Signs of the disease
Pathological inflammation in boys usually begins suddenly, with discomfort in the penis, sharp pain or. Significant redness and pronounced swelling of the head of the penis and the inner side of the foreskin are detected, observed in large quantities (smegma), which have a characteristic odor. With further progression of the disease in children, it is even possible for the formation of erosive areas and peeling of the skin.
Babies become very irritable and cry often.
There are also general signs of the onset of illness:
- decreased appetite;
- restless sleep;
- low-grade body temperature;
- inguinal lymph nodes enlarge;
- enuresis may occur.
In the absence of adequate timely therapy, balanoposthitis becomes chronic. This can provoke the formation of scar changes on the foreskin with the development of conditions such as phimosis and paraphimosis, as well as noticeable deformation of the head of the penis.
When you need medical help
There are several situations in which parents should seek qualified medical help as soon as possible:
- Paraphimosis;
- Balanoposthitis;
- Adhesions between the foreskin and the head of the penis.
- Paraphimosis can occur when parents, contrary to common sense, decide to personally stretch the foreskin due to physiological phimosis. At some point, everything went wrong: the head came out, but found itself pinched by the foreskin from below, and there was no way to get it back. If this happens, you need to take the child to the surgeon as soon as possible, minutes count. Otherwise, the head, pinched by a ring of narrowed flesh and deprived of normal blood supply, is at risk of developing gangrene, which, in turn, risks amputation of an organ so important for a man’s future.
The sooner the child is taken to any nearest medical facility, the better. If treated in a timely manner, the doctor can get by with manually moving the head of the penis into place. Under no circumstances should you try to do this at home yourself! But what you need is to immediately slightly squeeze the head of the penis and apply something cold to it, but do not allow frostbite.
In some cases, this is even enough to relieve swelling and return the foreskin to its place. But you shouldn’t count on this and hesitate to see a doctor.
- Balanoposthitis and other inflammatory diseases of the penis should also not be treated at home with folk recipes. A child who, due to physiological phimosis, has pain when urinating (he cries before peeing), has reddened and swollen foreskin, must be shown to a pediatric surgeon. These diseases occur more often in children than in adult men, which in itself is dictated by physiological age-related narrowing.
Types of pathology
There are 3 variants of the disease: acute (lasting less than 3 months), chronic (disturbing for more than 3 months), specific.
- Acute balanoposthitis.
Acute balanoposthitis in boys is characterized by:
- pain when urinating and when touching the genitals;
- severe swelling of the foreskin;
- cyanosis of the head of the penis;
- low-grade fever;
- refusal to eat;
- irritability.
Often the pathology begins after a viral illness, when wearing tight underwear that rubs the head, or failure to comply with hygienic requirements for child care.
Inflammation of the penis, occurring in acute form, is divided into:
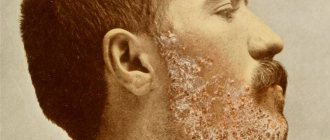
- purulent balanoposthitis - the symptoms are pronounced, there is a temperature and purulent discharge with an unpleasant odor, as well as hyperemia, swelling of the exposed area of the head, severe burning and itching. In case of chronic inflammation, the foreskin has to be removed;
- simple - signs of changes are moderate, mucous discharge, temperature is not elevated, general condition is satisfactory;
- erosive - the appearance of small erosions on the inflamed areas of the penis is noted;
- necrotic - necrosis of the foreskin of the head of the penis due to the progression of pathology.
- Chronic balanoposthitis.
Long-term inflammation has certain manifestations:
- exacerbations of the disease alternate with short periods of easing symptoms;
- itching, discomfort, hyperemia of damaged areas;
- cracks that do not heal for a long time;
- compaction, thickening of the foreskin;
- regular, unpleasant-smelling discharge from the penis.
Symptoms significantly affect the usual way of life, causing serious damage to health.
- Specific balanoposthitis.
This is the name given to inflammation provoked by certain microorganisms. Various pathogens can become infectious agents:
- syphilis;
- tuberculosis bacillus;
- chlamydia;
- gonococci;
- herpes.
Specific pathologies in children are rarely observed. Most often in utero or during childbirth from an infected mother.
Possible complications
DVR with four surveillance cameras and warning system Replica Galaxy S10 Plus for only 7990 rubles! Mirror-computer in an ultra-thin case + rear view camera using Japanese technology
Recommended reading: Until what age does manhood grow?
When pathology develops, surgery is usually prescribed to remove scars. Phimosis is a narrowing of the foreskin that prevents the head from being removed. As the child develops, the head of the penis gradually moves apart the tissues and the physiological fusion is destroyed.
In adolescents, the sex hormones of the male body begin to actively operate. They make the foreskin mobile. When it begins to stretch well, the head of the penis opens completely. This natural process should not be interfered with prematurely.
To prevent the development of pathology, it is necessary to monitor the condition of the penis during the boy’s daily bathing. Also, the mother should monitor how the child urinates. Does urination cause him difficulty? Swelling of the organ, redness, and difficulty in passing urine are reasons to consult a doctor.
The development of pathology can begin to be judged starting from the age of seven. Phimosis can be hypertrophic and atrophic. During the pathological process, the skin of the penis becomes thinner and is subject to various microtraumas. As a result, scars form on the foreskin. The prepuce protrudes beyond the head of the genital organ.
There are four degrees of pathology:
- With the first, the head in a calm state is exposed quite easily;
- in the second and third stages of the disease, the head does not open completely;
- in the fourth stage of phimosis, the organ sac swells before urination, and only after that urine begins to be released in a very thin stream or droplets.
Phimosis also has a genetic predisposition. Also, the development of pathology can be affected by the resulting organ injury and the inflammatory process. All these negative factors negatively affect the condition of the foreskin. Tissue that is unable to stretch causes phimosis to progress.
When the head opens completely in boys, a specialist will tell you. During the examination, the doctor will identify the presence of complications. The most dangerous of them is the pinching of the head of the penis by the narrowed tissue. Pathology leads to impaired urine outflow and infectious processes in the urethra.
Inflammation of the organ flesh is called balanoposthitis. It is this disease that develops when regular hygiene standards are not observed. Tissue infection occurs. Children with reduced immunity are especially susceptible to infections. As a result of the inflammatory process, scars form on the foreskin. Balanoposthitis requires urgent medical intervention. Urinary retention requires immediately showing the child to a doctor.
Often fusion of the foreskin and glans occurs. In the initial period, small areas grow together, then they become larger. Any attempt to open the head of the penis in such a state is accompanied by severe discomfort, intense pain and bleeding.
Etiological factors
The most common cause of balanoposthitis in boys is considered to be a lack of necessary hygiene of the penis, which leads to the accumulation of cheesy discharge under the foreskin.
IMPORTANT!
Doctor of Medical Sciences, Professor Sergei Mikhailovich Bubnovsky tells how to save yourself and forget about venereal diseases.
Read the interview >>
Often pathological inflammation begins as a result of a parental attempt to help expose the foreskin. This is how infections enter the preputial sac from the external environment.
Physiological phimosis in children 3-5 years old is considered one of the factors in the development of balanoposthitis. It makes proper hygienic care difficult due to the impossibility of exposing the head when retracting the foreskin.
Other factors that provoke balanoposthitis include:
- infrequent diaper changes for infants or inappropriate size;
- wearing tight underpants that rub the skin of the penis for children 1.5-2 years old;
- allergies (to powder, diaper rash cream);
- deficiency of certain vitamins;
- diabetes.
Conservative drug treatment
Treatment of phimosis in boys without surgery can be of 2 types:
- medicinal;
- non-medicinal.
Glucocorticosteroid drugs are used as medications, usually in the form of ointments. Most often this is betamethasone or clobetasol. These medicines:
- help increase the elasticity of the foreskin tissue;
- heal microcracks;
- prevent inflammatory processes.
Non-drug treatment of phimosis
Non-drug therapy for phimosis in boys is most often used. Without surgery, treatment is based on regular massage. Dr. Komarovsky advises carrying out the procedure daily, preferably after a bath or shower, when the skin is more elastic. The set of exercises includes:
- Pull the foreskin over the head of the penis until the first pain is felt. Repeat 10-15 times.
- Insertion of two fingers into the preputial sac.
- Expansion of the flesh until the first manifestations of pain. Repeat 5-6 times.
This complex treats phimosis in boys, according to Komarovsky, in 2-3 months. You just need to do the exercises at least 2 times a day. It is also recommended to supplement the massage with a bath of a weak solution of potassium permanganate, known for its antiseptic effect, once a day. You need to dilute potassium permanganate with warm water until it turns slightly pink. A solution that is too concentrated can cause burns to the mucous membrane.
Therapy technique
If the disease is the result of insufficient hygiene, then it is necessary to take baths in a sitting position with antiseptics (potassium permanganate, furatsilin) or infusions, decoctions of astringent herbs (chamomile, oak bark, green tea, St. John's wort, calendula, plantain).
First you need to carefully pull back the foreskin and remove accumulated secretions. You can wipe the affected areas with solutions of Chlorhexidine and Miramistin. Effectively relieves inflammation of the foreskin in a child by applying antibacterial ointment (Sintomycin, Levomekol) to the affected areas. If it is impossible to treat the penis yourself, a specialist will open the head of the penis and remove smegma. Usually, 2-3 days are enough to successfully relieve symptoms. In between baths, at night, the penis can be wrapped in a gauze bandage soaked in the drug.
A pathology such as balanoposthitis in a child is often diagnosed. Balanitis is an inflammation of the skin in the area of the glans penis, and posthitis is an inflammation of the foreskin. Balanitis and posthitis separately are rare. Combined inflammation develops most often. This is a purely male disease. In the absence of proper assistance, a child may develop a complication such as phimosis. What are the etiology, symptoms and treatment of this disease?
Balanoposthitis in children is quite common. The prevalence of this pathology among boys is 6%. Children under 5 years of age are most susceptible to the disease. There are acute and chronic balanoposthitis.
In the absence of therapeutic measures, the acute form of inflammation becomes chronic. There are several types of balanoposthitis in children, depending on the main etiological factor. The primary form of the disease is most often caused by local irritating factors.
The secondary form develops against the background of another pathology. Inflammation of the skin of the head and foreskin is possible with Queyra's erythroplasia, Zun's balanitis, and Reiter's disease. Very rarely, xerotic obliterating balanoposthitis is detected in children. Purulent balanoposthitis is the most severe.
Hypertrophic phimosis
This form of the disease develops mainly in children, adolescents and adults who are overweight. Due to excessive accumulation of adipose tissue, the foreskin increases in size, which leads to the development of the disease hypertrophic phimosis in adolescents. Due to the large amount of moisture that the tissue retains, an infection begins to develop, which leads to balanoposthitis. In addition, this form of phimosis can provoke a number of complexes based on the excessive length of the foreskin.
In the case of cicatricial phimosis, in addition to the excess foreskin, scars and cracks form on it. Cicatricial phimosis - a photo will illustrate this disease. Cicatricial phimosis in adults is mainly observed due to poor hygiene or the presence of various diseases where phimosis is a symptom.
Stages of phimosis
There are only 4 degrees of phimosis:
- Phimosis 1st degree - in a calm state the head is exposed without difficulty, but during an erection difficulties arise with exposing the head;
- Phimosis 2nd degree - difficult exposure of the head at rest, exposure is impossible during excitement;
- Phimosis 3rd degree - the head of the penis is not exposed at all, but so far there are no problems with urination;
- Phimosis 4 degrees - the head of the penis is not exposed, and when urinating, liquid accumulates in the foreskin sac and flows out drop by drop.
Most complaints from patients are aimed at painful sensations during urination and during erection, as well as the inability to properly care for the intimate area and the constant accumulation of smegma. Physiological phimosis (photo) – the picture shows 2 stages of phimosis development – the first and the last.
Signs of phimosis
As such, the reasons for the narrowing of the foreskin have not yet been established, but according to studies it has been proven that this behavior of the disease is characterized by a lack of connective tissue in the body. A genetic predisposition to phimosis has also been established.
The disease phimosis can either be preserved from childhood, when the foreskin never moved away from the head, or it can form during puberty. During puberty, insufficient development of the foreskin may occur when the head is fully formed. In such a situation, the head either opens very hard at rest or does not open at all. Phimosis is also observed in adults.
If the disease is started, phimosis in men can develop into balanitis (balanoposthitis) - a disease characterized by inflammatory processes of the head and foreskin when an infection gets inside this “bag”. Or balanitis can cause phimosis. The latter is much more common. Since balanitis is an infectious disease that occurs mainly due to non-compliance with the rules of hygiene of the intimate area, as a result, without the necessary treatment, the flesh narrows, clogging the infection, which leads to phimosis.
Consequences of phimosis
The greatest danger of phimosis is that during an erection the head increases in size and the foreskin is strongly stretched. This leads to the fact that the speed of blood flow to the head gradually weakens, and the flesh becomes covered with small cracks and then scars. Due to scars, the elasticity of the tissue is lost, which leads to the progression of the disease. This especially affects adults who also suffer from inflammation. In this case, phimosis occurs in conjunction with an infectious disease, which can cause physical pain.
Further development of phimosis leads to the fact that the foreskin begins to grow back to the head. This does not in any way affect the general well-being of the patient, but when trying to expose the head, sharp pain and bleeding may occur.
With phimosis, another disease can develop, which is its complication - this is paraphimosis - complete pinching of the head. Phimosis (Paraphimosis) at this stage manifests itself during masturbation or sexual intercourse by pinching the head. In this case, the head loses blood flow and after some time tissue necrosis begins. If you do not consult an andrologist in time, you can wait until the amputation of the penis due to the risk of blood infection from dead tissue.
Dr. Komarovsky “Phimosis in boys” video
Dr. Komarovsky considers phimosis in boys to be a natural phenomenon, if no problems with urination have been noticed. In his opinion, when the child reaches a certain age, then the wall of the foreskin will separate on its own. He also believes that there is no medical evidence at what age one should start turning to specialists for help regarding phimosis. We also bring to your attention “Doctor Komarovsky: phimosis” video on the topic of the article.
Treatment of phimosis
If you have just begun to observe manifestations of phimosis, you should consult a doctor for advice. Below are ways to get rid of phimosis.
Why does the disease develop?
The development of balanoposthitis is caused by various factors. The skin of the genitals, like other areas of the body, needs constant care. The development of the disease is based on non-compliance with personal hygiene rules or irritation of the skin in the penis area, which leads to the activation of bacteria. Balanoposthitis is predominantly an infectious disease. Inflammation is caused by the following factors:
- accumulation of smegma on the penis, which is a breeding ground for microorganisms;
- attempts to expose the head of the foreskin;
- synechiae of the foreskin in a child;
- rare changes of underwear or diapers;
- excessive use of skin care products (creams);
- wearing clothes with residues of washing powder;
- irritation or injury to the skin of the penis with synthetic fabric and seams on underwear.
Most often, the causative agent of the disease is cocci (staphylococci, streptococci). Often the cause is the activation of E. coli, fungi, and the herpes virus. Predisposing factors for the development of balanoposthitis include the presence of endocrine pathology (diabetes mellitus), anemia, lack of vitamins in the body, congenital features of the foreskin, diseases of the genitourinary organs, in which purulent secretion is released from the urethra, as well as hypothermia. In young children, a condition such as physiological phimosis often occurs. As the child grows up, it goes away.
Surgical treatment of phimosis in boys
The radical treatment for phimosis is surgery. It is prescribed only if the child has practically no opportunity to empty the bladder naturally, and also if scarring changes due to inflammation are noticeable on the penis. There are several types of operations that eliminate this problem:
- using a probe and a gauze pad, the adhesions are separated under local anesthesia by making three incisions in the foreskin;
- circumcision (circumcision), if scar changes have severely affected the epithelium;
- Schloffer incision: the foreskin is cut in a zigzag, and then stitched at the sharp corners of the incision - the hole for the exit of the head is enlarged.
The surgical method of treating phimosis provides an almost one hundred percent guarantee of results. But it requires careful adherence to all recommendations of the postoperative period: you will have to use manganese baths, antibacterial gels or creams. In some cases, plastic surgery is necessary to make the penis more aesthetically pleasing after surgery.
Main clinical manifestations
Symptoms of the disease in children are similar to those in adult men. Acute inflammation is characterized by the following symptoms:
- burning sensation in the area of the head of the penis;
- itching;
- pain syndrome;
- impaired urine output;
- redness and swelling of the penis;
- presence of discharge;
- general malaise;
- fever;
- disturbance of night and daytime sleep;
- tearfulness.
Symptoms often include swollen lymph nodes in the groin area. In rare cases, enuresis develops. Symptoms largely depend on the form of inflammation.
With simple catarrhal balanoposthitis, hyperemia and swelling of the head of the penis, moderate itching and burning, and maceration of the skin are observed. In the erosive form, the presence of painful erosions on the skin is visually determined.
The latter are bright red. Some children develop lymphadenitis. With gangrenous inflammation, severe intoxication of the body is observed. Ulcers form on the skin. This form of balanoposthitis is often complicated by phimosis. Healing of ulcerative defects occurs very slowly.
During a medical examination, purulent contents are detected under the foreskin. Smegma has an unpleasant odor. Often the skin of the perineum and scrotum is involved in the process. In this situation, cracks in the skin, exanthema, and diaper rash are detected. The disease begins acutely. In the first week of illness, symptoms increase. Most patients heal on their own. In other cases, special treatment is required.
If the disease becomes chronic, phimosis and paraphimosis, inflammation of the urethra and deformation of the head of the penis may develop.
Types of phimosis
Phimosis is difficulty in removing the head of the penis from the foreskin. The problem is very common in infants. By the age of one, as a rule, the foreskin moves back more easily, and by the age of three, only 10% of boys suffer from this disease. What are the causes of the disease? To begin with, it should be noted that phimosis is of two types:
- physiological (innate);
- pathological (acquired).
Both types can be treated, mostly conservatively. However, in case of complications, it is possible or necessary to solve the problem surgically.
Child examination plan
Before treating balanoposthitis, it is necessary to carefully examine the child. Diagnosis of balanoposthitis is not difficult. The initial examination can be performed by a pediatrician, pediatric surgeon or urologist. In most cases, instrumental research is not performed. Data obtained from interviews with parents and the child himself are of great diagnostic value. The patient needs to donate blood and urine for analysis. With balanoposthitis, the ESR in the blood may increase, and leukocytosis is observed. There is an increased content of leukocytes in the urine and bacteria are present. If necessary, the secretion of the preputial sac is examined. To identify chronic pathology, an ultrasound of the genitourinary organs can be performed.
Age of onset of erection in boys
The child’s genitourinary system begins to form while he is in the womb. In a boy who has not reached puberty, an erection most often becomes the result of external influence. Reasons for erection of the penis include:
- tight underwear or an inappropriately sized diaper;
- bladder fullness (after sleep);
- failure to maintain intimate hygiene;
- tactile contact.
The latter especially applies to children aged 1–2 years. Sometimes parents show their love too emotionally, which is expressed in touching sensitive places (buttocks, legs). A child, having reached a certain age, begins to explore his body. By touching the penis, the baby provokes the transmission of nerve impulses to the brain, which results in an erection.
Friction against tissue leads not only to enlargement of the penis, but also to damage to its mucous membranes. This is fraught with infectious contamination, so you should choose underwear for a boy taking into account physiological characteristics. If the baby is already potty trained (usually by the age of 2–2.5 years) and does not suffer from sleep disorders, he may have an erection in the morning after waking up.
An erection in children that occurs due to similar reasons does not indicate the presence of any pathologies, so parents have no reason to worry. The child's body is constantly being rebuilt. During this period of time, children grow quite quickly, so adults need to be prepared for changes.
A cause for concern is prolonged erection (the penis becomes erect for several hours). This is considered a deviation from the norm, so parents should immediately contact their pediatrician. Violations may occur due to:
- developmental anomalies affecting the organs of the genitourinary system;
- infectious infection of the foreskin;
- inflammatory process that occurs in the testicles, intestines, urinary tract, bladder;
- mechanical damage to the brain and spinal cord;
- helminthic infestations;
- diseases of the cardiovascular system;
- pathologies of the central nervous system that provoke spontaneous activation of the spinal erection center;
- diabetes mellitus;
- oncology;
- intoxication;
- diseases of the rectum.
A characteristic sign of the presence of helminths in a boy’s body is discomfort in the anal area. To get rid of them, the baby unconsciously makes movements that promote contraction and relaxation of the sphincter, and with them the ischiocavernosus muscles. The result is a long-lasting erection.
The father must explain to the teenager the reason for the changes that have occurred.
The first erection provoked by sexual desire occurs at 11–12 years of age. Spontaneous enlargement of the penis is often caused by desire, erotic dreams, watching movies, and nocturnal emissions. They appear due to the production of testosterone, the time of day does not matter. Their disappearance will be facilitated by constant intimate connection or regular self-satisfaction.
Changes in hormonal levels affect the appearance and behavior of a teenager. His voice changes, hair appears in the genital area, armpits, face and chest. According to statistics, most boys first enter into intimate relationships at the age of 13–16. By this time, sperm has already accumulated in the testicles; if contraceptive measures are not followed, a teenager can become a father without even reaching adulthood.
Lack of information regarding discharge after erection, traces of which are detected the next morning, leads to tension and irritation. Often the dreams that triggered ejaculation are forgotten. Misunderstanding gives way to anxiety; teenagers often hesitate to approach their parents with such a question. The boy goes through the last stage of formation of the reproductive system after he reaches 18 years of age.
The mother should not notice the teenager’s awkwardness and try to get him to talk. He is unlikely to talk about this topic with a woman. The result of such a conversation can be a teenager’s feeling of guilt, hostile relationships between family members, and discomfort. A teenager will definitely appreciate the desire of his loved ones to come to terms with the fact that he is growing up.
Puberty is a period that has a great impact on a man’s life. The appearance of an erection and other metamorphoses that occur with the boy at this time should not result in injury. The task of parents is to make it clear that everything that is happening is absolutely normal. The sexual development of the child depends on competent preparation and the quality of the relationship between the teenager and parents. It is advisable that he hear the truth from close people, and not gain experience while being among friends.
Do you have problems with ERECTION? Have you tried a lot of remedies and nothing has helped?
These symptoms are familiar to you firsthand:
- sluggish erection;
- lack of desire;
- sexual dysfunction.
The reasons for erections in adult men are obvious, mainly due to sexual arousal. But few people know why erections occur in boys and adolescents, as evidenced by this phenomenon, as well as ejaculation in boys. To understand the issue, you need to understand what an erection actually is.
So, the male sexual organ - the penis - consists of two cavernous bodies, below them is the corpus spongiosum with the urethra (urethra). At the base of the penis there are muscles attached, which at the moment of contraction block the veins, preventing the outflow of blood from the penis. When the sexual organ is filled with blood, but there is no outflow, it swells and increases in size - this is an erection. Nerves, hormones and mechanical factors are also involved in the process of its occurrence.
Erection in boys
A young mother, seeing a boner on her little son, immediately falls into bewilderment, not understanding why this is happening. Initially, it should be noted that erections in children are purely mechanical. She has no connection with sexual moments or hormones. Most often, the cause of an erection in a baby is the friction of the penis against underwear or a full bladder.
A slight malfunction in the nervous system can also cause the spinal center responsible for erection to spontaneously fire. This is a normal phenomenon and worries about this are inappropriate. But there are also diseases that contribute to excess blood flow to the genital organ. For this reason, contacting a doctor is necessary if the child has an erection very often and the penis is tense for a long time.
Numerous ultrasound examinations of women during pregnancy show that the first erection in boys occurs in the prenatal period. This is due to the development of the nervous and muscular systems. It's no secret that even after birth, the male reproductive system continues to actively improve; a number of inevitable processes occur, during which a boy can have his first erection.
Often, a one-year-old child, studying his body, begins to show an active interest in the genital organ, since touching it causes pleasant sensations even in the smallest men. Observing an erection during such studies, many mothers begin to scold their sons and constantly pull them back
We suggest you familiarize yourself with Burning in the urethra and pain when urinating in the urethra in men, pain when urinating with discharge
There is no need to focus on this. For young children, the penis is an organ just like an arm, leg or ear.
No one scolds a child who studies his ears?
The boy's first erection is hidden and occurs in the mother's womb at 18 weeks. A tense penis can be observed in infants from the first months of life. Some information sources devoted to caring for a baby warn parents against too violent manifestations of feelings in the form of kissing the baby on all the bulges and tickling the heels.
At an early age, the baby often instinctively touches himself, which is why an erection begins. Some parents observe this condition up to 5-7 times a day. From 1.5-2 to 3 years old, a boy most actively explores himself. At this time, you can already try to explain to the child what the parts of the body that are usually covered are called.
At 4-5 years old, a boy begins to study himself and those around him more specifically. Shows interest in the “structure” of the genital organs of the opposite sex
You should not stop “inconvenient” questions; it is important to answer them comprehensively and correctly: explain what behavior is acceptable in public and what is not, who can be allowed to touch themselves and who cannot. A reflex erection in boys at this age may be a reaction to tight underwear or trousers, or the touch of the mother - this should not be taken as a sign of sexual desire
At 6-7 years old, reflex reactions occur less frequently, but a boy can cause an erection consciously. There is no need to scold for attempts at masturbation and to be frightened by its sudden appearance - this can lead to psychogenic impotence in adulthood.
At 8-9 years of age, preparation for puberty begins, and at 10-11, some already experience their first emissions (involuntary ejaculation, mainly at night). Teenage erection becomes conscious - the boy reacts to explicit scenes or images
An erection can happen while bathing a baby or changing a diaper and is absolutely nothing to worry about.
How to cure a child?
Treatment of balanoposthitis should begin as early as possible. In case of acute inflammation, treatment involves the use of local baths with herbs or antiseptics (Furacilin solution), the use of ointments, antimicrobial drugs (antibiotics, antiviral or antifungal agents). A chamomile-based decoction is used for baths. Baths should be done several times a day at intervals of 2 hours. The temperature of the solution should be close to human body temperature. Hot water may cause burns. During treatment, you should wash your hands more often, shower regularly, or bathe your child without using irritating hygiene products.
Treatment of balanoposthitis in chronic form is more complex. The standard treatment regimen provides only a temporary effect. In this situation, treatment at home is ineffective. Surgical treatment (removal of the foreskin) is often performed. The operation is also indicated for developed phimosis. To prevent the development of balanoposthitis in a child, you should follow the recommendations:
- observe the rules of personal hygiene;
- do not use irritating creams and soaps;
- wear comfortable underwear made of natural fabric;
- do not touch the penis with dirty hands.
Thus, balanoposthitis is a common pathology among young children. With timely treatment and consultation with a doctor, this disease does not pose a threat to the baby’s health.
The genital organ of a newborn boy has always raised a lot of questions and fears among the whole family. Over time, any mother of her baby faces problems with the care and hygiene of the “main” organ of her beloved little one. The main goal here is not to touch it again, so as not to cause harm. in children, it mainly occurs in boys between the ages of birth and 5–6 years; in men it is detected quite rarely. This disease is called balanoposthitis, when the head of the penis and the inner sheet of the foreskin become inflamed. Almost every second child suffered such a disease in childhood.
In newborn babies, inflammation of the penis and its flesh is diagnosed quite often. At birth, the end of the flesh of a baby is narrowed and fused to the head. This most often leads to the onset of the disease. The toddler's behavior becomes restless, swelling and redness appear and, as a result, pain occurs. Since all children at birth already have physiological phimosis, the reasons for the appearance of balanoposthitis in them is the intervention of parents who forcibly tried to open the head of the penis. This effect on the foreskin leads to its tearing and penetration of infection inside. As the famous doctor, pediatrician Komarovsky says: “If the child is bathed regularly, he does not overheat, his diaper is changed on time, then there should be no problems. Parents themselves create, through their inept actions, a situation in which inflammation occurs. When the child is doing well and nothing is causing concern, there is no need to try to open the head of the foreskin on your own, even if someone strongly recommends that you do so.” When balanoposthitis is detected, treatment is required immediately so that the process does not develop into a complicated form.
What is “phimosis”
So, let’s understand the concept of “phimosis”. Phimosis in boys is the inability to expose the head of the penis . In any newborn boy, the head of the penis is covered with skin, which is called the foreskin. It performs certain functions, the main one of which is the protective function. The foreskin protects against damage and contamination. Over time, it begins to open, and if this does not happen, then this pathology is called phimosis, which comes in two types:
- physiological phimosis;
- pathological phimosis.
With the first form of pathology, there is no need to worry. Gradually the head of the penis will begin to open. This happens to almost all children by the time they reach puberty. Photos of a similar pathology can be seen on the Internet.
However, there is also a pathological form of phimosis in boys, and with this, a visit to the doctor can no longer be postponed for long. This diagnosis can be heard from a doctor when there is a pronounced narrowing of the foreskin. The reasons for such a diagnosis may be the individual characteristics of the connective tissue, the presence of microtraumas. We can talk about pathology when the following symptoms are present:
- the child has difficulty urinating;
- when urinating, the child begins to show anxiety and strain;
- the foreskin may fill with urine and a ball may be visible;
- redness may appear or the foreskin may become inflamed;
- urine may come out through the hole in a very thin stream or in the form of drops.
All these signs are a signal that the child needs to be seen by a doctor and may need the help of a specialist.
Is it necessary to do something if a boy has physiological phimosis?
A similar question arises for most parents faced with such a diagnosis. Doctors give different recommendations. Someone says that in this case there is no need to do anything and everything will be resolved by itself. Other pediatricians advise opening the foreskin little by little and gradually, thereby exposing the head of the genital organ, without waiting for it to open on its own. Well, you shouldn’t act according to the second advice, because there is a risk of causing more harm to the baby than good, damaging the organ itself or introducing an infection there.
Even the International Association of Pediatricians does not recommend doing this if the baby is diagnosed with physiological phimosis. Early and careless retraction of the foreskin can cause microcracks to appear. And after they heal , the narrowing will become even more significant.
It should be noted that this pathology in most cases goes away on its own, and only one percent of boys require medical help. This is usually required if the glans penis has not opened even between the ages of 14 and 17 years. In this case, consulting a doctor is simply necessary. Only he, after examination, can prescribe treatment, which can be either medicinal or surgical.
If phimosis in boys is pathological
When some of the symptoms described above are noted, we are talking about a pathological form of the disease. What to do in this case? The first thing to do is show the child to the doctor.
In some cases, the help of a surgeon is not even required, but an examination by a specialist still won’t hurt. The first thing that specialists are trying to do is to resort to conservative non-drug therapy. In some cases, treatment may be prescribed with certain medications that can be used at home. Experts have long developed non-drug conservative therapy and successfully use it for similar problems to this day. This technique involves gradually stretching the foreskin. It is recommended to do this daily for pathological forms of the disease. Such exercises are aimed at gradually stretching the foreskin and exposing the head of the penis. It should be noted that during such exercises it is necessary to comply with certain conditions, which include:
- You must first consult a specialist about the use of such a technique;
- it is necessary to stretch the foreskin gradually; you cannot immediately expose the head of the genital organ, otherwise you can damage it and cause pain;
- Such exercises must be carried out regularly.
Home treatment and medications can be used to treat phimosis in boys.
However, only a doctor can decide what medications are needed and whether their use is necessary. Doctors usually prescribe corticosteroid therapy to the patient. It consists in the fact that the child is prescribed an ointment based on corticosteroids. This ointment can help improve skin elasticity, reduce inflammation and swelling, and speed up the healing of small cracks. An example would be Prednitop ointment . Such ointments can be prescribed in combination with the exercises described above, that is, retracting the foreskin. All this contributes to the fact that there is a chance to deal with such a problem without surgical intervention.
The pathological form of phimosis in children can also be eliminated surgically, that is, with the help of surgery. This treatment is, of course, more complicated, but in some cases it is the only treatment option. This technique is used quite rarely and only in cases where the conservative technique did not produce positive results. If there are cicatricial changes in the foreskin, specialists perform partial or complete circular excision.
Reasons for appearance
All boys are born with physiological phimosis and a lubricant – smegma – collects inside them under the foreskin, which is very difficult to clean hygienically. Since this skin covers almost the entire head of the penis and is fused with it.
Here a favorable environment is formed for the activation and growth of pathogenic bacteria. Phimosis in boys persists until 5–6 years of age. Also, the cause may simply be poor hygiene of the child’s genital organ - this omission on the part of the parents gives rise to the occurrence of an inflammatory process. Some of the most common pathogens of this disease are staphylococcal infection, fungal infection, herpes virus, intestinal bacteria, and Proteus. In addition, there are other factors that can also cause the disease:
- incorrectly selected underwear (too tight synthetic panties that injure the child’s foreskin);
- allergies to detergents (washing powder, soap or hygiene gel);
- infrequent diaper changes for infants;
- too frequent intimate hygiene, with increased PH content;
- endocrine diseases (overweight, diabetes);
- lack of vitamins or other microelements;
- reduced immunity (causes fungal infection).
What to do with physiological phimosis?
This question arises for most parents. Komarovsky does not recommend treating physiological phimosis in boys, but advises waiting until puberty. Otherwise, irreparable harm may be caused to the newborn. Inaccurate manipulation of the foreskin often results in the appearance of microcracks. As they heal, a more pronounced narrowing may form.
If physiological phimosis has not resolved by the age of 14, you should consult a doctor for advice. Based on the physical examination, he will be able to prescribe medication. In rare cases, surgery is required. According to statistics, only one boy out of 2 thousand children needs surgery.
Symptoms of the disease
Signs of inflammation of the foreskin in children begin to manifest themselves gradually. Against the background of excellent health, the child after sleep experiences painful urination, itching, burning, and may experience restlessness and restlessness in behavior. The penis becomes swollen and red, this condition is accompanied by increased body temperature. If you do not pay due attention to these symptoms, the disease begins to progress. The lymph nodes in the groin enlarge, involuntary urinary incontinence may develop, purulent discharge is released from the urethra, the temperature rises to 39 degrees - this means that the disease has entered the acute phase.
Drug treatment
If the cause is poor hygiene, curing balanoposthitis will not be difficult. Parents are recommended to rinse the penis with Furacilin solution at the rate of 1-2 tablets per 100-200 ml of water or with a weak pale pink solution of potassium permanganate.
In this case, a bath with a decoction of Chamomile, St. John's wort, and Sage relieves inflammation very well. It is prepared strictly according to the instructions written on the package. The resulting solution is combined with warm boiled water and added to the bath. They are done 6–8 times a day for 15 minutes, alternating with each other. The water in which the child is placed should not exceed 37.2–37.5 degrees. You can do without a bath, simply dip the baby’s penis in a glass with these solutions for a long time, it all depends on how the child perceives such treatment. After washing the penis, you can drop 2-3 drops of sea buckthorn or vaseline oil into the gap. Under no circumstances should you expose the head of the penis from the foreskin during procedures; all preparations will reach the preputial sac on their own. With such active procedures, it will take only 2-3 days and there will be no trace of the disease left.
If the cause of inflammation of the foreskin is an infection that is detected after smear culture, then certain drug therapy is prescribed. The doctor selects the medications based on the results of the study. These may be antibiotics or antifungal medications. Local antiseptic procedures will also help treat inflammation. They consist of treating the affected area with disinfectants. Apply compresses soaked in an antiseptic to the affected area. Levomekol ointment, which has a powerful antiseptic effect, has proven itself very well; it is advisable to apply it before bed, wrap the head with a bandage and do not touch it until the morning. If the cause is a fungal infection, then Clotrimazole ointment is prescribed. All antiseptic drugs are used only as prescribed by a doctor; independent use is unacceptable.
Surgery
There are advanced cases of balanoposthitis, in which the disease cannot be cured. If all methods of drug treatment provide temporary relief and the symptoms return again, then it is recommended to resort to the surgical method.
Adhesions formed during physiological phimosis prevent the glans penis from opening slightly. The surgeon separates them from the foreskin and cleanses the pus and smegma that has accumulated inside, rinsing the cavity with chlorhexidine or hydrogen peroxide. This surgical intervention does not require anesthesia and is well tolerated by the child.
When the disease is in a chronic stage and periods of exacerbation alternate with remission, tissue deformation occurs and a complete narrowing of the foreskin may be observed. Then a purulent inflammation forms underneath it. In this condition, circumcision is prescribed - circumcision of the foreskin, after which the head of the penis comes out. This operation is performed under general anesthesia, and after it the patient recovers completely.
Symptoms of phimosis
The main manifestation of phimosis is difficult or completely impossible exposure of the glans penis. In addition, you may experience:
- weak stream when urinating (in especially severe forms, liquid is released drop by drop);
- painful urination;
- discharge of pus when pressing on the head of the penis;
- enlarged inguinal lymph nodes and increased temperature.
If phimosis is severe and provokes a complication - paraphimosis, then the head of the genital organ swells and turns blue. In this case, surgical intervention is necessary.
Preventive measures to help prevent inflammation
The main mission of parents is to observe the rules and norms of personal hygiene of the child, to provide proper care for the genital organ:
- Daily hygiene procedures (rinse the penis with warm water, without special detergents, after each bowel movement).
- Select high-quality cotton underwear that matches the size and age of the child (do not allow it to become dirty).
- Change the baby's diaper on time (try to use it only at night and for walks; when changing a diaper, give air baths, leaving the baby naked for 10–15 minutes).
- Do not try to forcibly open the leaves of the foreskin (you need to show the child to the doctor if he has noticed phimosis).
- Wash children's clothes only with special powders or laundry soap, without aggressive agents that can cause an allergic reaction in the genitals.
- Conduct regular preventive examinations with a pediatric surgeon for the purpose of early detection of pathology.
It is strongly recommended to completely cure any form of balanoposthitis so that it does not become chronic. It is important to understand that all boys between the ages of 0 and 10 years can experience physiological phimosis. The existing adhesions prevent the foreskin from being separated from the glans. They are destroyed independently when the body secretes a special secretion. If you forcefully release the head, you can get an infection that will cause an inflammatory process. It is dangerous for the development of serious complications, which may subsequently affect reproductive functions. And as the respected pediatrician Komarovsky says: “There is no need to climb there and pull anything unnecessarily, it is better not to touch anything at all, so as not to worsen the situation, and if in any doubt, it is better to seek help from a qualified family doctor.”
What should parents do?
First of all, says Evgeny Komarovsky, mothers and fathers should clearly understand that if a pediatric surgeon diagnoses a child with “phimosis,” then this is most often a diagnosis for the sake of diagnosis: the doctor is only stating a fact - the boy has a physiological narrowing of the foreskin. We already know that it is completely natural.
If such an unpleasant verdict is given to a teenager aged 15-16 years, and conservative measures (corticosteroid ointments and stretching) do not help, you should contact a surgeon for simple manipulations - circumcision. This will not make a man’s life worse at all, and in some ways will even improve it.
Five stages of sexual development
- The period from birth to the onset of puberty is considered to be the first stage of development - infantile, in other words, childhood. From a physiological point of view, no radical changes occur in the reproductive system at this time. Along with the overall growth of the child, the genitals also increase slightly (up to about 4-5 cm), the volume of the testicles can range from 0.7 to 3 cubic meters. cm, by the age of 6-7 years, as a rule, physiological phimosis disappears and the head of the penis has the opportunity to “see the light.” No secondary sexual characteristics are observed. This stage ends in boys by the age of 10-13 years. At the same time, some of them begin a period of rapid growth.
- The second stage, as it were, prepares the boy’s body for the drastic changes awaiting him. It is called the pituitary gland, and it is the beginning of puberty, or puberty (from the Latin pubertas - puberty). At this time, the pituitary gland is activated and the secretion of the hormones somatotropins and follitropin, which are responsible for the appearance of the initial signs of puberty, increases. First, the subcutaneous fat in the scrotum disappears, it increases in size, its pigmentation and many small folds appear. The testicles also increase in size and sink to the bottom of the scrotum. The growth of the penis begins, although its increase is not yet so noticeable. General growth continues, the outlines of the body begin to change.
- The third stage is the stage of activation of the sex glands (gonads). The gonads begin to produce male and female hormones (androgens and estrogens), and the development of the genital organs and secondary sexual characteristics continues. At the age of 12-13, pubic hair growth sometimes begins - the first hairs appear at the base of the penis. At 13-14 years old, pubic hair darkens, becomes coarser, and spreads towards the legs. The penis lengthens, the scrotum and testicles continue to grow.
- The fourth stage is the stage of greatest activity of the gonads. In boys, it begins on average at 12-14 years of age. During this period, the outlines of the body and face become more mature. The penis begins to grow not only in length, but also in thickness, and the growth of the scrotum and testicles continues. “Vegetation” appears above the upper lip and in the armpits, as well as around the anus. At the same age, under the influence of testosterone, due to the development of the muscles of the larynx and the lengthening of the vocal cords, the boy’s voice begins to “break”: it becomes rougher and deeper. The thyroid cartilage of the larynx, the so-called “Adam's apple,” begins to grow. The appearance of pain in the nipple area in a child is also an indicator of normal sexual development. Some breast enlargement is also possible - this is the so-called physiological gynecomastia, which is also not a pathology. By the age of 15, many young men already produce mature sperm, which mature continuously. At the same age, the first emissions may appear - spontaneous, usually nocturnal, ejaculations.
- The fifth stage is characterized by the final formation of the reproductive system. By this time, the genitals reach “adult” sizes, secondary sexual characteristics are also fully expressed - hair growth of the pubis, lower abdomen and face is completed, the physique and facial features finally acquire a masculine appearance. Around this time, body growth generally ends, although in some young people it continues until the age of 20-22. Puberty in boys ends by the age of 17-18, with significant fluctuations of 2-3 years possible. Physiologically, they are already ready for procreation, but psychological maturity will come later.
We invite you to familiarize yourself with Inclusions in seminal fluid
Dear Parents! Let me emphasize once again that the above data reflect only the average norms of sexual development of young representatives of the stronger sex. Depending on the individual characteristics of the child’s body, quite significant deviations from the “arithmetic mean” are possible.
Relaxed penis sizes for teenagers
| Age | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| Height (cm) | 142±6 | 147±7 | 152±8 | 160±8 | 167±8 | 171±8 | 173±6 | 175±6 |
| Member (cm) | 4±1 | 5±1 | 6±1 | 7±1 | 7±1 | 8±1,5 | 9±1,5 | 10±1,5 |
| Age | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
| Penis length (cm) | 10,4 | 13,0 | 15,2 | 15,5 | 16,5 | 17,0 | 16,5 | 16,5 |
| Age | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
| Penis girth(cm) | 7,6 | 9,9 | 10,5 | 11,0 | 11,5 | 12,0 | 13,0 | 13,0 |