The size of the pelvis plays a very important role during pregnancy. Sometimes the course of labor depends on the pelvis: if it is narrow, then the birth can be complicated or end in a caesarean section. A narrow pelvis occurs in 2-3% of pregnant women, but it is not always an indicator for artificial delivery.
Gynecologists pay great attention to a woman’s pelvis even during registration. Be sure to have it measured and already in the first days of pregnancy you can predict how the birth will proceed. So what are its features? And what to expect if the pelvis turns out to be narrow? Let's try to find answers to these and other questions.
Pelvic dimensions: norm and deviations
Every woman knows very well what a pelvis is. It is conventionally divided into large and small. It is in the large pelvis, towards the end of pregnancy, that the uterus and fetus are accommodated. And if for some reason its wings are not straightened, then the uterus will move forward, as a result the tummy will “stick out” (become pointed). The small pelvis is a kind of birth canal through which the baby will move at birth. It is clear that if the pelvis turns out to be narrow, then the child will have a hard time “making his way” into the light.
How is the pelvis measured? Surely, if this has already been done to you, then you noticed an incomprehensible set of numbers on your card. If they look like this: 26-29-31-21, then there is nothing to worry about: your pelvis is normal. If any of the indicators is 2 numbers less, then you will be diagnosed with a narrow pelvis. What do these numbers represent? Regular sizes. For example, the interosseous size (the distance between the upper corners of the protruding bones) should be from 25 to 26 cm and so on. All measurements are carried out using a tazometer and a centimeter tape. By measuring the large pelvis from the outside, you can guess what the small pelvis will be like. The size of the latter can be determined by vaginal examination, and you may also be prescribed radiography and ultrasound to determine the size of the pelvis. Also, other factors indicate the narrowness of the small pelvis: hand length is less than 16 cm, shoe size is less than 36, height is less than 160 cm. When measuring the pelvis, it is imperative to take into account the massiveness of the pelvic bones, using the Solovyov index, i.e. measure the circumference of your wrist and if the size becomes more than 14 cm, then your bones are massive, which means your pelvis will be narrow even with normal values.
However, in reality everything is not so simple. A narrow pelvis has its own varieties and characteristics. Both the course of pregnancy and delivery depend on this.
Diagnostics
Many business and most active mothers try to find out on their own how to determine whether the pelvis is narrow for childbirth, and whether they can give birth themselves at certain sizes. In fact, this cannot be done either at home or “by eye”. Diagnosis is possible only in a hospital; it is carried out exclusively by a professional doctor using a specific obstetric instrument called a pelvisometer. With its help, the following dimensions are determined:
- the interspinous distance is measured between the anterior iliac (connecting the pelvis to the spine) spines (processes), normally it should be more than 25 cm;
- the gap between the most distant points of the iliac bones is normally more than 28 cm;
- the distance between the trochanters (greater) of the femurs, the desired norm is more than 30 cm;
- the true conjugate is measured during a vaginal examination, this is the distance between the pubic joint and the highest point (promontory) of the sacrum; it is considered normal when the obstetrician cannot reach this point;
- external conjugate - the gap between the suprasacral fossa, which is located in the lumbosacral region, and the upper corner of the pubic symphysis, a certain norm - more than 20 cm;
- Michaelis's diamond above the coccyx, in the area of the sacrum, the boundaries of which are normally clearly visible, all sides are symmetrical: transverse are 10 cm, vertical - 11 cm;
- The Solovyov index allows you to evaluate the thickness of the bones, which can also interfere with normal childbirth - this is the circumference of the wrist, the maximum norm is no more than 14 cm.
To clarify the parameters, in rare cases, radiography is performed, but it can harm the fetus. An ultrasound examination can also help assess the size of the narrow pelvis during pregnancy. In clinical cases where this data cannot be obtained in advance, obstetricians are guided by specific signs and symptoms.
Through the pages of history. S. A. Michaelis is a German gynecologist of the 19th century, whose name is the famous sacral rhombus, which determines whether a woman can give birth on her own or not.
Anatomically narrow pelvis
This is called a basin in which the main dimensions are smaller by 1.5-2 cm. This can be reduced by several sizes, or just one. Depending on this, a generally uniformly narrowed, transversely narrowed, simple flat and flat rachitic pelvis is distinguished. In order to confirm the diagnosis of an anatomically narrow pelvis, additional research methods are used. This may be a computed tomographic pelvimetry method or an x-ray method. Thanks to them, it is possible to determine the degree of narrowing of the pelvis. Depending on this, an anatomically narrow pelvis of 4 degrees is distinguished. The first is the most common, and fortunately, it is the easiest, considering its effect on the outcome of pregnancy and childbirth.
More on the topic
When do the pelvic bones begin to separate during pregnancy?
When do the pelvic bones come together after childbirth?
What to do if you have a small belly during pregnancy and it doesn’t grow?
Large fetus during pregnancy
What complications may occur during childbirth?
Unfortunately, it is very difficult to prevent an anatomically narrow pelvis, because many factors influence the formation of the female pelvis. Most often, the causes arise in early childhood. These may be frequent infectious diseases, poor nutrition, lack of vitamins, hormonal disorders during puberty. Bone damage due to rickets, poliomyelitis, and tuberculosis leads to pelvic deformation. There are also congenital anomalies of the pelvis, spinal deformities, pathology in the hip joints, injuries and fractures of the pelvis.
How often does this type of presentation occur?
Such an arrangement of the fetus occurs in 5 cases out of 100, while:
- in 63-75% of cases the buttocks are presented, the lower limbs are extended upward and along the body;
- in 20-24%, the child sits “Turkish”: both the buttocks and legs are facing down, bent at the knees and hip joints;
- in 11-13% the child “stands” on one or two legs;
- in 0.3% of cases the baby is on his knees.
The obstetrician's decision depends on the type of pathology - whether a woman can give birth herself with a breech presentation, or whether a caesarean section should be performed.
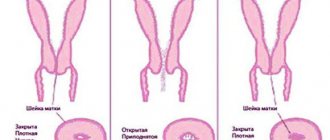
Clinically narrow pelvis
Unlike an anatomically narrow pelvis, which is determined already at the beginning of pregnancy, with a clinically narrow pelvis the situation is different. It can only be diagnosed during childbirth, even if the anatomically narrow pelvis was “absent” throughout the entire pregnancy. Clinically, a narrow pelvis does not depend on the size of the pelvis; it is determined by a discrepancy between the fetal head and the mother’s pelvis.
The causes of its occurrence are most often associated with the course of labor. In the first place are a large fetus and post-term pregnancy, as a result of which the bones of the fetal skull become too dense and they are unable to configure themselves. Clinically, a narrow pelvis is also diagnosed with anomalies of labor, improper insertion of the head, with tumors of the uterus, as well as if there are congenital malformations of the fetus. In other words, you will hear about the diagnosis “Clinically narrow pelvis” only during childbirth, or even after it.
What explains the doctors' desire to perform a caesarean section?
Before being born, the baby must pass through the bony canal of the mother's pelvis, which is wide at first and then narrows. To do this, he makes several turns, standing each time so that the part of the body that goes first (the presenting part, in our case these are the legs or buttocks) coincides in diameter with the surrounding bone ring.
This rule applies to the head, which has a certain shape and is formed in such a way that the distances between the forehead and the back of the head, temples, as well as diagonal lines are almost identical to the distances between the maternal bones.
The buttocks and legs are very small, they move along the birth canal quite quickly, and the head does not always have time to adjust (turn to the other side, “bring” the fontanelles together) to the changing sizes of the bone ring.
The small diameter of the presenting part also plays the following role:
- childbirth with this pathology occurs earlier (before 34 gestational weeks);
- they begin with the fact that prematurely, when the cervix is not yet ready for this, amniotic fluid flows out (the head, due to its size, is able to create negative pressure near the presenting part of the fetal bladder);
- the outpouring of water stimulates labor, while the cervix does not experience the necessary pressure and does not open properly;
- a long time passes between the opening of the amniotic sac and the onset of normal labor, which can result in infection;
- breech birth of boys is dangerous: strong pressure arises between the legs and the mother’s soft tissue, acting on the organs of the scrotum and causing them to be compressed. As a result of ischemia, death of the spermatogenic epithelium of the testicles may occur, which threatens infertility. In addition, during childbirth, stimulation of the scrotum may occur, causing the baby to inhale while immersed in an aquatic environment (most often there are already particles of original feces - meconium, due to hypoxia during such births). This allows fluid to enter the respiratory tract, causing breathing problems (aspiration pneumonia), requiring a long stay in the neonatal intensive care unit;
- passing through the birth canal, the head often presses the umbilical cord against the walls of the pelvis, which leads to acute hypoxia or even asphyxia;
- since the cervix does not always have time to fully open (or it may spasm) by the time the fetal head reaches there, it can compress the head, causing fatal asphyxia of the fetus;
- passing through the birth canal, almost at the very exit from the pelvis, the baby’s head can hyperextend, causing complications in the brain (for example, hemorrhage in the cerebellum, subdural hematoma), which threatens death or disability;
- weak stimulation of the birth canal threatens weakness or discoordination of labor (when parts of the uterus contract not harmoniously, but separately), which is bad both for the child (fetal hypoxia increases and can become critical) and for the mother (the birth canal becomes infected). At the same time, it is impossible to stimulate uterine contractions with oxytocin - the blood supply to the fetal tissue may suffer even more;
- during childbirth, the baby’s arms may tilt back, which leads to injury;
- the mother's birth canal is injured: from minor ruptures of the perineum to injuries to the cervix, damage to the pelvic bones, which provokes postpartum bleeding and serves as a source of purulent-septic complications of the reproductive organs;
- children who survived hypoxia and asphyxia have problems with the nervous system: epilepsy, paresis, hydrocephalus, developmental delays.
Therefore, delivery with breech presentation is often carried out surgically, especially if ultrasound predicts the child’s weight to be more than 4 kg or less than 2800 grams.
Narrow pelvis and pregnancy
A narrow pelvis has virtually no effect on the course of pregnancy. It’s just that during this period, if we are talking about an anatomically narrow pelvis, you should be under the supervision of your attending physician. And it is natural to prepare in advance for the upcoming birth, and it may occur with some peculiarities. In the last trimester, a pregnancy with a “narrow pelvis” can be complicated by incorrect position of the fetus. Due to the fact that the baby's head is not pressed against the entrance to the pelvis when it is too narrow, the expectant mother often experiences shortness of breath.
But even if your pelvis turns out to be “normal,” you shouldn’t relax. You have read the information about a clinically narrow pelvis. In this case, much depends on the expectant mother herself. For example, food. After all, excess weight can be detrimental to your pelvis and baby. In any case, the nutrition of a pregnant woman should be rational. Doctors also advise every pregnant woman to work on the elasticity of the perineal muscles. For this you may need Kegel exercises and... regular sex.
Pregnancy management
The diagnosis of breech presentation is first made at 21-24 weeks upon examination by an obstetrician at the antenatal clinic, but is finally established by an ultrasound picture. Until 32-33 weeks, as long as there is room in the uterus, there is a chance that the fetus will change its position. From 21 to 32 weeks, if there are no contraindications, a woman is recommended to perform special gymnastics:
- I.p. lie on the floor, on your back. Turn on your left side and lie there for 10 minutes. Then do the same on the right side. Repeat 3-4 times in 1 approach. Perform 3 approaches per day.
- Stand in a knee-elbow position so that your pelvis is higher than your head, stay like this for 15 minutes.
- Lie on your back with a folded blanket or pillow under your pelvis. You need to lie like this for about 15 minutes.
You can perform gymnastics developed by Dikan, Shuleshova or Abramchenko. After consulting with your obstetrician, perform exercises in the pool under the guidance of a trainer (water aerobics). In this case, you need to take No-shpa or Riabal in the recommended dose for up to 5 days.
If the next ultrasound shows that the fetus has turned over, you will need to wear a special corrective bandage. If this does not happen, the doctor leading the pregnancy will advise you to go to the hospital at 33-34 weeks with a specialist who knows the technique of external fetal rotation (this manipulation is performed under ultrasound control and can provoke premature birth). There are contraindications for external rotation.
If it was not possible to turn the fetus into the occipital position, or due to contraindications this manipulation was not performed, and the pregnancy proceeds without gestosis or other complications, the woman is scheduled to be hospitalized at 38 weeks. In case of pathological pregnancy, hospitalization is carried out at the 36th gestational week.
You need to pay attention to the warning signs of labor:
- “lumbago” appears in the pubic area;
- appetite worsens;
- more often you want to go to the toilet in a small way;
- “training” contractions appear once or more often (those who are having their first birth will only have to learn about this sensation): uterine contractions, the intensity and duration of which do not increase over time, they can be relieved with the “No-shpy” tablet;
- the mucus plug comes off.
When warning signs appear, especially training contractions and mucus discharge, a woman whose pregnancy is complicated by this pathology should be urgently hospitalized. Also, a pregnant woman should know how labor begins with a breech presentation.
This is the rupture of amniotic fluid: wetness of a pad or underwear, which does not necessarily immediately be strong (water can leak through a small hole in the amniotic sac). Full-fledged contractions during breech presentation rarely develop immediately after the rupture of water, so if you suspect this symptom, you should go to the hospital.