There is practically no woman who has never experienced troubles associated with thrush in her life.
In fact, this harmless term “thrush” means nothing more than vulvovaginal candidiasis, that is, inflammation of the external genitalia and vagina caused by fungi of the genus Candida. In addition to the feeling of discomfort from the manifestation of the disease, a pregnant woman has a lot of questions: how did she become infected, is her partner to blame? But the most important questions are: how will the infection affect the course of pregnancy, should it be treated and with what, is treatment harmful for the unborn baby?
Over the past two decades, the frequency of this pathology has increased 7 times; thrush has become more common in early pregnancy.
Where does thrush come from?
Fungi of the genus Candida are opportunistic. This means that they can exist in the human body for a long time without causing any harm. But under the combination of certain conditions they become pathogenic, that is, they begin to manifest themselves, causing certain complaints in a person. That's why you shouldn't rush to accuse your partner of infidelity - the appearance of signs of thrush most likely indicates a problem in your body.
The state of pregnancy cannot be attributed to troubles, but thrush during pregnancy occurs quite reasonably and often (up to 50.8%). Some expectant mothers first encounter this disease during pregnancy.
- First, pregnancy changes the state of the body's immune defenses. Paradoxically, the immune system ceases to keep the pregnant woman’s body at a high level of resistance. It would seem that it should be the other way around, who, no matter how the expectant mother and child, should be protected from all sorts of microbes. But wise nature judged in its own way. The organism emerging in the mother's body is for her a set of foreign proteins, which, with a high level of immunity, should be rejected. By saving the child from rejection, nature “turns off” the defense mechanism, making the mother more vulnerable to infections, including her own pathogenic fungi.
- Secondly, the hormonal background changing during pregnancy leads to proliferation (increase in the number) of vaginal epithelial cells rich in glycogen. Glycogen is converted into glucose, which serves as an excellent food for fungi.
- Thirdly, the thrush fungus, having attached itself to the vaginal mucosa, forms colonies, displacing the normal flora (lactobacteria), and further weakens local immunity.
Thrush at the beginning of pregnancy is more likely to occur against the background of:
- Long-term use of oral contraceptives prior to pregnancy.
- Uncontrolled use of antibiotics.
- Treatment with glucocorticosteroids.
- Metabolic disorders.
- Diseases of the gastrointestinal tract, dysbacteriosis.
- Endocrine disorders in diseases of the thyroid gland, adrenal glands, diabetes mellitus.
- Hypo- and avitaminosis.
Immunodeficiencies that occur against the background of chronic intoxication, cancer, and in HIV-infected people are always accompanied by the appearance of thrush.
Do not forget that it is candidiasis that first appears in the early stages of pregnancy that is the first marker of these terrible diseases. This is another argument in favor of early contact with the antenatal clinic at the beginning of pregnancy.
Causes of thrush in pregnant women
The main causes of thrush during this period are hormonal “storms” during pregnancy, as well as lifestyle habits before pregnancy. If you notice at least one of the reasons listed below, then you are at risk and you should be careful.
- Hormonal changes in the body during pregnancy. The hormone progesterone, which is responsible for pregnancy, comes to the fore. It increases the acidity of the shells, which is a positive habitat for fungi of the genus Candida.
- Unnatural changes in hormonal levels. It may occur, for example, when taking contraceptives and as a result of their cancellation, during menstrual irregularities, etc.
- Vaginal microflora disorders or dysbiosis. This disease may be asymptomatic. Normally, a woman should have virtually no discharge other than a small amount of mucus. There should also be no dryness or discomfort, including during sexual intercourse. If there is at least one sign, then you should consult a doctor for a gynecological examination and take material for tests, including cytological.
- Incorrect or prolonged period of taking antibiotics. Antibacterial drugs are aimed at combating pathogenic bacteria, but beneficial bacteria are also exposed to them. When they are destroyed, the background of the mucous membranes changes and local immunity decreases. This provides an excellent opportunity for the development of pathogenic microflora, which includes Candida.
- Consequences of operations, trauma to mucous membranes.
- Incorrectly selected underwear: if it is too small, normal blood circulation is disrupted. You should also pay attention to thong panties; you shouldn’t get carried away with them.
- Mistakes in personal hygiene.
- Decreased immunity due to infectious diseases.
- The presence of diseases that are sexually transmitted.
As you can see, there are a lot of reasons for the development of thrush. And in order to prevent illness, you should be vigilant.
Symptoms in early pregnancy
Currently, more than 200 species of Candida fungi are known. There is no need to specify whether it belongs to one species or another, but for information, it should be borne in mind that the nature of the discharge from the genital tract may vary: from cheesy to creamy mucous. More often, the discharge is cheesy in nature (in 95% of cases).
A feature of thrush during pregnancy, in contrast to gynecological patients, is the absence of complaints in the presence of discharge:
- When examining the mucous membrane of the vaginal opening, vagina, cervix, external urethral opening, pastiness, friability and swelling are determined.
- The color of the mucous membrane changes from pale pink to red-bluish.
- There is a cheesy discharge on the walls of the vagina and inside it, sometimes in significant quantities (up to half a glass or more).
- When a secondary banal or specific infection occurs, the color of the discharge may change to yellowish-green. This creates an unpleasant sour smell.
Only a small number of pregnant women in the early stages may have “classic” symptoms of thrush:
- Burning, itching in the vagina, which is sometimes unbearable. The burning sensation often intensifies when washing, after sexual intercourse, in the evening and at night.
- Discomfort and burning when urinating.
- Dyspareunia (painful sexual intercourse).
- Irritability, insomnia, nervousness.
- Characteristic cheesy discharge.
Ongoing research:
- To confirm the diagnosis, a laboratory diagnosis of a smear taken during examination of the pregnant woman is sufficient. During microscopy, the laboratory assistant finds mycelium and threads of the fungus.
- Cultural diagnostics (culture on media) is carried out in case of long-term unsuccessful treatment.
- Immunological methods are extremely rarely used to detect antibodies to Candida fungi and its species.
- The PCR polymerase chain reaction method has also not been widely used for diagnosing Candida yeast because of the large number of false positive results.
The disease can last a long time. The duration of thrush up to 2 months is considered an acute process, beyond this time it is considered chronic. Chronic thrush can recur.
Why is it dangerous?
You say: “Such a nice, kind name, especially since the fungi are our own, not strangers, there are practically no complaints. What is there to treat?” And you will be completely wrong! Although seemingly harmless, thrush poses a serious danger to the expectant mother and child at all stages of pregnancy and the postpartum period:
- In the early stages, against the background of thrush, early gestosis is more common. Their course is more severe and prolonged than during the normal course of pregnancy.
- A dangerous complication that threatens pregnancy loss, early and other miscarriage.
- When asked whether a child born from a sick mother can have thrush, unfortunately, doctors give a positive answer. Thus, in utero, a baby can get congenital candidiasis, which often causes stillbirths and death of the child after childbirth. In 30% of all perinatal deaths, the child had signs of thrush. Thrush penetrates all organs and tissues; there may be candidiasis of the intestines and pneumonia.
- In turn, acquired candidiasis in an infant occurs due to contact of the child’s skin with the mother’s infected genitals. Yeast stomatitis is common, and candidiasis dermatitis is also possible.
- The frequency of late gestosis, pathology of the placenta, abruption of the normally attached placenta and anomalies of its attachment is increasing.
- During childbirth, labor anomalies, untimely rupture of water, increased maternal trauma, and bleeding in the postpartum and early postpartum period are possible.
- Also, after childbirth, there is a high probability of developing purulent-septic complications.
In some cases, when thrush is not severe, if the woman refuses treatment, the pregnancy ends with a normal birth and on time. Moreover, the mother can please her loved ones with a healthy baby.
Children from mothers with thrush are often born in a state of chronic hypoxia and with low weight.
Symptoms
The main symptoms of thrush that a woman can identify include:
- Itching in the genital area, which is sometimes very difficult to bear. As a result, a woman can scratch some areas until small wounds appear.
- Burning in the vaginal area.
- Vaginal discharge is white, has a specific sour odor and a cheesy consistency.
Why does thrush “attack” pregnant women? Doctors say that Candida fungi live in the body of almost all people, both women and men, and may not make themselves felt for years.
Frequent cases of thrush during pregnancy are a consequence of a significant decrease in the immunity of the expectant mother. The body is weakened, and fungi begin to rapidly multiply on the vaginal mucosa.
How to treat?
After reading the list of possible complications, I want to run to the pharmacy to buy some super-effective remedy against “that lady with the cans,” as was recently shown in an advertisement on TV. And this is the mistake of expectant mothers - self-medication can also cause negative consequences in the child. Therefore, an experienced doctor should select therapy.
There are plenty of anti-candidiasis remedies in the pharmacy:
- Old time-tested polyene series (Nystatin, Levorin, Pimafucin).
- Imidazole derivatives (Clotrimazole, Miconazole).
- Triazolones (Fluconazole, Intraconazole).
- Combined (Terzhinan, Polygynax, Klion D, Imozimaza).
Many drugs can be prescribed only after 12 weeks, having previously assessed the harmful effects on the fetus and the possibility of complications. On the eve of childbirth, you can use Polygynax suppositories for a short course. Five-day use of Polygynax suppositories 2 times a day sanitizes the birth canal on the eve of childbirth.
Old, harmless, but ineffective methods of treatment are now recommended as traditional ones. These include:
- Douching with a 2% soda solution.
- Borax tampons in glycerin.
- Treatment with brilliant green.
- Douching with a decoction of oak bark.
- Kefir tampons.
When using folk remedies, we must remember that if there is a threat of miscarriage, any manipulation in the cervical area is prohibited.
During treatment, it is recommended to follow a diet. You should exclude sugar, honey, bread, and baked goods made from yeast dough from your diet.
Pimafucin
Most doctors agree that the drug of choice for treating thrush in early pregnancy is Pimafucin. It is completely safe for the fetus and does not interfere with the content of the vaginal bacillus, although the main active ingredient is the antibiotic natamycin.
Pimafucin in the form of vaginal suppositories is suitable for early pregnant women. They are inserted deep into the vagina at night. The course continues after the symptoms disappear for another 2-3 days. After a course of Pimafucin suppositories, it is useful to consolidate the result with Acylact suppositories in the vagina.
The disadvantage of Pimafucin is its low effectiveness and relapses in the third trimester of pregnancy. When using Pimafucin suppositories, slight itching in the vagina may occur, and nausea and vomiting are extremely rare.
Useful tips
When treating thrush in pregnant women in the early stages, it is necessary to follow some rules. And the most important of them: treatment should be carried out according to the principle “Do no harm!”, especially to the fetus in the early stages.
What you should know about treating the disease:
- The treatment regimen consists of 2 stages: against thrush, then to restore the vaginal flora.
- Local treatment should be preferred, because with it the sanitation of the vagina occurs faster, relapses occur less frequently, the trophism of the vaginal mucosa improves and the restoration of the vaginal biocenosis.
- Remember that Candida fungi have not only developed resistance to some antibiotics, but have learned to feed on them.
- It is difficult to treat thrush in pregnant women, since the fungus can “hide” in the cells of the vaginal epithelium.
- Treatment should only be prescribed by a doctor.
Opinions differ regarding the treatment of the sexual partner, but no one denies sexual rest during the period of treatment.
Why is thrush dangerous during pregnancy?
https://youtu.be/rAFuWHnJDsA
There is an opinion that thrush during pregnancy does not harm the unborn child and his mother. Firstly, even if this were true, this would not mean at all that the disease does not need to be treated. Secondly, in fact, thrush, like any other infection, is a potential danger.
This disease, in addition to noticeable discomfort, complicates the course of pregnancy itself and can negatively affect the process of childbirth itself. Thus, thrush can become a “catalyst” for uterine erosion, which provokes a loss of elasticity in the vagina. In this regard, the risk of internal and external ruptures during childbirth increases significantly.
Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
Thrush during pregnancy is also dangerous because it can easily be passed on to the baby: the lack of proper treatment increases the risk of infection of the fetus and newborn. For example, a mother can infect a newborn, as a result of which thrush can “settle” in the baby’s mouth, which will complicate feeding in the future.
If thrush is transmitted from the mother to the baby, already in the second week after birth, doctors, as a rule, diagnose the so-called candidal stomatitis in the newborn.
But the worst outcome that thrush can cause during pregnancy is the death of the baby: a tragic outcome is possible if the vital organs and systems of the fetus are affected by infection. That is why treatment of thrush during pregnancy is extremely necessary, and the problem cannot be ignored under any circumstances.
Specifics of thrush during pregnancy
Pregnancy is a special condition, and the use of most medications to treat certain diseases is simply not acceptable. This is also relevant for thrush.
Therefore, you should not listen to advertisements that claim that after a few days of using this or that drug everything will return to normal, since it is not a fact that it is approved for the treatment of thrush in an “interesting situation.”
The first thing you need to do is go to a doctor who will establish an accurate diagnosis and prescribe a treatment that will not harm the course of the pregnancy and the baby itself.
Prevention
Treatment of diseases in the early stages of pregnancy is always problematic, because you need to choose a medicine so that the fetus is not harmed. And since thrush often occurs in expectant mothers, it is advisable to take preventive measures.
What is meant by thrush prevention:
- A healthy lifestyle, good sleep, a balanced diet including vitamin and mineral complexes help the immune system to be in working order.
- Increase stress resistance and positive attitude. Adequate physical activity is also recommended.
- Replace synthetic tight-fitting underwear with comfortable cotton panties, and it’s better to sleep without them at all.
- It is very important to follow the rules of personal intimate hygiene: wash with warm water without soap at least 2 times a day. You can use special intimate hygiene products instead of soap.
- It is better to plan pregnancy in advance. The couple should be examined for the presence of genital tract infections and any existing ones should be treated in a timely manner.
- Carry out your pregnancy under the supervision of an obstetrician-gynecologist.
You should not self-medicate thrush. The doctor will select individual treatment regimens for you.
How to treat thrush during pregnancy
Thrush can be identified at home based on general symptoms, but the diagnosis will be inaccurate.
After all, a number of other sexually transmitted infections have the same symptoms. Therefore, the final diagnosis will be made only by a gynecologist after bacterioscopy (popularly, taking a smear). It is necessary to treat thrush during pregnancy. Firstly, few women will be able to tolerate its symptoms for a long time. Secondly, it is still an infection, so it can negatively affect the baby. This issue has not yet been fully studied, but doctors are unanimous in one thing - it is necessary to treat. But how, since most medications are contraindicated during pregnancy?
Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
You should not self-medicate so as not to harm the fetus. But if the doctor has prescribed a remedy, you can use it, especially if the instructions do not say otherwise. Pregnant women treat thrush exclusively with topical medications. Most often these are vaginal suppositories or tablets, sometimes creams or ointments.
They are safe, but do not have a very long-lasting effect. This is their main drawback, so the disease has to be treated again and again. There are also traditional methods that may help for a short time. But they should also be recommended exclusively by a doctor.
For example, many gynecologists advise washing the genitals with a solution of soda, a decoction of oak bark, etc. This treatment is purely symptomatic and short-term, but can reduce the woman’s discomfort. If it is determined that the cause of thrush is chronic diseases of the pregnant woman or a deficiency of vitamins, measures should be taken to eliminate these problems.
And then the thrush will retreat. The problem is that during pregnancy it is very difficult to treat serious chronic diseases, because most drugs are also contraindicated. Thrush during pregnancy is an unpleasant but quite common occurrence.
It will definitely remain a thing of the past after childbirth, but in the meantime you should try to alleviate its symptoms by following the recommendations of your gynecologist.
Pathogenesis
Fungi belonging to the genus Candida are opportunistic microorganisms that widely inhabit the external environment, growing mainly in the soil, on fruit trees, and on fruits.
In the form of saprophytes, fungi can be found on the skin and mucous membranes, as well as in the feces of every fifth healthy person.
The transition of an opportunistic fungus to a pathogenic form is facilitated by external and internal factors.
External factors can be:
- climate features, high humidity;
- mechanical irritation of mucous membranes.
Even more interesting:
The echo structure is not changed, what does this mean?
Tongue with pharyngitis photo
Internal factors are considered:
- metabolic diseases;
- deficiency of certain vitamins in the body;
- any immunodeficiency conditions;
- prolonged or uncontrolled treatment with antibiotics, hormones, cytostatics, etc.
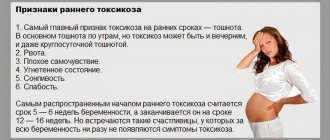
Often, the activation of fungi at the beginning of pregnancy is associated with the onset of early toxicosis in a woman: the weakened female body suffers especially during this period. Poor nutrition, weight loss, anemia, immunosuppression - this is not a complete list of signs accompanying early toxicosis. All this leads to the body’s own defenses failing, and the fungal infection becoming more active.
[13], [14], [15], [16]
Comprehensive treatment of thrush
Treatment of illness caused by Candida fungi during the first weeks of pregnancy will be limited to a minimum of medical resources. In particular, until a period of 8 weeks is reached, it is strongly recommended to completely abstain from taking all medications and drugs, because at this time the internal organs of the embryo are formed.
1 teaspoon of soda per 1 liter of boiled water at room temperature. The use of such a solution will help relieve irritation of the mucous membrane, and will also create extremely unfavorable conditions that prevent the growth of fungus.
After the first 8 weeks of pregnancy have passed, a special antifungal drug called Pimafucin can be used to treat a disease popularly called thrush in the early stages of pregnancy.
The treatment regimen for neem is as follows: 1 capsule is applied at night, the procedure should be repeated for exactly 6 days. In advanced or chronic forms of this infection, the course of treatment, and therefore the number of procedures, can be extended and reach 10 days.
You should also pay close attention to the fact that none of the other antifungal drugs, be they local or systemic, can be used at all in the initial stages of pregnancy.
In many cases, thrush, which appears in the initial stages of pregnancy, responds well to the above therapy. But, if for some reason relapses occur, then this type of therapy can be repeated many times, using the same vaginal suppositories called “Pimafucin”.
Complications and consequences
What can happen if thrush that occurs in the early stages is not treated?
- Long-term candidiasis can lead to decreased elasticity of vaginal tissues. What does this mean: birth ruptures, long treatment.
- During childbirth, a fungal infection can get on the baby's mucous membrane.
- Weakened immunity due to a fungal infection can cause the development of other diseases, for example, frequent colds, intestinal diseases and upper respiratory tract diseases.
Contrary to general belief, spontaneous abortion due to untreated thrush is extremely rare. The effect of thrush on early pregnancy is negative only in isolated cases. As a rule, if a woman consults a doctor on time, any manifestations and complications of thrush are eliminated and prevented.
[17], [18], [19]
Folk remedies for thrush
It doesn’t matter whether thrush started after ovulation or in the last trimester of pregnancy, in any case, the woman needs to undergo treatment and get rid of this disease.
In addition to medications, doctors often recommend effective folk remedies and give advice on hygiene and wearing underwear. You should also follow a diet for thrush during treatment - the fungus “loves” sweets, yeast baked goods. We need to give them up.
Below are traditional medicine recipes that can be used independently or in combination with traditional therapy. A cloth or gauze is soaked in this solution and applied as a compress to the genitals. This will quickly relieve itching and inflammation.
Chamomile for candidiasis
Chamomile is known to great-grandmothers as an anti-inflammatory agent. It will relieve swelling and kill harmful microorganisms. Chamomile is used to make decoctions that are used internally and externally. To prepare a solution for washing, take 1 tbsp. l. chamomile, pour a glass of boiling water, heat for 15 minutes and filter. Can be used as compresses or for washing. Douching is not recommended for pregnant women.
For greater effect, add calendula to chamomile. To prepare the solution, take 1 liter of water and add 1 tbsp. l. chamomile and calendula, heat for 15 minutes, cool and filter. This is an excellent cleanser.
Is it worthwhile to carry out treatment in the 1st trimester?
Since the disease poses a serious threat to the health of the mother and the development of the child, it is necessary to treat candidiasis.
However, the greatest effect is obtained by taking antifungal drugs for thrush orally, which is strictly prohibited in the first trimester.
Typically, treatment for thrush in the first weeks of pregnancy is carried out to eliminate symptoms and ensure the woman’s comfort and reduce the risk of complications.
During this period, the final formation of the fetal placenta occurs, and the child is more protected from toxic substances that enter the bloodstream when using medications.
In addition, the formation of internal organs is almost completely completed, so the risk of disrupting their development is significantly reduced. It is advisable to treat thrush before labor begins to avoid infection of the fetus during its passage through the birth canal.