For some reason, many young mothers are quite pessimistic about breastfeeding after a caesarean section, and believe that it is impossible to establish lactation if there has been an operation.
Undoubtedly, due to surgical intervention in the process of bringing the baby into the world, it may take longer for milk to “receive” than during natural delivery. But this does not mean at all that the newborn will have to grow up on artificial formula. Let's talk about how a young mother can “make” the body systems that are responsible for producing nutrition for the baby work. We will also consider in detail what problems associated with lactation can arise as a result of CS.
How to establish breastfeeding after cesarean section
It is noteworthy that women who have undergone “upper birth” began breastfeeding not so long ago. Some 40 years ago, only 2% of newborns born through CS grew up on mother's milk. In the 70s and 80s, manufacturers of artificial mixtures began to appear, like mushrooms after the rain, and HF depreciated in value. In those days, CS was quite a rare occurrence, and all operations were performed only under general anesthesia. All this contributed to the widespread opinion that breastfeeding is impossible after surgical delivery.
Are you planning to breastfeed or bottle-feed?
GVIV
Today the situation has changed dramatically, and almost all babies can enjoy their mother's milk. The process of establishing lactation, thanks to the enormous work done over the years by specialists in the field of medicine, has been significantly simplified.
So, here are recommendations on how to establish breastfeeding after a caesarean section:
- Attaching a newborn to the breast. There is a common misconception that you should not feed your baby immediately after a CS. Yes, indeed, the sucking reflex does not immediately awaken in a child born through surgical intervention. But already within 4–6 hours after the baby is born, you can and even need to feed it. It will be quite difficult for a mother who has recently undergone surgery to organize this process on her own, so the help of medical staff or, even better, a loved one will not be superfluous.
- Stop, bottle. We are not talking about newfangled drinking vessels that prevent liquids from spilling. On the contrary, even if a newborn very strongly asks to eat, communicating this with loud crying, giving him a bottle with an artificial formula is extremely undesirable. It is optimal if the baby’s first “dish” is colostrum. In the meantime, while mom is recovering from anesthesia, dad or grandma will help establish contact with the baby (bring him to the breast).
- Stimulation of milk production. Even if it was not possible to establish lactation immediately after childbirth, there is no need to give up. While still in the maternity hospital, and after being discharged home, you need to regularly knead your breasts and try to express milk. At this time, the baby can be on artificial formulas and receive his “moral compensation” when the mother’s milk production improves.
- Meal upon request. Even if a newborn eats from a bottle due to lack of milk from the mother, it is necessary to offer the baby the breast as often as possible. It’s even better to organize free access for the child to it, for example, carry him in a sling, often practice skin-to-skin contact, etc.
Important! If you have to feed your baby formula during the breastfeeding recovery period, it is better not to use a bottle.
The best option is to use a system for supplementary feeding at the breast, which will allow you to control the amount of food consumed and help the newborn learn how to properly latch onto the nipple.
The timing of the operation is a decisive factor
Lactation after cesarean section depends to a large extent on when the surgery was performed: before the onset of labor or after the first contractions appear. The onset of labor is triggered by the hormone oxytocin, which is also responsible for the appearance of the first milk - colostrum - in a woman's breast. That is, a woman who had a caesarean section during the initial contractions can produce breast milk in almost the same way as a mother who gave birth naturally. Usually milk arrives 3-4 days after birth.
In the first days, colostrum is produced in the breast. This is a particularly valuable substance that contains many vitamins, nutrients and immunomodulatory components. Just 5-10 ml can saturate a newborn. As a rule, there is very little of this “first” milk both in women who have undergone physiological labor and in those who have had a cesarean section. Therefore, it is possible to say when milk appears after a caesarean section when the nature of the operation is known.
If a caesarean section was performed as planned, before the onset of contractions in a woman, then the natural chain of hormonal processes is disrupted, or rather, it is delayed. After surgical delivery, the body of a woman in labor restores the production of oxytocin a little later. Colostrum may appear 1-2 days later than during physiological labor. “Mature” milk will begin to be produced 4-9 days after surgery.
In primiparous women, lactation appears somewhat later than in subsequent pregnancies. The ducts of the mammary glands are still closed and not fully formed, the physiological “program” of feeding is being established for the first time. This is true for both women who have had a natural birth and women who have had a cesarean section. Therefore, breastfeeding after a cesarean section will be faster for multiparous women than for first-born women.
Painkillers during breastfeeding
It is no secret that establishing lactation is associated with quite severe painful manifestations. In addition, after a CS, a young mother may be bothered by headaches, aching sensations in the suture area, pain in the abdomen, etc. Is the use of analgesics allowed in such cases?
Painkillers during breastfeeding should:
- Be non-toxic.
- Enter the blood in minimal quantities.
- Do not affect the composition of breast milk.
- Quickly eliminated from the body (maximum 4 hours).
- Be compatible with the lactation process.
- Act quickly.
- Contain a minimum of components (optimally 1 active ingredient).
- Do not cause side effects.
Paracetamol and ibuprofen-based drugs best meet all of the above requirements. You can safely take children's syrups - Efferalgan or Panadol.
But in any case, consultation with your doctor, including a pediatrician, is necessary. Only a specialist can accurately determine whether it is permissible to take certain tablets/syrups in a particular situation.
Some women mistakenly believe that analgesics in small doses will not harm the baby. It is worth considering that the drug gets into the milk in any case (even if it is only half a tablet) and can cause irreparable damage to the health of the baby.
Important! Painkillers should be taken only after the newborn is put to the breast. This minimizes the risk of harm to the baby - before the next feeding, most of the medicine will have time to be eliminated from the body.
How does taking medications affect?
It is important to consider that the mother takes painkillers, which pass into breast milk. You can take medications based on paracetamol, ibuprofen, etc. You cannot take codeine, products containing analgin and aspirin. The woman in labor is prescribed antibiotics to avoid inflammatory processes. Whether it is possible to breastfeed a baby in such circumstances and on what day, the doctor will tell you. It depends on the condition of the woman in labor and on the medications prescribed to her.
The newborn may experience drowsiness due to the anesthesia. The baby should be woken up for the first breastfeeding. In this case, the baby may suck sluggishly, since the sucking reflex is impaired. Therefore, breastfeeding after cesarean section using general anesthesia involves great efforts to establish it.
We can draw conclusions:
- The appearance of milk is affected by the time of the operation.
- Milk production depends on the first attachment to the breast.
- The rate at which lactation appears is determined by the choice of type of anesthesia.
- Breastfeeding depends on the baby's sucking activity to ensure the breasts are emptied.
- The appearance of milk in women in labor during repeated pregnancies occurs faster than in first-time mothers.
- Establishing lactation depends on the genetic characteristics of the woman.
How to develop breasts after cesarean
We found out above that caesarean section and breastfeeding are quite peacefully coexisting concepts, contrary to popular contrary opinion. Next, we’ll look at how to develop the breasts so that milk flows in sufficient volume and with minimal pain. The first thing a woman in labor should take care of literally the next day after the CS is her own proper nutrition.
It is optimal to adhere to the following menu for the first few weeks:
- Breakfast: porridge (oatmeal, buckwheat), boiled in water, tea (preferably green), bread with low-fat butter.
- Lunch: vegetable soups, steamed beef cutlets, mashed potatoes, dried fruit uzvar.
- Dinners: baked apples, low-fat cottage cheese with sour cream (fat content no higher than 15), kefir.
By eating this way, a young mother will not only ensure stable lactation, but will also be able to recover faster after undergoing abdominal surgery.
As for the development of mammary glands directly, the process consists of the following activities:
- Washing your breasts with warm water (you can practice a non-hot shower) several times a day - this will help improve blood circulation in the mammary glands and ensure the expansion of their ducts.
- A massage that begins with light stroking, smoothly turning into gentle kneading of the chest. Strong compression of the nipples should be avoided, movements should be careful.
- Creating compression, which involves lifting the chest with one hand while simultaneously pressing on it with the palm of the other hand.
- Expressing milk from the glands using light squeezing movements - at this time it is very important to control your own sensations.
- Applying cool compresses to the chest - the procedure lasts up to 10 minutes.
All of the above activities should be performed in strict sequence 5–7 times throughout the day. If positive dynamics are not observed, you should consult with a specialist who will determine the causes of milk stagnation and prescribe therapy.
How long does it take for milk to come in after a caesarean section?
Milk production in the mother's breast or lactation depends on only two hormones: prolactin and oxytocin.
Prolactin is produced in the body already during pregnancy and helps the breasts fill with milk. Oxytocin is responsible for the contraction of the pectoral muscles and the flow of milk through the thoracic canals to the nipple. Knowing about the work of these hormones, you can artificially control them, namely:
- Prolactin can be stimulated by frequently putting the baby to the breast;
- and oxytocin is produced when a baby sucks at the breast.
Therefore, having learned that you need a caesarean section, talk to your doctor in advance about how you want to feed your baby naturally and discuss the conditions of birth.
Possible problems after surgery
Of course, breastfeeding a newborn during a caesarean section has some peculiarities. But by preparing for possible difficulties in advance, mom will be able to overcome them with ease.
Let's highlight the 5 most common problems:
- No. 1 – the impossibility of early attachment of a newborn to the breast. The reason may be the poor health of the mother after anesthesia or the lack of sucking activity in the child. Nothing bad will happen if the baby has to eat artificial formula for the first 24 hours until the mother fully recovers. If the baby does not want to suckle, you should offer feeding for every concern - after a few hours the newborn will definitely show activity.
- No. 2 – prescription of medications. Often, women in labor are prescribed a course of antibiotics to exclude possible infectious complications after a CS. In such cases, it is necessary to postpone breastfeeding, giving preference to formula. But it is necessary to maintain lactation by systematically expressing milk.
- No. 3 – the newborn’s refusal to breastfeed after supplementary feeding. If a child, due to circumstances, is accustomed to a bottle nipple, it will be difficult for him to latch onto the breast correctly. At first, the baby will need to be helped in this process, paying attention so that it captures the entire areola, and not just the nipple.
- No. 4 – choosing a comfortable position for feeding. Of course, sitting for a long time to feed a child is very difficult for a woman who has undergone surgery. The way out of the situation is feeding, in a lying position or “from under the arm.”
- No. 5 – lack of milk. It is normal for lactation to fully improve only a week after the CS. Therefore, do not be alarmed if the baby does not have enough milk before this period; supplementary feeding will save you in such cases.
In general, the problems that may arise with lactation after surgical childbirth are no different from those that appear in mothers who gave birth to children naturally.
How does lactation develop?
The problem when there is no milk for a long time after a caesarean section worries many women. But waiting until the process of its production begins on its own is wrong. Already in the intensive care unit, it is important to put the baby to the breast and stimulate the production of colostrum. At first, it will be released drop by drop until the level of oxytocin and prolactin, the hormones responsible for milk production, begins to rise.
It is not always possible for a woman who has undergone such a complex operation as a caesarean section to immediately begin to establish natural feeding. Various circumstances can interfere with this, for example, being in different rooms with the baby, prescribing broad-spectrum antibiotics, placing the newborn in an incubator or connecting to an artificial respiration apparatus. It is important to overcome difficulties in order to give the baby the opportunity to feed on mother's milk, a valuable source of vitamins and minerals.
Antibacterial drugs are prescribed after cesarean section for prophylactic purposes to avoid the development of an inflammatory process in the uterus. Young mothers worry that medications will change the composition of the milk and harm the baby, but such fears are not always justified.
Firstly, a specialist prescribes antibiotics for medicinal purposes, so you cannot refuse injections or tablets on your own. And secondly, today there are a lot of drugs that pass into breast milk in small amounts, which will not harm the newborn and will not affect the lactation process.
In some cases, after a cesarean section, a woman may be prescribed antibiotics.
If the baby is weak and reflexes are inhibited, the first feeding can be postponed for 5-6 hours, but not later. Full attachment involves the newborn sucking on one breast and then the other for at least 15 minutes on each. The main condition is that the first thing that enters the child’s mouth should be the mother’s mammary gland. In no case should you use a pacifier or a rubber nipple; this point is important to discuss with doctors before the start of the cesarean operation.
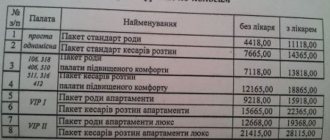
With this approach, it will be possible to maintain lactation, even if the baby is not in the same room as the mother. You can ask the grandmother to be in the intensive care unit with the woman and help in caring for the baby (this is allowed in paid maternity hospitals).
In the event of a difficult birth after a caesarean section, the woman may be transferred to the intensive care unit
Lack of milk
What to do if a nursing mother has little milk after a cesarean section? First you need to make sure that the baby is really not eating enough - conduct a test developed by WHO. The number of urinations in the first two days is two times every day, on the third day it increases to four times, on the sixth – to six. Under such conditions, there is no need for complementary feeding.
If the mother really has little milk, it is important to try to establish lactation and start supplementary feeding. First, the baby is applied to the breast, then food is given from a syringe or spoon, and the process is completed by applying it to the breast again. Three days later, a diaper test is carried out and if the milk volume increases, supplementary feeding is abandoned.
When combining artificial and natural feeding, the volume of the formula is gradually reduced, replacing it with breast milk.
The transition from artificial feeding to natural feeding should be gradual.
Stagnation
During the operation, the water balance in the woman’s body is disrupted, and she needs to drink plenty of fluids. But excessive water consumption provokes increased lactation, the breasts swell, the milk ducts become clogged - stagnation occurs. When you are in the room with your baby, you need to apply it to the glands as often as possible; over time, lactation will stabilize and the blockage will go away.
When the baby is separated from the mother, ordinary lactostasis will turn into mastitis, so you need to pump every 1.5-2 hours before starting regular breastfeeding. Massage procedures are useful, and health workers will teach you how to express properly after kneading the hardened gland.
To establish breastfeeding after a caesarean section, it is important to put the baby to the breast as early as possible. Even a few drops of colostrum will trigger the production of antibodies, populate the baby’s intestines with beneficial flora, and activate the immune system. Feeding should be done on demand to ensure stimulation of lactation.
The procedure should not cause pain or discomfort. It is better to ask the midwife to be present at the first sessions to learn how to pump correctly.
Correct posture is very important for full lactation and resorption of lumps if they have formed in the mammary gland. The best option after a caesarean section is to hand feed to relieve pressure on the abdomen. The baby's chin should point towards stagnation if lactation is intense. During attachment, the baby should grasp most of the areola so as not to damage the nipple and not provoke the development of mastitis.
Breast massage
How to increase the lactation of a nursing mother after a cesarean section using breast massage? The procedure is carried out immediately before latching - this will facilitate the outflow of milk, help the baby to attach to the breast more easily and suck out more liquid.
The massage is carried out by supporting the breast with one hand, and with the other making smooth movements from the periphery to the nipple. Before the session, you can slightly warm up the gland by applying a warm towel - this will enhance lactation.
Breast milk is, from all points of view, a food that is ideal for a baby. The composition of this product has no analogues, so there is no complete replacement for human milk. It is not surprising that every loving mother would like to give her child as much as possible useful and necessary for growth and development. Therefore, the issue of lactation after childbirth and after cesarean section is most acute.
After a physiological birth, when the baby is born according to all the laws of nature, the woman’s hormonal background fully corresponds to the baby’s new needs, milk comes in much faster than after surgery. They try to perform a caesarean section before labor begins, which means that the woman’s mammary glands are not yet ready to feed the baby. But the closer to the date of birth the operation is scheduled, the fewer problems there will be with lactation.
Operative childbirth disrupts the natural endocrine chain, in which first the mammary glands mature for almost a full nine months, and then oxytocin and prolactin begin to be produced, which stimulate milk production. First, colostrum is secreted, for many even before birth, and only a few days after the birth of the child, colostrum turns first into a transitional form of milk, and then into full-fledged breast milk.
On average, milk appears on the third day after birth. But in the case of surgical delivery, various options are possible. One woman will have milk on the second day, while another will only appear on the fifth. There is no need to despair. Lactation can be improved even in the most difficult cases, when a cesarean section was performed for urgent medical reasons long before the expected date of birth.
Scientists have long proven that the amount of breast milk directly depends on the frequency of the baby’s attachment to the breast. It is better to do this immediately after birth - this way lactation will normalize faster.
What do doctors think?
Member of the ILCA multilingual committee, lactation consultant with international certification IBCLC Irina Ryukhova: “If a woman has had a caesarean section, some difficulties may arise with breastfeeding a newborn. In such cases, it is imperative to enlist the help of specialists. Problems, as a rule, lie in insufficient milk production and the reluctance of the baby to latch on to the breast. A young mother should not worry in such situations - this will only worsen the overall picture. There is nothing wrong with supplementing the baby with formula while breastfeeding until lactation improves and the baby’s reflexes return to normal.”
Physiology of the process
Why doesn't milk come in after a caesarean section? Doctors explain it this way: according to nature’s plans, everything that happens to our body is closely intertwined. Especially when it comes to bearing and giving birth to a baby. Therefore, breastfeeding after cesarean section is a pressing issue for many. In the normal course of events, childbirth triggers the production of special hormones that stimulate lactation. In a situation where a child is born as a result of a caesarean section, the “beacons” are confused. Endorphins, whose role is to alleviate pain during contractions and help the body produce prolactin (milk hormone), do not “signal” to the body that it is time to feed the child.
In addition, there is another hormone that is of great importance - oxytocin. It is he who “contracts” the uterus during childbirth and causes a rush of milk after. Is the body of mothers who have given birth without giving birth capable of producing oxytocin in the required quantity? It is logical that those who gave birth naturally will have more intense hormonal work.
In order for everything to go as it should, experts recommend not giving the baby anything to drink or feeding until the first breast milk. This can be done within six hours after the baby is born.
If the circumstances are such that the child or mother is, for example, in the intensive care unit, you should not worry about breastfeeding and constantly torment yourself with the question “When does milk come after a cesarean section?” Of course, you will have to retrain, but this is not a problem. Especially if milk is expressed every 2 - 3 hours, and it is this, and not formula, that the baby is fed.
Don't forget to pump at night. At this time of day, prolactin (the hormone responsible for the amount of milk) is especially actively produced. Give this time to recovery. Learn the correct pumping technique, and everything will be fine once both you and your baby are strong enough.
Characteristics of lactation after cesarean section
Most women are sure that breastfeeding is generally impossible after a CS. Obstetricians and gynecologists, in turn, dispute this opinion.
Let's look at how the whole process works. During the operation, a woman’s body experiences enormous stress. Of course, this affects lactation. The special hormone prolactin is responsible for the amount of milk. A woman needs to do everything that he has worked out as much as possible.
How does the process of milk production develop after a CS? The entire period can be divided into several stages:
- Colostrum release. Many people think that there is nothing useful in it. But that's not true. A few drops of colostrum are enough for a newborn to get enough. The liquid is rich in vitamins and minerals. Protects the baby from infections and improves immunity.
- Transitional milk. Released on days 3–6. It has a bluish tint, almost transparent.
- Full lactation process (7–9 days). By this time, the milk is already quite fatty and light yellow in color.
To improve the lactation process, you need to feed your baby often. Forget about feeding by the hour, this practice has long been unwelcome in medicine.
Lactation and caesarean section
As we have already found out, breast milk does not disappear during artificial birth. The main problem is that a child during a caesarean section may not be with his mother in the first minutes. Therefore, the first thing you need to do is take the baby in your arms as often as possible and establish contact with him. This will help the hormone prolactin increase the amount of milk in the mother's breasts.
The second step is to teach your baby to breastfeed. Most likely, in the postoperative period, the nurse fed the baby formula, and the child got used to immediately receiving milk from the nipple. Therefore, you will have to teach him to strain himself and get his mother’s milk. You know that breast milk does not come in full immediately and you need to spend 30 to 50 minutes feeding.
If for some reason you lose milk, do not think that it is due to artificial birth. Many women often produce little milk after giving birth. This is influenced by several factors such as: postpartum depression, unhealthy and insufficient nutrition, lack of sleep and so on. Having eliminated these factors, milk appears again - the main thing is not to panic.
An important point is to take painkillers after childbirth. Some of them are completely incompatible with breastfeeding. Therefore, be sure to discuss the subsequent recovery and feeding of the baby with your attending gynecologist. He will prescribe you homeopathic remedies, exclusively based on natural ingredients.