Why does gestational diabetes develop during pregnancy?
Pregnancy is a period of hormonal changes in the mother's body. The placenta secretes substances that block the effects of insulin. This is how hormones help prevent blood sugar levels from falling.
As pregnancy progresses, substances produced by the placenta impair glucose tolerance. Blood sugar levels rise. The body begins to produce more insulin to reduce the amount of glucose and help it get into the cells. Gestational diabetes develops in pregnant women.
As a rule, the pancreas produces three times more insulin during pregnancy. This suppresses the effect of hormones on sugar levels. If the pancreas cannot cope with the effect of the increasing concentration of pregnancy hormones, the mother’s blood sugar level rises.
Diagnostics
According to the standard monitoring scheme for patients, in the period from 22 to 28 weeks (it is then that the female body’s need for insulin increases significantly, on average up to 75 percent of the usual norm), a glucose tolerance test is performed. For this analysis, blood is first collected from a finger on an empty stomach in the morning. It should be noted that twelve hours before the test, you must refrain from eating, any medications not approved by the doctor, and also avoid physical/emotional stress, refrain from alcohol and smoking.
After collecting capillary blood according to the above scheme, the fair sex is given an oral dose of glucose equivalent to 75 grams, after which an hour and two hours later the second and third capillary blood sampling is done.
The norms of the above test are: on an empty stomach no more than 5.1 mmol/l, an hour after oral administration of glucose no more than 10 mmol/l, after 2 hours no more than 8.5 mmol/l. As a rule, fasting test values in pregnant women with GDM are even lower than normal, but during exercise they are significantly higher.
Unlike classic diabetes mellitus types 1 and 2, a test for glycated hemoglobin is not performed when gestational diabetes is suspected, since it is often false negative due to the peculiarities of the formation of temporary GDM in women.
In addition to this analysis, to confirm the diagnosis, the doctor must exclude other diseases that cause hyperglycemia, and, if necessary, prescribe alternative forms of research.
How dangerous is the disease for a child?
Possible complications for the fetus:
- various developmental defects (the child in the womb receives glucose, but feels a lack of insulin, and he does not yet have his own pancreas in the first trimester);
- elevated sugar levels interfere with the normal development of organs and systems, causing a lack of energy;
- The pancreas, which appears in the child in the second trimester, begins to work for two (trying to normalize the glucose level in the body of the baby and the mother); as a result, a large amount of insulin is produced and hyperinsulinemia develops, which can lead to a hypoglycemic state in the newborn and the development of asphyxia;
- excess glucose accumulates and is converted into fat; a large fetus has a high risk of damage to the humerus during childbirth;
- Excessive amounts of insulin can lower sugar levels, which is also dangerous for the baby (brain nutrition is disrupted, there is a high risk of mental disorders, respiratory disorders, obesity and diabetes in the future).
Consequences for the expectant mother and child
Mycelix - for diabetes. Hurry up to get it for free! More details
Northern Lights - diabetes prevention (consultation) More details
Gestational diabetes is dangerous for both mother and baby. A woman with this disease may have:
- Spontaneous abortions
- Late toxicosis,
- Polyhydramnios,
- The occurrence of ketoacidosis, preeclampsia,
- Exacerbation of diseases of the kidneys, nervous system, blood vessels, heart,
- Manifestation of a full-blown disease after childbirth.
Hyperglycemia in pregnant women has the ability to be transmitted to the developing fetus. Excess glucose stores are transformed into fat cells, which leads to complications during childbirth.
Expert opinion
Guseva Yulia Alexandrova
Specialized endocrinologist
Ask a Question
When a baby is born, the pancreas intensively produces insulin in order to evacuate the glucose that came from the mother to the fetus during pregnancy. When a blood test is performed, such a child will have low blood sugar levels.
At first, babies may have problems with the respiratory tract; in the future, they often face obesity or type 2 diabetes. The child’s condition is assessed using a biophysical profile, which is carried out at least once a week. It includes:
- non-stress test (heart response to movement);
- volume of amniotic fluid;
- fetal tone;
- physical activity;
- maturity of the placenta;
- breathing movements;
If indicators of GDM in pregnant women are confirmed, doctors begin careful monitoring of the condition and development of the fetus, evaluate the situation in points, draw conclusions and prescribe an appropriate regimen or treatment.
Newborn children are most often susceptible to this in those mothers who are diagnosed with pregestational diabetes (previously identified, of one form or another). In cases where they are diagnosed with gestational diabetes, this happens less frequently, but in order to protect themselves, the patient should follow all the doctor’s instructions.
What are the dangers of gestational diabetes mellitus during pregnancy for the mother?
Possible complications for the expectant mother:
- disruption of the normal course of pregnancy;
- the development of gestosis, in which a malfunction of various systems occurs, especially the vascular system;
- polyhydramnios;
- frozen pregnancy;
- genital tract infections that are dangerous to the fetus;
- ketoacidosis, in which the entire body is poisoned;
- diseases of the organs of vision and kidneys.
All risks and complications can be prevented by normalizing sugar levels.
What causes gestational diabetes
This disease is more likely to occur in women with:
- extra pounds;
- carbohydrate metabolism disorders;
- diseases of the cardiovascular system;
- severe toxicosis;
- carrying twins or triplets;
- GDM in previous pregnancies.
The age of the expectant mother also influences the development of the disease. Most often it occurs in women giving birth over 30 years of age. The cause of the pathology can also be diabetes in one of the parents.
The birth of a previous child can also influence the formation of pathology. The fetus could be overweight or stillborn.
Chronic miscarriage from previous pregnancies may also be affected.
Who can get sick?
As mentioned above, the percentage of development of gestational diabetes in pregnant women is not very high. The following factors increase the risk:
- excess weight before pregnancy (more than twenty percent of normal body weight);
- belonging to “dark” races (African Americans, Latin Americans, Asians, Native Americans);
- diabetes mellitus in close relatives;
- gestational diabetes in a previous pregnancy;
- the birth of a previous child with a large weight (more than four kilograms);
- stillbirth;
- chronic miscarriage;
- impaired glucose tolerance (sugar levels are high, but not high enough to diagnose diabetes);
- polyhydramnios.
Gestational diabetes can develop in the absence of known factors.
Consequences of GDM during pregnancy
The main danger of the disease is that the fruit is too large.
It can be from 4.5 to 6 kilograms. This can lead to a difficult birth that may require a caesarean section. Large children have an increased risk of obesity later in life.
Even more dangerous consequences of diabetes in pregnant women include an increased risk of developing preeclampsia.
This complication is characterized by high blood pressure, large amounts of protein in the urine, and swelling.
All this poses a threat to the life of mother and child. Sometimes doctors have to induce premature labor.
If the fetus is overweight, breathing problems may develop and muscle tone decreases. The sucking reflex is also suppressed, swelling and jaundice appear.
This condition is called diabetic fetopathy. It can lead in the future to heart failure and retardation in mental and physical development.
How does the disease manifest?
Symptoms of gestational diabetes mellitus may be absent for a long time. Sometimes the following symptoms are observed:
- slight thirst;
- increased appetite while maintaining or decreasing body weight;
- severe fatigue;
- increased volume of urine, frequent urge.
Women do not pay attention to these manifestations, attributing everything to their pregnant condition. We recommend that you tell your doctor about any unpleasant sensations.
During pregnancy, blood and urine tests for sugar are taken more than once. If its level is higher than normal, additional diagnosis of gestational diabetes mellitus may be performed.
First, take sugar on an empty stomach. After an hour, you need to drink fifty grams of glucose. Wait half an hour. After which a blood sample will be taken from the vein again. To confirm the diagnosis, the test is repeated after two weeks.
The following indications indicate a pathological condition:
- fasting sugar values – above 5.8 mmol/l;
- an hour after drinking glucose – above 10.0 mmol/l;
- after two hours – more than 8.0 mmol/l.
Diagnosis of GDM during pregnancy
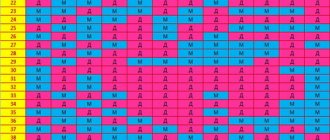
The first step in diagnosing gestational diabetes is to assess the risk of its development. When registering a woman with the antenatal clinic, a number of indicators are assessed, for example, the age and weight of the pregnant woman, obstetric history (presence of gestational diabetes during previous pregnancies, birth of children weighing more than 4 kg, stillbirth, etc.), family history (presence of diabetes in relatives) and so on. The following table is filled in:
| Options | High risk | Moderate risk | Low risk |
| Woman's age over 30 | Not really | Yes | Less than 30 |
| Type 2 diabetes in close relatives | Yes | No | No |
| History of GDM | Yes | No | No |
| Impaired glucose tolerance | Yes | No | No |
| Glucosuria during previous or current pregnancy | Yes | Not really | No |
| History of hydramnios and large fetus | Not really | Yes | No |
| Birth of a child weighing more than 4000 g or history of stillbirth | Not really | Yes | No |
| Rapid weight gain during this pregnancy | Not really | Yes | No |
| Overweight (> 20% of ideal) | Yes | Yes | No |
Let us pay attention to the parameter “Birth of a child weighing more than 4 kg”. It is no coincidence that it is included in the assessment of the risk of developing gestational diabetes. The birth of such a baby may indicate the development of both true and gestational diabetes in the future. Therefore, in the future, the moment of conception must be planned and constantly monitored blood sugar levels.
Having determined the risk of developing diabetes mellitus, the doctor chooses management tactics.
The second step is to draw blood to determine your sugar level, which should be done several times during your pregnancy. If at least once the glucose level exceeds 5 mmol/l, further examination is carried out, namely a glucose tolerance test.
When is a test considered positive? When performing a test with a load of 50 g of glucose, the glycemic level is assessed on an empty stomach and after 1 hour. If fasting glucose exceeds 5.3 mmol/l, and after 1 hour the value is higher than 7.8 mmol/l, then a test with 100 g of glucose is necessary.
The diagnosis of gestational diabetes mellitus is made if fasting glucose is more than 5.3 mmol/l, after 1 hour - above 10.0 mmol/l, after 2 hours - above 8.6 mmol/l, after 3 hours - above 7.8 mmol/l. Important: an increase in just one of the indicators does not provide grounds for making a diagnosis. In this case, the test must be repeated again after 2 weeks. Thus, an increase in 2 or more indicators indicates diabetes.
Test rules:
- 3 days before the examination, the pregnant woman eats her usual diet and adheres to her usual physical activity
- The test is performed in the morning on an empty stomach (after an overnight fast of at least 8 hours).
- After taking a blood sample on an empty stomach, the patient should drink a glucose solution within 5 minutes, consisting of 75 grams of dry glucose dissolved in 250-300 ml of water. A repeat blood sample to determine blood sugar levels is taken 2 hours after the glucose load.
Normal glycemic values:
- fasting glucose - 3.3-5.5 mmol/l;
- glycemia before meals (basal) 3.6-6.7 mmol/l;
- glycemia 2 hours after eating 5.0-7.8 mmol/l;
- glycemia before going to bed 4.5-5.8 mmol/l;
- glycemia at 3.00 5.0-5.5 mmol/l.
If the test results are normal, the test is repeated at 24-28 weeks of pregnancy, when hormonal levels change. At earlier stages, GDM is often not detected, and diagnosis after 28 weeks does not always prevent the development of complications in the fetus.
However, pregnant women face more than just high blood sugar levels. Sometimes a blood test “shows” hypoglycemia—low blood sugar. Most often, hypoglycemia develops during fasting. During pregnancy, the consumption of glucose by cells increases and therefore long breaks between meals should not be allowed and in no case should you “go on” a diet aimed at losing weight. Also, sometimes in tests you can find borderline values, which always indicate a higher risk of developing the disease, so it is necessary to strictly monitor blood counts, adhere to the doctor’s recommendations and follow the diet prescribed by a specialist.
How is gestational diabetes treated?
Often, a diet for pregnant women with gestational diabetes is sufficient to normalize nutrition. Its main provisions:
- preservation of the energy value of food;
- frequent meals in small portions (breakfast, lunch and dinner plus two or three snacks);
- refusal of “light” carbohydrates (baked goods, sweets, sugar);
- limiting fatty foods (fish and fatty meats, cream, butter), which in conditions of lack of insulin can provoke poisoning of the body;
- daily consumption of foods high in fiber (greens, vegetables, fruits, except grapes, bananas, melons).
In the daily diet, the necessary nutrients should be distributed as follows:
- 50% - carbohydrates;
- 20% - for proteins;
- 30% - for fats.
If nutrition does not help with gestational diabetes, insulin therapy is prescribed. After childbirth, there is no need for treatment.
Treatment and diet for gestational diabetes in pregnant women
In some cases, nutrition and dieting are already powerful tools in the treatment of gestational diabetes. During pregnancy, all tablet medications are contraindicated, so the only way to lower blood sugar, besides diet, is insulin injections.
But in most cases, it is possible to do without it only by properly adjusting your diet, creating a rational menu, and also increasing feasible physical activity in the form of walking, for example.
Only a few are prescribed insulin and only in two cases:
- failure to achieve target glycemic values within 1-2 weeks with diet alone
- presence of signs of fetal distress according to ultrasound data
Management of pregnancy with gestational diabetes is no different from management of pregnancy and childbirth in women with diabetes. I won’t repeat myself here; you can easily find out by reading the article “Can you get pregnant with diabetes?” .
What is the diet and nutrition of a woman with diabetes?
While a low-carbohydrate diet is an effective method to normalize blood sugar in a non-pregnant woman, this method is not suitable for a pregnant woman.
Such a woman should not completely deprive herself of carbohydrates, as this will lead to the formation of ketone bodies, which can negatively affect the development of the fetus. But there are still some restrictions. These restrictions are imposed on carbohydrates with a high glycemic index, namely any sweets, bread and flour, potatoes, cereals, sweet fruits (banana, persimmon, grapes).
What can you eat if you have gestational diabetes during pregnancy?
All types of meat and fish, any vegetables except potatoes, whole grains, seasonal local fruits and berries, nuts, mushrooms, and herbs are allowed. Maintain the following protein/fat/carbohydrate ratio. It is important to get high-quality proteins and healthy fats, both plant and animal in equal proportions.
- proteins 30 – 25%
- fats 30%
- carbohydrates 40 – 45%
Various cooking sites offer many recipes and menus, so I won’t go into more details. In addition, it is not always possible to satisfy the tastes of an audience of thousands of blog readers.
What should a pregnant woman's sugar level be (normal)
How do you know if you're doing everything right? Frequent monitoring of blood glucose will help you with this. Be sure to check your blood sugar before each meal, as well as 1 hour after eating; after 2 hours you don’t have to check it. If necessary, you will have to check your sugar at night at 2-3 o'clock.
- fasting sugar should be less than 5.1 mmol/l
- 1 hour after eating should not exceed the level of 7.0 mmol/l
- before going to bed and at night, sugar should be no more than 5.1 mmol/l
- the level of glycated hemoglobin should not be more than 6.0%
What procedures are required for such a diagnosis?
If a pregnant woman is diagnosed with gestational diabetes, she needs to:
- monitor your sugar level four times a day (on an empty stomach, two hours after each meal; sometimes you have to monitor your sugar before each meal);
- control the appearance of ketone bodies in the urine (they should not be there; if these acids appear, then sugar in the body is not controlled, poisoning occurs);
- follow a diet, distributing calories evenly throughout the day;
- perform physical exercises (as agreed with the doctor);
- control weight and blood pressure;
- if necessary, administer insulin.
Treatment
The main thing in the treatment process for pregnant women is careful monitoring, which will identify any pathology at an early stage. Therefore, it is best to register in advance, otherwise the birth may not go as planned. Blood tests should be taken at least once a month.
After identifying the problem, when the indicators are already known, the woman should carefully monitor them, at least 4-5 times a day. It is also necessary to monitor your blood pressure.
Particular attention should be paid to the diet for a pregnant woman:
- Meals should be fractional and low-calorie, approximately 25-35 calories per kilogram of a woman’s weight.
- The table must be balanced, contain a large amount of proteins, carbohydrates and even fats, as well as vitamins and microelements, otherwise the fetus will not be able to develop well and in a timely manner.
- Preference should be given to foods high in fiber.
- Fried and fatty foods and foods with easily digestible carbohydrates should be avoided.
- You need to drink at least one and a half liters of clean water per day.
Taking medications that lower blood glucose levels is contraindicated during pregnancy. If the diet prescribed by the doctor, along with moderate physical activity, does not produce the expected results, you will have to resort to insulin injections.
How to prevent the disease?
Possible preventive measures:
- limiting or completely avoiding refined sugar, honey, sweets and other “light” carbohydrates;
- limiting fatty foods and salt;
- control over your weight (if you are overweight, you need to normalize it before pregnancy);
- moderate physical activity (morning exercises, outdoor exercise, jogging, swimming, cycling, active walking);
- rejection of bad habits.
How to treat diabetes during pregnancy
Treatment for pregnant diabetics includes a special diabetic diet. This diet is not intended for weight loss, but to normalize blood glucose levels. Therefore, it should contain all the necessary nutrients, but certain foods should be limited, including:
- sweet drinks and juices;
- sweetened yoghurts and homogenized cheese;
- full-fat milk and cheese, cream;
- sweetened bread (such as challah);
- simple sugars: sugar, jams, honey;
- alcoholic drinks;
- fat meat.
When diagnosed with gestational diabetes, the menu should contain three main meals and three snacks, which should be consumed at regular intervals. Don't forget about eating before bed - it should protect a woman from hypoglycemia (low blood glucose levels) at night. It is important that food contains an appropriate amount of carbohydrates, that is, foods that contain about 10 g of digestible carbohydrates. A nutritionist will help you organize an accurate diet.
Self-monitoring of blood glucose levels (using glucose meters, widely available in pharmacies and medical stores), as well as glucose and ketone particles in morning urine (using test strips), also plays an important role in the treatment of gestational diabetes.
When treating gestational diabetes, regular physical activity (such as walking) is also recommended, which reduces insulin resistance, that is, increases insulin sensitivity. Before undertaking any physical effort during pregnancy, you should consult a gynecologist to rule out any contraindications.
If the diet used does not lead to a decrease in blood glucose levels, it is recommended to begin insulin therapy. Small doses of insulin are used that do not have a negative effect on the developing fetus.
Any woman diagnosed with carbohydrate disorders should be under the constant supervision of a diabetes specialist.
Controlling Gestational Diabetes
A woman should systematically keep a special diary in which she should note her sugar level and the number of insulin doses each time, and additionally carefully record all meals and snacks. You should also take into account the so-called carbohydrate exchangers, also known as bread units. This is the equivalent of 10 g of carbohydrates absorbed by the body (starch, sucrose, lactose). Not only a proper diet is important, but also physical exercise, which improves the burning of glucose, reduces insulin resistance of tissues and increases their sensitivity to insulin. Therefore, if the expectant mother feels well and there are no other contraindications, the doctor recommends special exercises to speed up the metabolism.
Frequent medical examinations
Pregnant women with diabetes are more likely than healthy women to see their doctor to monitor their baby's condition. How often? From diagnosis of diabetes to 34 weeks of pregnancy every two weeks, after 36 weeks weekly. During such an examination, the doctor evaluates, among other things, the baby's size and listens to his heartbeat using a camera. If necessary, additional assessment of the biophysical profile of the fetus is carried out. All this is necessary to prevent the death of the child (a decade ago, pregnant women with diabetes often gave birth to stillbirths). If the fetal assessment is successful and blood sugar control is positive, you can carry the baby to term until vaginal labor begins. In this case, there are also no contraindications to natural birth. However, such births must take place in a specialized hospital.