Treatment of acute otitis media in children in ENT clinic No. 1
Author:
- Khirnetkina Ayuna Fedorovna
otolaryngologist, otoneurologist, audiologist
Acute otitis media is an acute disease of the middle ear. Accounts for approximately 25-40% of all ear diseases.
Inflammatory diseases of the middle ear occur in all age groups. This disease develops especially often in children, with the peak incidence occurring between 6 and 18 months; Before the age of three, 90% of children experience acute inflammation of the middle ear at least once. Timely diagnosis and adequate treatment of otitis media are extremely important to prevent possible adverse consequences, the most difficult of which are meningitis, death, and the development of hearing loss, which can subsequently lead to mental retardation.
Reasons for the development of the disease
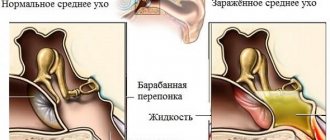
The main reason for the development of serous otitis is a runny nose, which can be associated both with the presence of a viral infection and with adenoids (in children). Since the hearing organs are directly connected to the nasopharynx, the Eustachian tube (which connects the cavity of the middle ear to the pharynx) with a runny nose can become overfilled with mucous secretions and stop performing its functions. In this case, the fluid accumulates in the middle ear cavity, cannot leave naturally and becomes a cause of inflammation.
Another reason is pathology of the eustachian tube itself. Disturbances in the passage of air in the Eustachian tube are often accompanied by the development and proliferation of pathogenic microflora.
Prevention
Prevention of otitis in young children includes the following measures and recommendations:
- Regular hearing hygiene. Parents should not clean their children's ears with improvised means or allow deep penetration into the ear canal.
- After swimming in the pool or bath, children need to blot the water from the ear canal.
- Babies under 1 year old should not be in a draft without a hat covering their ears.
- It is important to promptly and fully treat diseases of the ENT organs. Bilateral otitis in children is often the result of a runny nose.
What happens with serous otitis: stages of disease development
- Initial stage. Not accompanied by symptoms. The patency of the auditory (Eustachian) tube is impaired. In children it occurs asymptomatically; the second stage, acute pain, is immediately diagnosed.
- Second stage. In 4-7 days. Ear congestion and pain appear.
- Third stage. Fluid appears behind the eardrum. It begins to put more pressure on the membrane and cause more pronounced pain.
- Fourth stage. If treatment is not prescribed, the fluid may turn into pus, which has a more pronounced inflammatory effect. In children, intracranial complications such as meningitis and brain abscess sometimes occur.
Causes of illness in infants
In addition to the standard factors that provoke inflammation in the ear canal, pathological childbirth, trauma received during delivery, prematurity, infection of the fetus during the birth canal of a woman suffering from one of the sexually transmitted infections can lead to otitis in children in the first days of life.
Additional reasons leading to otitis media in children of the first year of life include:
- Anatomical features
- Teeth growth
- Poor hygiene of the nasal passages
- Poor indoor hygiene (dry air, tobacco smoke)
- Allergies
- Artificial feeding
- Avitaminosis
- Temperature violation
- Illiterate antibiotic therapy
- Poor nutrition
The Eustachian tube of a newborn has anatomical features that contribute to the development of inflammation (it is wider and shorter). It is located almost horizontally. This means that the free outflow of fluid is difficult; the mucous membrane of the tube is covered with a substrate, which pathogenic bacteria gladly use as a nutrient medium. Even without additional factors, a combination of anatomical features contributes to the development of inflammatory processes in the baby’s ear canal.
Otitis media in an infant can be caused by the mother's inability to put the baby to the breast or errors in feeding the baby from a bottle. If a child often chokes, the likelihood of reflux of the pharyngeal contents along the tubal route increases. Leftover milk and formula are an excellent environment for bacteria to multiply. As the pyogenic flora multiplies, it leads to the accumulation of significant amounts of exudate, which puts pressure on the eardrum, causing pain to the baby.
The growth of teeth in a child of the first year of life causes swelling of the oral mucosa and impaired nasal breathing. This process is often accompanied by allergies and an increased incidence of respiratory diseases . This provokes inflammatory processes in the ear. Children suffering from any type of allergies are more likely to suffer from otitis media .
An insufficiently ventilated room and lack of wet cleaning can lead to swelling of the mucous membrane of the child’s respiratory tract, impaired nasal breathing and become a factor contributing to the development of a pathological process in the middle ear.
In children over one year old, especially those with a labile nervous system and prone to crying, inflammation of the middle ear mucosa can be triggered by constant whimpering and screaming. In children 1–3 years of age, inflammation of the middle ear can be provoked by constant crying, frequent acute respiratory viral infections and childhood diseases, damage to the eardrum, and adenoids. Since children from 1.5–3 years old often go to kindergarten, at this age their mothers no longer feed them breast milk, which provides immunity . Therefore, children begin to actively suffer from childhood infections (measles, scarlet fever, ARVI), which can cause the described illness.
At the age of 1.5–3 years, children, especially organized ones, begin to spend their leisure time together. This is very useful, but it means that ear injuries are possible (being hit by a ball or other object), a foreign object getting into the ear canal, attempts to independently care for the ears (children may try to repeat the actions of their parents and use ear sticks, and not necessarily clean ones if adults were not vigilant enough). All these mechanical damages contribute to inflammatory processes in the ear.
Treatment of serous otitis in children and adults
In children, the development of the disease occurs very quickly, so if a child experiences pain in the ear, be sure to immediately show it to a doctor - a pediatrician or otolaryngologist.
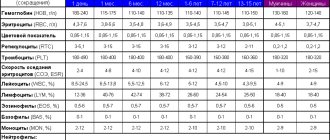
Children under 1 year of age with serous otitis must be prescribed antibacterial therapy (antibiotics), regardless of whether there is intoxication, high fever, or abnormalities in the clinical blood test. This is due to the peculiarities of the child’s anatomy, the speed of the inflammatory process, which can move to another stage within an hour.
Otitis in adults does not always require treatment with antibiotics. Serous (catarrhal) otitis media in adults can be treated with ear and nasal drops. During the period of illness, flights are not recommended due to pressure changes, which can negatively affect the condition of the eardrum.
Depending on the stage of otitis and the age of the patient, treatment can be conservative (medicinal) and surgical.
Drug treatment includes:
- treatment of the nasopharynx to relieve the auditory tube, relieve swelling;
- sometimes local drops in the ear are prescribed;
- if antibacterial therapy is prescribed, ear drops are usually no longer necessary;
- you can add gymnastics for the auditory tube, chewing gum, blowing, etc.
If conservative treatment is not effective in a child, namely, intoxication, pain persists, and fluid remains in the ear, surgical treatment is used.
In children, we can observe the presence of fluid and treat it conservatively for 1-1.5 months. During this time, the liquid will not thicken and will not interfere with the movement of the auditory ossicles that are located in the ear.
The operation consists of puncturing the eardrum under a microscope and installing drainage - a shunt or tube. They are silicone and allow fluid to drain out of the middle ear. The essence of the treatment is to allow air to appear in the ear cavity so that the child does not experience hearing loss. The tubes remain in the ear for varying periods of time - from one month to a year, and even longer. Sometimes they fall out on their own when the inflammation goes away and ear function is restored. Or we take them out after a while ourselves.
Indications for antibiotic therapy
The drugs of choice (depending on the condition, the nature of previous therapy, the presence of allergies to drugs) are penicillin antibiotics. Antibiotic dosing is carried out according to the severity of the process and the child’s weight. The duration of antibacterial therapy depends on the severity, nature of the disease, and timing of initiation of treatment.
In most cases, acute otitis media in children ends in recovery. The average recovery time is 2-3 weeks. Recovery involves restoration of general condition, otoscopic picture and complete restoration of hearing.
Unfortunately, neither parents nor doctors always pay attention to the latter circumstance. Therefore, every child who has suffered acute otitis media should be examined by a specialist for a control hearing test. According to various sources, about 20% of children then suffer from hearing loss after untimely and inadequate treatment.
Clinical picture of otitis media
Symptoms of purulent otitis are pronounced and acute. There is severe pain, which becomes more intense at night. In addition, children usually experience:
- purulent discharge from the auricle, sometimes mixed with blood;
The ears fester only after the eardrum is perforated; before this, exudate is not released.
- sharp shooting or throbbing pain;
- congestion and significant hearing loss;
- increase in body temperature to 38-39°;
- weakness and general malaise.
Based on the child's complaints, a disease can be suspected. But with infants the situation is more complicated. Recognizing otitis, especially in the initial stage, is not easy. Parents need to pay attention to the following signs:
- pale skin;
- constant reasonless crying and moodiness;
- attempts to touch the sore ear or lie on its side;
- refusal to eat;
- restless sleep and insomnia.
You can check suspicions of otitis yourself by gently pressing on the tragus - the pain will intensify significantly, the child will react by crying. No further manipulations can be carried out; diagnosis and treatment must be carried out by a doctor.
How to prevent the development of the disease
It is possible to prevent the development of pathology in a baby; for this it is necessary:
- Breastfeed your baby for as long as possible. Experts have proven that artificially educated children are most susceptible to the development of pathology.
- Limit your baby's contact with various allergens.
- Avoid contact with sick children.
- Treat colds in a timely manner.
- Pay attention to the correct procedure of blowing your nose.
- Taking vitamins and immunostimulants.
- For preventive purposes, visit an otolaryngologist.
This is a fairly serious disease, so efforts should be directed toward preventing otitis media in children.
Diagnosis of hearing loss
Hearing restoration is carried out by a doctor - an otorhinolaryngologist. At the first appointment, the doctor will examine the child, ask the parents what symptoms appear in everyday life, and whether the adenoids are bothering them. Then the examination is carried out using several methods:
- audiometric examination - to determine hearing acuity;
- tympanometry - using a tympanometer to study the functions of the elements of the middle ear, as well as the mobility of the eardrum;
- tuning fork research - carried out using special tuning forks;
- studies of evoked potentials - carried out on young children during sleep, if it is impossible to carry out the above studies;
- Ottoacoustic emission - the auditory nerve is stimulated with electrical impulses to test its response;
- if necessary, additional x-ray examinations are prescribed (CT-temporal bones, MRI of the brain, x-ray examination of the temporal bones according to Schüller, Mayer, Stenvers).
Causes of pathology
ENT organs are in close proximity to each other. Harmful microorganisms easily migrate from one part of the system to another, which leads to the spread of infection. The origin of purulent otitis media in most cases is of this nature.
Suppuration of the ear in children occurs against the background of:
- ARVI;
- flu;
- tonsillitis;
- rhinitis;
- inflammation of the adenoids;
- catarrhal otitis.
The main risk factor is untreated respiratory viral infections. They are accompanied by a significant secretion of mucus containing a large number of bacteria. When sneezing, coughing and especially blowing your nose, it enters the auditory tube and causes inflammation.
“I always warn parents at appointments that they need to blow their noses of mucus accumulated in the nose correctly. You cannot close both nostrils at the same time - this creates increased pressure in the tympanic cavity and disrupts ventilation. As a result, the exudate is thrown into the middle ear and leads to suppuration.”
Lina Dementieva, pediatric ENT
Unfavorable factors also contribute to the appearance of purulent otitis:
- hypothermia;
- water getting into the ear canal;
- injury to the ear canal, in particular when using cotton swabs for cleaning;
- vitamin deficiency and immature immunity.
It is important to take into account all the reasons and protect the child as much as possible from a serious disease that causes painful symptoms.
Treatment
To identify hearing deviations from normal values, a special device is used - an audiometer. To restore hearing after otitis media, doctors use a variety of methods. The main methods include:
- Ventilation of the ear canal. In this case, blowing is done using a Politzer balloon. This design is a rubber bulb that resembles an enema. The doctor places a special tip into the ear canal, after which the child must say a certain word. At this moment the procedure is carried out.
- Rinsing the ear cavity with antiseptic substances. Using this method, it is possible to get rid of pus.
- Vibromassage of eardrums.
- Ear rinsing. This method is effective if the cause of hearing loss is excessive accumulation of sulfur. After the plugs are washed out, the child begins to hear normally.
Drug therapy
Drug therapy is usually carried out to eliminate the source of inflammation that has caused hearing loss. Most often, specialists prescribe antibacterial drugs. In some cases, the use of steroids is indicated. This allows you to avoid hearing deterioration during therapy.
Vitamin complexes help improve the prognosis and speed up the recovery process. To make treatment as effective as possible, doctors usually use several techniques.
Folk remedies
Traditional recipes cannot completely restore hearing in case of abnormalities in the elements of the hearing organ. However, with reversible damage, they are quite capable of speeding up the healing process. To do this, you can use the following tools:
- Propolis oil tincture. To make it, 50 g of propolis should be crushed and 100 g of alcohol added. Leave the product to infuse for a couple of weeks. Then you need to strain it and mix it with vegetable oil. It is recommended to moisten a tampon in the tincture and insert it into the ear. After 10 hours it needs to be replaced. The course of therapy lasts 2 weeks.
- Camphor oil and garlic. A clove of garlic should be finely chopped and mixed with 2 drops of oil. Wrap the resulting mixture in gauze and place it in the ear. After a burning sensation appears, the tampon can be pulled out. The product is used before bedtime.
- Melissa tincture. To make this remedy, the leaves of the plant must be mixed with alcohol and left to infuse for 3 days.
- Beet juice. This method is effective if the cause of hearing loss after otitis media is a chronic runny nose. To treat the disorder, you need to inject a few drops of the product into each ear.
Dr. Komarovsky about hearing loss in children after otitis media:
Surgery
If hearing impairment is caused by the formation of adhesions in the ear canal area, hard seals consisting of connecting cords must be excised surgically.
Complex perforations that cannot heal naturally should be closed with an element of the temporal fascia. A membrane made of a special polymer is applied to the medial zone of the membrane. If there is necrosis of the incus located between the stapes and the handle of the malleus, a spacer must be installed. It is pre-modeled.
Artificial materials should be used only in cases of severe destruction of the auditory ossicles. This requires complete prosthetics of the membrane, malleus, incus and stapes base.
Causes of otitis media in children
Otitis media in children is usually caused by bacteria and viruses, and allergies can also cause otitis media.
Infants and young children are more susceptible to otitis media due to the shape of the eustachian tubes, because they are more likely to have respiratory infections that often precede ear infections, because they have a weak immune system, or because they are fed in a supine position .
The Eustachian tubes in infants are shorter than in adults; they drain fluid into the nasopharynx from the ears. Inflamed adenoids can block the outflow of fluid, which can lead to otitis media.
Prevention of otitis media in children
The risk of disease can be reduced by:
- Maintain overall health through proper nutrition, adequate rest, and regular medical checkups.
- Breastfeeding for at least one year.
- Feeding in an upright position, especially when the baby has a respiratory infection.
- Elevated position during sleep when the child has a cold. The pillow should be placed under the mattress, not under the child's head.
- Vaccination against influenza and pneumococcal infection.
- Give your baby a pacifier during air travel during takeoff and landing.
- Limit the use of the pacifier during the day and be sure to take it away from the child before bed.
- Decongestants for children with colds or allergies, especially before flying. Do not bottle feed your baby during takeoff or landing, when the risk of ear damage is greatest.
- Proper cleaning of the nose, one nostril at a time.