lead to loss of nails, and since their health reflects the state of the body, the risk of unwanted consequences increases.
Diagnosis of health using fingernails. Photo
Diagnosis using fingernails is a method with a long history. Even in Tibet, and even in Ancient China, doctors perfectly mastered the science of determining the state of health by nails.
Modern doctors confirm that the condition of the nails can indicate the beginning of problems in the body, even when serious diseases are far away.
There is a direct correlation: nails - health - nail diagnostics will help you find emerging problems, especially if you use several nail diagnostic methods at once.
Fungal nail diseases: types, signs and treatment
In most cases, fungal diseases of the toenails appear. This is due to the fact that there are more favorable conditions for the development of fungi.
Increase your risk of developing a fungal infection on your toenails:
Fungal infections can form on the hands due to the use of an “infected” tool by a manicurist. This is due to improper processing of the tool after the previous client.
However, the carrier of the infection does not always have visible signs of the disease.
To consider the types of fungi in more detail, we can roughly divide diseases into 3 types:
- Normotrophic. With diseases of this type, nails can become white or even bright yellow. Spots or stripes are observed on the nail plates, which after a while affect their entire area and do not extend to the hole. At the same time, the nails themselves do not change shape and thickness for a long time.
Hypertrophic. The diseases manifest themselves in the form of thickening of the nail plate, the appearance of yellow stripes and white spots on it. Over time, it can become depleted, leading to its complete loss.
Onycholytic. Nails begin to quickly fade, become cloudy or acquire a yellowish tint. During fading, their separation from the nail bed is noted, starting from the free edge. The surface of the nails remains unchanged, it is just as smooth.
You can find out the cause and type of fungal infection by other signs. For example:
- Mold fungi: thickening of the nail plate, which does not change its color for a long time. Spots appear through it, which can be of different shades - gray, green, brown, yellow, black.
Athlete's foot, which affects the nail plates of the big toes and little fingers. Toenail disease is characterized by thickening of the plate, yellow spots or stripes appearing. As a result, they are destroyed.
Candidiasis: mainly affects the skin near the posterior periungual fold. It turns red and shines. The nail fold swells and a cheesy substance may separate from it. As a result, the nail skin disappears.
Treatment of a fungal infection on the nails involves a complex of measures. Antifungal ointments and immunomodulators, multivitamins are mainly prescribed.
The use of ointments chosen independently is not recommended. They should be selected depending on the type of fungus. For these purposes, the dermatologist uses a scraping and refers the patient for a general examination of the body.
In quite rare cases, treatment of toenail disease involves the need for surgical intervention.
It consists of excision of the damaged area of the nails or their complete removal.
However, this method is used if the lesion affects almost the entire area of the nail plate and will interfere with its normal development.
Therefore, in order to prevent the development of the disease and begin timely treatment, it is undesirable to experiment with folk remedies. After all, fungal infections are toxic, which leads to a general weakening of the immune system and an increased risk of secondary diseases.
Nail atrophy
A deviation that may result in changes in the thickness, width and shape of the nail. As in the case of anonychia, it can be congenital and acquired. The first option is more common in medical practice.
And another place in this area is the general showers that athletes use after sports and rely on them to stay clean. When traveling, you'll most often find uniforms in hotel rooms and showers because they do contain a lot of fungal pathogens. We recommend wearing a girdle to prevent infection.
Even in your own home, you can catch a fungal nail infection. If you have a family member who has nail fungus, this is another method of transmission. But the most common victims of nail fungus are people with weakened immune systems, the elderly and people with sugar.
Nail atrophy can be caused by systemic diseases, as well as dermatological diseases such as lichen, psoriasis or fungus.
Atrophy N. Severe stage. N. is strongly exfoliated and softened.
In some professions, such as workers, craftsmen, gardeners, foresters and others, they must use durable shoes. But even tough boots and sweaty feet create a humid, warm climate that is ideal for mold. For these activities, your doctor should do regular checkups to make sure you don't have nails.
Preventive measures against nails
- Don't wear tight shoes against your toenails—there should be no pressure on your feet.
- Against mold, you need to take care of your nails with regular manicure.
- It is effective against mildew to cut the nails as much as possible.
Anyone who has ever suffered from nail athlete's foot is still at risk because they can get their nails in shape again.
Regular examination of your nails is recommended to find out if there are any other new symptoms of a fungal infection. Signs of atrophy:
- Deformation of the surface of the nail plate;
- Nails become dull and take on a gray tint;
- It may crumble and become thinner;
- Softening the plate;
- Instead of a smooth surface there is an abundance of flaws and inclusions.
A type of nail disease in which the nail plate peels away from the nail bed. In advanced cases, the nail may die. The disease begins with partial onycholysis, when one of the edges peels off. As the disease progresses, the area of detachment increases.
In public places such as swimming pools, saunas, hotel rooms, simply enter in slippers. Use thin, breathable cotton socks that make your feet feel so light. Change your socks daily. Change your shoes as much as possible. Disinfect your shoes regularly.
- Use only your own towels to dry your feet.
- Make sure your feet are dry, especially between the toes.
Fungi that cause nail infections are found in our environment because they love warm and humid conditions.
A normal healthy nail does not become infected so easily, in most cases a fungal infection can lead to a weakened immune system, various diseases or injuries to the nails. Recognizing the shape is easy because the color of the nail is changed, which can also start to crumble. If you have a fungal infection, treatment is necessary. The doctor diagnoses the fungal infection under a microscope from a sample of the nail or uses a fungal culture.
Onycholysis. All N. on the hand are affected. On N.'s ring finger, the plate peeled off in half. The disease is advanced.
The causes of this defect are varied. These may be: systemic diseases, fungal infections, lack of microelements in the body, side effects of taking potent drugs and antibiotics.
A fungal nail infection can be treated externally or with medication. The duration of treatment depends on the degree of mold development. Mild to moderate fungal disease does not exceed 50% of the nail. Onychomycosis with less than 50% of the nail or nail infection is an external local treatment. The key to success in treating all nails with fungal disease is early onset.
If infection accounts for more than 50% of the nail, treatment with oral medications should begin with systemic therapy. The correct form of treatment should be determined by diagnosis and by a dermatologist. Maintenance treatment is a carefully performed medical pedicure in which the nails are professionally treated by a doctor. Pedicures help keep feet healthy and mold-free.
Symptoms of onycholysis are as follows:
- Formation of emptiness under the nail;
- The smooth dividing line becomes abrupt at the end;
- Loss of sensation in the nail pad;
- Loss of pink color.
Video
A nail affected by fungus weakens, may crack or become rough, change color, peel or crumble. Irregularities or growths appear on the surface of the nail.
Fungal infections cause fluid to accumulate under the nail plate; a bruise may appear on its surface, and the nail itself becomes deformed and becomes an unnatural color. This happens especially often with the nail plate of the big toe. The fungus very quickly spreads from damaged to healthy areas of the nail and neighboring fingers.
Fungal infections can affect the nails due to improper foot care. People who regularly use saunas, swimming pools and other crowded establishments can become infected with the fungus. Factors that increase the risk of developing fungus also include flat feet, poor-quality shoes, increased sweating of the feet, and diaper rash.
At an early stage, foot fungus is treated with external agents with antimycotic properties that act on the pathogen at its location. These products are available in the form of a spray, gel, ointment or varnish and provide the desired effect only for minor manifestations of fungal infections.
Advanced fungal infections that have affected more than half of the nail or several nails cannot be cured with external ointments alone. In this case, their complex treatment is used, which consists of medicinal ointments and tablets.
One of the diseases that most often affects toenails is fungus. Fungal infections can have different pathogens, but are expressed by similar symptoms.
Osteomed – health and beauty of your nails!
Osteomed can be safely used to restore and maintain the beauty and health of nails, hair and teeth, and also as a means of preventing osteoporosis. The key difference between Osteomed is a small amount of calcium with guaranteed delivery to the main bone storage areas - bones, nails, hair, teeth. The harm of large doses of calcium is well known today.
What, when using Osteomed, guarantees the delivery of calcium to the right places, and not to the vessels and soft tissues? Firstly, it is the presence of the most digestible, effective and safe form of the mineral - calcium citrate. And secondly, drone homogenate as part of Osteomed . This natural component not only helps to establish mineral metabolism and delivers calcium to its intended purpose, but is itself a unique natural complex of amino acids, vitamins and minerals. Osteomed is a healthy choice for beautiful people!
Sources:
https://sovets24.ru/998-diagnostika-po-nogtyam.html https://www.blog-o-krasote.ru/post-diagnostika_po_nogtyam_palcev_ruk.html https://osteomed.su/diagnostika-po-nogtyam/
Ingrown nail
Orthopedic doctor Anatoly Shcherbin: “It is known that for the treatment of bunions there are special insoles, correctors and operations that are prescribed by doctors. But we will not talk about them, and those medicines and ointments that are useless to use yourself at home. Everything is much simpler..."
Ingrown nails into the skin must be treated comprehensively. Another common foot disease is an ingrown toenail. An ingrown nail occurs when it is trimmed incorrectly and untimely. When people cut the corners of their nails, they leave sharp ends that can dig into the skin and create small wounds. Infection easily penetrates these areas. After this, redness occurs in the area of the ingrown nail, it swells and hurts. The inflamed area oozes yellowish fluid.
Ingrown toenails most often occur on the big toe. Ingrowth should be treated using several methods:
- Shoes should be comfortable and wide, without heels, and tailored to the size of your feet. Pointed-toe and square shoes contribute to finger rubbing and ingrown toenails. Feet should take a break from shoes as often as possible.
- Foot care should be timely and correct. Be sure to regularly wash your feet in warm water. You should choose simple soap, without harmful dyes that can cause allergies.
- It is necessary to make foot baths with the addition of soothing medicinal herbs.
Sea salt relieves inflammation and redness well. The affected area should be washed with a disinfectant solution of potassium permanganate or furatsilin. The ingrown area should be wiped with hydrogen peroxide. It is imperative to show the problem to a dermatologist. The doctor will prescribe medications to facilitate the healing process or, in severe cases, refer you to a surgeon.
If you do not respond to an ingrown toenail, the wound will fill with pus. If left untreated, over time, the ingrowth can turn into an abscess that will have to be operated on.
Symptoms of the problem
It is not uncommon for people to notice a blackened nail on their hand or toe. The transparent plate becomes purple or bluish, the darkening is limited in size or covers the entire surface, sometimes the surface changes its shape. As the process progresses, the stratum corneum may peel off and fall off. In some cases, several fingers darken.
Painful sensations do not always accompany the process. Pain may appear if you press on a black nail, but sometimes it torments a person constantly. Some diseases are not accompanied by pain, and the plate only changes its color.
Hematoma formation
Nail diseases also develop due to mechanical damage to the fingers. Injury can be caused by a blow from a heavy object, resulting in bleeding and hematoma formation. The nail takes on a blue tint, which indicates burst blood vessels. A slight hematoma, or simply a bruise, quickly resolves on its own. White spots can also appear on the nail plate from trauma. These spots are a kind of wounds and signal that dystrophy processes are occurring in the body due to lack of calcium.
If the nail is swollen, the area around it is red and very painful, medical attention is needed. You will also need the help of a doctor if, after an injury, the nail begins to peel or purulent discharge is observed from under the nail plate. If the peeling is complete, the nail will need to be removed.
Nail dystrophy, which occurs when it is injured, provokes the development of dyschromia. The nail radically changes its color, becoming almost black. Dystrophy causes a feeling of rejection of the nail; it begins to gradually atrophy.
Injury to the nail plate and subsequent dystrophy can also manifest itself in excessive flexibility of the nail. Lump-shaped growths often form on the damaged area of the nail plate.
As often happens, at the first symptoms of some disease, most people are in no hurry to seek help from a doctor. And it’s in vain, because every painful symptom can become a harbinger of some serious disease. In the same way, with diseases of the toenails, you must adhere to the rule that at the first incomprehensible symptoms you need to consult a doctor.
Many girls and men will agree that shoes are not always comfortable, so, one way or another, their feet may experience pain. Such symptoms should not be underestimated, as they may continue to spread. Everyone knows such a nail disease as fungus. What can we say about toenails, if it can be difficult to cure this disease on your hands! Feet are always in socks and shoes, and it can be difficult to cure nails in such conditions.
It is also worth noting that not every person, experiencing discomfort or pain, thinks that this may be a symptom of a serious illness. And this is precisely why most cases of nail disease develop further and are not treated at the initial stages.
Doctors consider nails to be a separate human organ, because they directly show the state of the body and whether a person is healthy. So, toenails, just like on the hands, show what a person eats, drinks and what vitamins are missing in the body. If a person's health is in good condition, the toenails will be smooth, regular in shape, and without bulges. Otherwise, nails may become brittle and change color. And if they are attacked by some kind of disease, they can completely deteriorate.
It is worth understanding that nails are not only the nail plate, but also all nearby skin coverings. For example, the ridges and cuticle are also part of the nail, and they need the same care as the nail. This applies to both fingernails and toenails. Due to the fact that there are special ridges near the nails, and a matrix directly under the nail, the nail plate develops in a healthy manner. If one of these skin coverings is damaged, the nail will not grow properly.
When carrying out a manicure procedure, the main thing is not to damage the cuticle, or rather its base. Thanks to the cuticle, access to the base of the nail is blocked, this protects it from the influence of the external environment and from harmful substances. If a girl, while doing a trimmed manicure, damages the cuticle, then the base of the nail is damaged and it begins to grow poorly, or its structure deteriorates. It should also be remembered that it is better to begin treatment of the nail or periungual area immediately after the detection of unpleasant symptoms, because this way it will be faster and more successful.
If you look at a photo of those diseases that can damage the toenail, you can be horrified, because even looking at the photo, you can feel the pain that people with such a disease experience.
There are many types of nail diseases, the most common are claw nails, ingrown toenails, nail fungus, and nail trauma.
The first disease is caused by deformation of the joints of the middle phalanx of the finger. If the phalanx bends, it can lead to the formation of toenails. The sooner this predisposition is identified, the faster the treatment process will take place. In order to determine whether there is a predisposition, it is necessary to undergo a diagnosis and consultation with a doctor.
The second disease, ingrown toenails, can occur due to improper nail trimming. Sometimes this disease can be congenital, but this is rare. The disease is that the nail affects the skin and grows into it, causing pain to the person and causing unpleasant odors. The most important thing that can prevent the appearance of an ingrown toenail is proper trimming - the nail should be trimmed evenly, without sharp corners. At the first symptoms of an ingrown toenail, you need to go to the hospital, otherwise you may wait until surgery.
The third disease is nail fungus. The disease often appears in those who wear uncomfortable, tight shoes. The fungus develops in a confined space and affects the nail plate until it is completely destroyed. The most common symptom of fungus is yellowing and thickening of the nail. As soon as these symptoms are detected, you need to resort to drug treatment.
The last disease is injury to the nail plate. It is observed very often in people who work with heavy tools. When something falls on the nail or is hit hard, it begins to turn blue, which means that there is bleeding under the nail. Usually, in order to remove a hematoma, the nail is punctured, the blood goes away, and the nail grows normally. But many people do not pay attention to the blue discoloration, and a hematoma can develop. Therefore, if the nail hurts and the leg swells, you should immediately go to the hospital. In other cases, if there is a small spot of blood under the nail, you can figure it out yourself, following the doctor's instructions.
A detailed description of each disease can be found on websites dedicated to nail care. There will also be tips on how to avoid toenail diseases.
Structure of nails
Nails are derivatives of the skin, which in the process of evolution have turned into a dense material that protects the nerve endings of the hands and feet. The hard and at the same time flexible plate provides not only protection, but also sensitivity to the fingertips. A healthy nail consists of:
- cuticles;
- nail root (it is hidden under the skin at the back of the nail);
- holes;
- nail plate (nail body);
- free edge.
The nail is hard due to the fact that it contains a protein called keratin.
From birth, the nail matrix (the main part of the nail growth zone) contains the main characteristics of the nail: its color, density, length and thickness. Modern cosmetology, thanks to an integrated approach, has learned to correct these features of the human body. So, even if you have thin and brittle nails, it is possible to strengthen them and saturate them with nutrients.
The condition of the nail is influenced by many factors:
- genetic characteristics of the organism;
- nutrition;
- general health;
- environmental influences;
- mechanical damage;
- fungi and so on.
With the development of cosmetology, caring for nails has become much easier, because it does not take much time and does not require special expenses. You can always contact a specialist who will make your nails beautiful. But sometimes complications arise after a manicure:
- inflammation;
- cracks;
- detachment of the nail plate.
Video: nail structure
Why do nails darken?
The main cause of blackening of the nail is hemorrhage due to injury:
- bruise,
- pinching,
- constant compression of tissues when wearing narrow shoes.
If the hematoma is minor, you can treat the nail at home. As the nail grows, the blackness spontaneously disappears.
Other dangerous causes of partial (dots, spots, stripes) or complete blackening, bluing of nails:
- bacterial infections,
- fungal diseases,
- frostbite,
- avitaminosis,
- obstructive changes in the lungs,
- liver diseases,
- renal failure,
- oncology (melanoma),
- hemangioma (benign tumor),
- diabetes,
- gastrointestinal diseases,
- intoxication with heavy metals and drugs.
Household external factors that are not hazardous to health for changing the color of nails are stains from tobacco, varnish, and all kinds of dyes used at work and at home.
If the color of nails suddenly changes to black, blue, or brown in the absence of a traumatic factor, it is important to promptly determine the exact cause, since pigmentation may indicate extensive internal damage to the body.
What happens during an injury:
- hemorrhage occurs in the soft tissues, which puts strong pressure on the area of the nail plate.
- The person experiences severe bursting pain.
- The hematoma from the accumulation of blood begins to increase, lifting and tearing the nail away from the skin of the bed.
- There is an urgent need to stop the development of extensive bleeding and relieve the person of pain.
- Prevent finger infection.
How to do this correctly?
To stop the development of a hematoma and prevent the formation of an inflammatory process, you need to perform the following steps: Urgently place your finger under a stream of cold water, or apply ice wrapped in a sterile cloth (15 minutes). Cooling procedures promote the resorption of the hematoma and partially relieve pain.
Disinfect the injured nail with antiseptics (alcohol, hydrogen peroxide 3%, Miramistin, or Dioxidin).
Raise your finger (or toe) up to ensure blood flow.
To reduce swelling of the skin, an iodine mesh is used (on intact skin).
The area of the bruised nail needs to be protected from infection - tied with a sterile napkin (bandage). If the plate is torn off, you need to apply a bactericidal patch or bandage it with a dressing with ointment (antibiotic).
If the pain is severe, you can take Nise, Ibuprofen, or another pain reliever.
What you should absolutely not do
Some procedures may worsen the condition:
- It is unacceptable to immediately warm up the injured limb,
- It is forbidden to tightly bandage the injury site,
- if the nail is torn off, do not lubricate the wound with iodine,
- In case of severe pain, you should not self-medicate.
If a child’s nail turns black, it is imperative to see a doctor, regardless of the extent of the damage.
An adult should call an ambulance under the following circumstances of a blackened nail from a bruise:
- continuous bleeding
- deep wound,
- fracture of the finger bone,
- severe pain,
- tearing of the nail plate,
- contamination of the wound with soil,
- the finger dangles or does not bend.
It is imperative to get a tetanus vaccination if more than 5 years have passed since vaccination. Do not delay a visit to the doctor even if the nail is slightly blackened in cases of an inflammatory process: redness of the skin of the nail folds, the appearance of purulent discharge, increased swelling of the finger.
Treatment of nail psoriasis at home
The healing process of soft tissues and nail plates damaged by bruises or pinching is delayed for a long time: the growth of a new healthy nail occurs in six months, or even a year. Throughout this period, it is necessary to protect the wound surface of the epithelium from the penetration of various types of infectious agents:
- pathogenic bacteria,
- viruses,
- fungi,
- protozoa.
Anesthesia
The doctor will determine which medications are necessary for an individual patient; here is a list of the most popular medications for the treatment of black nails:
- Compresses to reduce pain are made using an aqueous solution of Dimexide (2 times a day for 30 minutes), Novocain.
- They use anti-inflammatory painkillers: Analgin, Ibuprofen, Nise, Ketanov.
- Diclofenac, Ibuprofen, and Troxevasin ointments have anesthetic properties.
Anti-inflammatory and regenerating agents
- Relieve swelling and promote resorption of hematomas: Heparin ointment, Riciniol, Troxevasin. Herbal ointments Bodyaga Forte, Comfrey, Calendula.
- Cooling ointments with Menthol and Arnica are used to prevent the formation of hematoma and swelling immediately after a bruise.
- To activate tissue restoration, spray (or gel) Panthenol, Bepanten, Solcoseryl are used.
- When tissue inflammation occurs, doctors recommend lubricating the finger with Levomekol ointment and Ketonal cream.
We invite you to familiarize yourself with what red moles on the human body mean: causes of appearance, treatment, photos
If it is not possible to visit the surgeon’s office, the following safety measures should be taken:
- carefully trim off the plates extending from the nail bed,
- protect the wound with a bandage,
- disinfect the surface of injured tissues two to three times a day,
- lubricate with anti-inflammatory ointments.
Gradually the nail will come off spontaneously.
Forced removal will be required if the finger becomes infected and an inflammatory process begins.
In field conditions, crushed leaves of plantain, coltsfoot, and burdock, thoroughly washed in a clean spring or boiled water, can be applied to the site of the bruise (if there is no open wound).
2. To prevent infection, use decoctions of medicinal herbs that have antibacterial and anti-inflammatory properties: chamomile, calendula, willow bark.3. Nettle leaves and the white pulp of the puffball mushroom have remarkable hemostatic and disinfecting properties.4. One of the best folk remedies for treating black nails is honey with propolis.5.
- Changes in the pigmentation of the nail plates and skin may indicate damage by fungal microorganisms.
- A dermatologist determines the etiology of the disease, then prescribes the following drugs for treatment:
1. Antimycotic gels and varnishes: Lotseril, Demikten, Aventis, Mikozan, Oflomin, others. All of them have antiseptic as well as fungicidal properties.2. To safely remove the black nail plate, Nogtevit, Nogtemycin, Onychoplast patches are used.3. Effective ointments and creams for treating fungus: Lamisil, Kertonazole, Exoderil, Mycospor, Sertaconazole provide relief from fungal infection within a month to a month and a half from the start of treatment.
In order to reduce the spread of fungal spores, destroy pathogenic microorganisms and restore black nails in children, it is advisable to use the natural oil preparation Stop Active.
For internal use, systemic antifungal drugs are prescribed: Lamisil, Nizoral, Diflucan, Griseofulvin, and others.
All listed medicinal products should be used only as prescribed by a doctor.
In case of sudden blackening of nails in the absence of a traumatic factor or fungal infection, it is important to promptly determine the exact cause, since such symptoms may indicate the formation of malignant melanoma, the development of lung, liver, and kidney disease.
For consultation, you need to contact a therapist; if necessary, the doctor will make an appointment with a specialist.
You should not self-medicate, since incorrect use of medications can cause severe allergies, blood poisoning, and progression of malignant tumors.
| If there is a large accumulation of blood, detachment of the nail plate, damage to the skin, or acute pain, you should immediately contact the emergency room to exclude a fracture of the finger and proper antibacterial treatment. |