Causes of purulent otitis media
The main factors that can trigger the occurrence and development of the disease in adults include:
- presence of adenoids;
- inflammation of the nasopharynx (rhinitis, sinusitis);
- viral infections (parainfluenza, ARVI, influenza);
- decreased immunity;
- improper ear hygiene.
There are several ways for infection to enter the eardrum cavity. Most often, it penetrates there through the auditory tube in the presence of various inflammatory diseases. The development of traumatic otitis occurs due to infection of the cavity of the tympanic membrane of the middle ear through the mastoid process or an injured tympanic membrane. Another, most rare, variant of infection is hematogenous: during diseases such as typhoid, tuberculosis, scarlet fever, measles, influenza, pathogenic bacteria enter the middle part of the hearing organ through the blood.
Very often, infants suffer from various forms of otitis, which is explained by the peculiarities of the anatomy of the child’s ear. In an infant, the auditory tube is much wider and shorter than in an adult, and is located almost horizontally. In this regard, nasopharyngeal secretions can easily pass through the open auditory tube, delivering pathogenic microorganisms to the middle ear. A slight inflammation can close the already small lumen of the auditory tube in an infant, reducing hearing and complicating the course of the disease. The result of this anatomical feature is often bilateral purulent otitis. As the baby grows, their number decreases due to the development of the hearing aid.
Home and drug treatment
Treatment of bilateral forms of otitis in children is carried out only under the full supervision of a physician. Self-treatment and the use of folk remedies without consultation with a doctor complicates the recovery process and also leads to adverse consequences (loss of proper function of the hearing aid).
When a pathological process has formed due to a cold, special agents with antiviral action are prescribed. In some cases, the provoking factor of the disease will be tonsillitis. In such a situation use:
- Ear drops. Used mainly in the initial stages of otitis media. The choice of a specific drug is influenced by the cause of the disease - Otipax, Otizol. It is not recommended to use these medications when the membrane has ruptured.
- Nasal agents that are aimed at constricting blood vessels - Nazivin, Otrivin. These drugs are necessary to eliminate swelling in the Eustachian tube. Usually, medications based on xylometazoline are prescribed.
- Antihistamines. Their effect is aimed at eliminating swelling in the nasopharynx - Suprastin, Eden, Erius. They act on the auditory tube, which is often affected during bilateral otitis media.
- Antibacterial drugs. They are used only when purulent contents have formed in the ear canal and flow out - Augmentin, Sumamed, Macropen. Acceptable for use in childhood. Antibiotics are characterized by the least toxicity, do not harm fragile immunity and do not affect general well-being.
Treatment of otitis should be comprehensive. In this regard, in addition to medications that are aimed at getting rid of the provoking factor of the disease, symptomatic medications are also prescribed. They help ease the baby's overall well-being.
When the temperature rises above 38 degrees, the specialist will prescribe the use of antipyretics (tablets and syrups). During bilateral otitis media, discomfort is pronounced. It can be eliminated with the help of analgesics and drugs that are aimed at getting rid of the inflammatory process.
Course of the disease
The course of purulent otitis usually occurs in several stages:
Pre-perforation stage. The symptoms that appear at this stage are pronounced:
- sharp increasing pain;
- decreased hearing;
- painful palpation of the mastoid process;
- temperature increase.
The perforated stage, during which, after a rupture of the eardrum, pus begins to be released, sometimes mixed with ichor. The temperature gradually drops, the ear pain subsides.
Reparative stage. After the cessation of the flow of pus and the gradual scarring of the openings of the eardrum, the patient’s hearing is restored.
Acute purulent otitis in adults lasts on average no more than 20 days. A weakened immune system or inadequate treatment may cause the development of any complication. At any stage, acute otitis media can transform into chronic purulent otitis media, which is characterized by mild symptoms.
Therapy methods
First, you will have to undergo a series of laboratory tests. This is required to determine the type of viruses that caused the pathological condition. Additionally, it will be possible to find out the reason for its appearance.
Methods for eliminating this symptom in an adult:
- Only after visiting an otolaryngologist can treatment begin.
- Allow the secretion to flow out; do not plug the ear canal with various materials (cotton swab, turunda). It is necessary to use a loosened cotton ball, it will facilitate the absorption of liquid. It is recommended to change the balls as they absorb the secretion. The more the secretion is released, the more often the cotton wool needs to be changed.
- To clean the ear, you need to use soft cotton swabs. Pre-moisten it with an antiseptic solution diluted with water in a 1:1 ratio, for example, hydrogen peroxide, Chlorhexidine or Furacilin.
- If the doctor has authorized the use of compresses, then in the absence of purulent discharge, but with the presence of liquid, you can make a compress with alcohol. It must be applied for 2 hours.
- It is allowed to use drops prescribed by a doctor. They have a warming effect. They must first be heated to body temperature (37°C).
- Antibiotics when otorrhea is caused by infectious processes: Amoxicillin, Ospamox, Clarithromycin.
- Anti-inflammatory drugs.
- For severe pain, oral analgesics are prescribed: Aspirin, Ketanov.
- Rifampicin (otorrhea) if the fluid is clear.
- will eliminate unpleasant odor in the ears.
- Diclofenac ointment will relieve pain.
Acute form of the disease
Acute purulent otitis in adults develops after a pathogenic medium enters the middle part of the ear through the auditory tube, which occurs during acute or exacerbation of chronic diseases of the ENT organs or upper respiratory tract.
The first, or catarrhal, form of otitis, which lasts from several days to 2 weeks, is characterized by the onset of an inflammatory process with the formation of exudate.
The next stage - purulent otitis - begins with a perforation of the eardrum, after which pus flows out, lasting about 6-7 days, and the subsequent subsidence of pain.
The third stage is characterized by attenuation of inflammation, reduction and cessation of suppuration, during which hearing may decrease. It can be restored gradually as the perforation of the eardrum becomes scarred.
What are the symptoms and signs of the pathology?
Suppuration is the cumulative result of the activity of infectious agents and cells of the immune system aimed at their elimination.
Purulent otitis is always difficult. Despite the approximate similarity of symptoms, variants of purulent otitis within one local area (middle, internal or external) can differ significantly from each other depending on the pathogen that caused the inflammation. If we talk about the localization of purulent otitis media, then the tympanic region of the middle ear is the leader in this regard. The greatest danger is the purulent lesion of labyrinthitis. Finally, purulent inflammation localized in the external auditory canal is the simplest type of otitis that does not require serious medical care.
There are three ways for infectious agents to enter the middle ear cavity:
- through the Eustachian tube;
- through a rupture in the eardrum;
- with blood flow.
Of these, the first option accounts for up to 98% of all infections of the tympanic cavity.
- The presence of a focus of infection in the upper respiratory tract: sinusitis, tonsillitis, scarlet fever, pharyngitis or any other disease.
- Decreased local immunity of the mucous membrane of the nasopharynx and Eustachian tube.
- A general immunodeficiency condition that can occur, for example, during chemotherapy.
Acute purulent otitis is often a consequence of chronic catarrhal otitis.
1. The most typical pain symptom in acute purulent otitis media is:
- Extremely severe pain in the depths of the ear, mainly in the evening and at night.
- Nature of pain: throbbing, shooting.
- The pain radiates to other areas of the head: to the temple, to the eye, to the back of the head, and can affect the entire half of the head.
- During the day, the nature of the pain becomes dull and less pronounced. The feeling of heaviness in the head persists.
- The pain intensifies when coughing, sneezing, or pressing on the ear.
2. Against the background of pain, such classic symptoms as hearing loss, ear congestion, noise and distortion of sounds fade into the background.
3. Feverish state. In the purulent phase, body temperature rises to 39.5°C, in children – above 40°C.
4. Suppuration. Occurs after deformation and rupture of the eardrum under the influence of pus pressure. The pain symptom at this stage is significantly reduced.
1. Antibiotics are indicated for all patients with acute purulent otitis, including children under 2 years of age, patients with diabetes, immunodeficiency and other diseases for which antibiotic therapy is contraindicated.
The following drugs are most effective:
- Tetracycline (ineffective)
- Gentamicin (toxic to the auditory system)
2. To relieve pain caused by the pressure of purulent contents on the eardrum, turundas moistened with boric acid and glycerin are placed in the ear.
In the pre-perforation stage, Otipax is used, which has anti-inflammatory and analgesic effects. The alcohol included in its composition makes it impossible to use these drops in case of open suppuration.
To reduce pain, take ibuprofen-based medications.
3. In order to restore the functionality of the auditory tube, vasoconstrictor drops and drugs that relieve local irritation (for example, Tavegil) are used.
4. The result of pus formation is ultimately a rupture of the eardrum. If this does not happen, and the pain becomes unbearable, forced perforation is indicated.
After perforation, the entire complex of drug therapy that was used at the pre-perforation stage is continued.
Significant attention is paid to ear hygiene: pus must be removed 2-3 times a day. Hydrogen peroxide is used to clean and disinfect the external auditory canal. After cleaning, Tsipromed is instilled into the ear.
Chronicity of purulent otitis media of the middle ear is a consequence of undertreatment of the acute form of the disease.
- Frequent hypothermia and respiratory diseases
- Chronic catarrhal otitis
- Anatomical features of the structure of the nose and pharynx
Since perforation of the membrane remains in the chronic stage of purulent otitis, the pain symptom, unlike the acute pre-perforation form, is not dominant. The same applies to elevated body temperature.
- Suppuration occurs with a certain frequency.
- Hearing function progressively deteriorates.
- Lack of treatment leads to additional infection of the tympanic cavity, degradation of the eardrum, auditory ossicles and complete hearing loss.
There is no special drug treatment for chronic purulent otitis media that would lead to complete recovery with stable remission.
Everyone is advised to undergo surgery to restore the integrity of the eardrum with concomitant therapy and physiotherapy.
The appearance of ulcers in the external auditory canal is associated with loss of integrity of its skin, with cracking and abrasions. Purulent otitis of the external ear occurs for the following reasons:
- Mechanical trauma to the skin of the ear canal, including during hygiene procedures.
- Dermatological diseases.
- Frequent pouring of water into the ear canal.
- Using irritating ear drops.
- Tendency to form boils.
A significant factor in the occurrence of suppuration in the outer ear is a decrease in the local immunity of the ear canal due to excessive leaching of sulfur secretion.
- Itching.
- Unpleasant sensations.
- Redness and swelling of the visible part of the ear canal.
- Slight hearing loss.
- Mild pain; the nature of the pain is dull.
- Minor purulent discharge, often in residual quantities.
In most cases, no special treatment for otitis externa is required. People carry this disease at home, can go to work, and do all the usual things.
The suppurations break out on their own as they mature. Warming alcohol compresses can be used to speed up the process.
Plants and herbal infusions are often used. For example, aloe juice has good antiseptic properties.
The purulent form of internal otitis is a consequence of the serous form, which, in turn, occurs as a complication of the inflammatory process in the middle ear.
The membrane of the oval window, separating the middle and inner sections of the ear system, due to the pressure exerted on it by pus from the tympanic cavity and serous inflammation from the labyrinthine cavity, becomes thinner and eventually loses its integrity, allowing the purulent substance to infect the labyrinthine area.
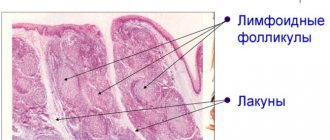
A labyrinth is not exactly an ear in the ordinary sense. It consists of two parts. In one, associated with the oval window, the resulting sound vibration is transformed into a nerve signal. The second part, the vestibular part, receives and transmits information to the brain about the position of the body in space and the direction of movement.
The functions of the labyrinth are important. This makes the symptoms of its purulent inflammation pronounced and severe:
- Involuntary jerky eye movements
- Intense pain that extends to the entire side of the head with the affected ear
- Heat
- Total hearing loss
- Noise, sound distortion
- Dizziness, nausea, vomiting
- Inability to perform coordinated movements
- Loss of balance
Drug treatment involves the use of the following drugs:
- Antibiotics (Amoxicillin, Erythromycin, etc.),
- Anti-inflammatory drugs (Diclofenac, Dicloran, etc.),
- Drugs that stabilize vestibular function (Betagistin, Bellataminal, etc.),
- Painkillers.
In especially severe cases, when the microbial environment extends beyond the labyrinth, infiltrates into the bone tissue and threatens the brain, an operation is performed to sanitize the damaged cavities.
The prognosis for treatment of purulent labyrinthitis is always negative. In most cases, there is complete hearing loss in the affected ear. The function of the vestibular analyzer is redistributed between the second labyrinth, the visual analyzer and tactile sensitivity.
A pathology such as purulent otitis media occurs mainly in childhood, and the disease often becomes recurrent. Factors contributing to the development of the disease can be very diverse: from a common runny nose to a weakened functioning of the body's protective functions.
Even the most subtle symptoms of purulent otitis in a child should be the basis for visiting a competent specialist, because this disease is very dangerous, especially in childhood. Next, we will talk about ways to identify and treat such pathology in childhood.
Purulent otitis is a disease that develops in the middle part of the human ear, namely in the tympanic cavity. This is a small space in the temporal bone that is responsible for receiving and processing incoming sounds.
With this form of the disease, inflammatory damage to the mucous membrane in the ear occurs, and the formation and accumulation of purulent masses is observed.
Reference. This disease is considered much more dangerous compared to the catarrhal form, as it can cause hearing loss and various intracranial complications.
The appearance of purulent otitis media in a child can cause problems with the formation of speech function. There are cases when such a disease causes disturbances in psycho-emotional development and difficulties in perceiving information, which significantly reduces the level of quality of life.
This type of pathology develops much more often in children than in adults. This phenomenon occurs due to the following objective reasons:
- The auditory tube in a baby has a slightly different shape and size than in an adult. It is shorter, narrower and has no curvature, which facilitates the penetration of various pathogenic bacteria into the ear cavity;
- many children have enlarged adenoids, which compress the auditory tube, thereby impairing its patency;
- children are more susceptible to frequent respiratory diseases.
In addition, there are additional factors that significantly increase the risk of developing an inflammatory process in the baby’s ear. These include:
- Hypothermia.
- Lack of vitamins.
- Liquid getting into the ears.
- Weakening of protective functions.
- Long-term use of antibiotics.
The main cause of the disease is various inflammatory processes in the nasal cavity and throat, adenoids, chronic rhinitis, respiratory diseases, and viral infections.
- Treat viral infections and nasopharyngeal diseases in a timely manner;
- Strengthen immunity;
- Carry out hygiene procedures carefully, using not a cotton swab or other hard objects to clean your ears, but a cotton swab moistened with saline solution, hydrogen peroxide or sterile oil.
Chronic form of the disease
Chronic purulent otitis media, which is an inflammatory process of the middle ear, is characterized by:
- perforated eardrum;
- recurrent flow of pus from the cavity of the hearing organ;
- decreased hearing, the loss of which can reach up to 50%.
Chronic purulent otitis media develops in cases where the patient did not treat or treated incorrectly acute purulent otitis media. It can appear as a complication of chronic sinusitis or rhinitis, as well as due to a rupture of the eardrum after an ear injury. Chronic otitis media affects one in 100 people worldwide. In almost half of all cases, the disease makes itself felt in childhood, manifesting itself even in infants. Possible intracranial complications pose a real danger not only to the health, but also to the life of the baby.
Acute otitis in adults can become chronic due to the presence of such unfavorable factors as: low resistance of the human body to infections, the presence of concomitant diseases of the respiratory tract, blood and ENT organs.
Chronic purulent otitis media, depending on the location of the perforation of the eardrum and the severity of the disease, is divided into 2 forms:
- mesotympanitis, which affects the mucous membrane of the tympanic cavity and auditory tube;
- epitympanitis, in which bone tissue is already involved in the inflammatory process, which can lead to its necrosis.
The danger of self-medication
Bilateral otitis media is a fairly serious disease that can lead to serious complications. That is why the treatment of such an illness cannot be delayed. Complex treatment of bilateral otitis involves various procedures, which can only be prescribed correctly by a qualified specialist.
Only after a thorough examination of the patient will a specialist be able to diagnose the exact stage of bilateral otitis and prescribe the necessary treatment. If you ignore the need to see a specialist or self-medicate, then otitis media can develop into a chronic form, which threatens that with any illness, otitis media will immediately make itself felt.
There are several general principles for the treatment of bilateral otitis media:
- If otitis has reached the stage when purulent discharge begins to appear, and the general body temperature has also increased significantly, it is strictly forbidden to resort to the use of thermal procedures. Warming manipulations are allowed only after a decrease in inflammatory processes and body temperature;
- Effective treatment of the disease includes the use of various medications that effectively fight inflammatory processes and harmful microorganisms;
- If bilateral otitis is diagnosed in a child and it is not treated for a long time, this may lead to the need to remove the adenoids. Surgical intervention is most often required if the source of the disease is localized near the paranasal sinuses and nasal cavity. If a specialist insists on surgical intervention, then there is no need to rush to abandon this method, because otherwise more serious diseases may arise;
- To effectively treat bilateral otitis media, it is necessary to strictly follow all the instructions of the attending physician. A lot of patients make a grave mistake - they stop taking medications immediately after the unpleasant symptoms of bilateral otitis media have passed. There is no need to do this, because the main task is not to relieve symptoms, but to eliminate the entire disease. Otherwise, there is a high probability that otitis media will develop into a chronic form;
- Bilateral otitis is usually caused by bacteria. The use of antibiotics helps to overcome the disease very quickly and effectively;
- If the inflammation occurs as a result of a viral infection, then bilateral otitis media is quite difficult to treat. Surgery may be required, in which a small tube is inserted into the patient's eardrum and allows any remaining pus and blood to drain from the ear canal.
Complications
Incorrect treatment for purulent otitis, after which the purulent-inflammatory pathology begins to cover the bone tissue, is fraught with severe irreversible consequences.
In this case, the following complications are possible:
- damage to the eardrum, after which you can completely lose your hearing;
- mastoiditis (inflammatory process of the temporal bone);
- osteitis (bone caries);
- labyrinthitis (inflammation of the inner ear);
- meningitis (inflammatory disease of the lining of the brain)
- encephalitis (inflammatory pathology of the brain).
Treatment of purulent otitis media
Diagnosing the disease in adults is usually not difficult. The diagnosis of “acute purulent otitis media” is made based on the patient’s complaints and otoscopy results. If bone destruction is suspected, an x-ray of the temporal bone is taken.
Treatment of the disease in adults is carried out on an outpatient basis; in the presence of fever and high temperature, the patient is prescribed bed rest. Treatment of acute otitis in a hospital setting is necessary if damage to the mastoid process is suspected.
Drug treatment includes:
- antibiotics;
- astringent or vasoconstrictor drops;
- painkillers.
Treatment of acute purulent otitis media is necessary based on the severity of symptoms and stage of the disease.
At the pre-perforative stage of the disease, the following drugs are used to relieve severe pain: alcohol solutions (boric acid or chloramphenicol with glycerin), heated ear drops (otipax, anauran), oral medications (diclofenac, paracetamol);
Means for simulating the drainage function: vasoconstrictor drops (galazolin, otrivin), warming alcohol compresses on the ear area to accelerate the resolution of the inflammatory process at home.
If necessary, paracentesis is used. During this operation, the eardrum is punctured to allow the unhindered drainage of pus.
At the second, perforated stage, experts recommend treating the disease using drug therapy:
- vasoconstrictor nasal drops;
- antibiotics;
- antihistamines;
- mucolytics (fluimucil, ACC);
- warmed ear drops after cleansing the ear with a solution of hydrogen peroxide.
In addition, effective physiotherapeutic treatment includes:
- Microwave;
- UHF;
- Ural Federal District;
- warming compresses at home on the ear area.
Treatment at the reparative stage, the main goal of which is to strengthen the immune system and restore hearing, is stopped: antibiotics, mechanical cleansing of the ear canal, and thermal procedures are canceled. To prevent adhesions in the tympanic cavity, the following may be prescribed: endaural iontophoresis using lidase, pneumatic massage of the tympanic membrane, and enzyme agents. To restore hearing, surgery may be necessary to remove adhesions and straighten the eardrum. Folk remedies can also help treat purulent otitis media at home One of the methods of alternative medicine is the use of mumiyo, which can even replace antibiotics. There are several known recipes for this healing drug:
- Instill a sore ear with an imperforated eardrum twice a day with a mixture prepared from mummy and rose oil mixed in a ratio of 1 to 10.
- As a pain reliever, insert a cotton swab soaked in a solution prepared from 100 grams of water and 2 grams of mumiyo into the ear.
Folk remedies prepared at home from lemon, pomegranate and bee products have also proven themselves well Most popular recipes:
- Place drops prepared from freshly squeezed lemon juice into the ear three times a day.
- Treat the ear canal of the affected ear with a mixture prepared from honey and pomegranate juice taken in equal quantities.
- For 3 weeks, insert a flagellum soaked in a 20% alcohol solution of propolis into the ear.
These and other folk remedies can be successfully used at home for both adults and children who have first consulted with their doctor.
How to treat acute diffuse otitis media
Acute diffuse otitis is expressed in inflammation of the skin and subcutaneous layers of the outer ear.
The causes of this disease can be damage to the skin of the ear canal caused by:
- injuries;
- unsuccessful manipulations during hygiene procedures;
- ingress of foreign bodies;
- burns;
- exposure to chemicals.
External diffuse otitis occurs when the damaged surface of the skin becomes infected with bacteria or fungi.
Acute diffuse otitis, as a rule, can manifest itself with the following symptoms:
- pronounced swelling of the outer ear;
- the presence of a boil at the site of injury;
- heat;
- pain;
- enlarged lymph nodes.
Depending on the nature of the infection, it is determined how to treat acute purulent otitis media.
Various treatment methods are used, such as:
- medicinal;
- physiotherapy;
- treatment with folk remedies;
- surgical intervention.
How to treat acute otitis media with medications:
- antibiotics in the form of ear drops or ointments;
- oral antibacterials;
- antifungal drugs in the form of ointments;
- antiviral drugs;
- hormonal drugs.
Physiotherapy includes the use of ultraviolet and UHF.
If the boil is large and there is no release of pus, then with the help of a surgical operation such a boil is opened and cleansed of purulent contents.
How to treat acute otitis media using folk remedies:
- cleansing the ear canal using tampons soaked in chamomile decoction or wild garlic juice;
- introducing into the ear turundas soaked in infusions and juice of herbs, such as nightshade leaves, plantain, mint;
- inclusion in the diet of foods that contain ascorbic acid (oranges, lemons, hawthorn, rose hips).
How to treat acute otitis media depends on many factors. In order for treatment to be effective, consultation with a doctor is necessary.
If your ear is leaking, it is recommended to consult an ENT doctor. Liquid discharge from the auricle is not a separate disease.
This occurs as a manifestation of symptoms of a disease of the ENT organs: ear, throat, nose. These organs are directly connected to each other by anatomical features. A doctor who examines and treats diseases of these organs is called an otolaryngologist.
Discharges can be of a different nature:
- bloody;
- purulent (white, yellow);
- transparent.
The causes of inflammatory disease of the outer and middle ear are associated with different types of bacteria. They cause purulent discharge (otitis media, fungus, open boil, exacerbation of inflammation). Bloody discharge occurs due to ear injury, tumor, or increased blood pressure. The cause of ear bleeding may be an inflammatory-infectious process:
- Fungi of the genus Candida cause thinning of the walls of blood vessels and further rupture. There is unbearable itching inside the ear, serous discharge, and deafness.
- Inflammatory processes of the hair follicle. This occurs due to a decrease in immune functions.
- Penetration of Staphylococcus aureus, pneumococcus, and Haemophilus influenzae into the ear canal.
Clear fluid may also be released. Inside the auricle, exudate is formed - a good nutrient medium for the development of pathogenic microflora. Then otitis media occurs; if treatment is not prescribed in a timely manner, the disease progresses and pus begins to leak out.
- With a high probability, exudate occurs in young children, unlike adults, behind the eardrum. When the pus begins to break through and flow out, the child will feel noticeable relief. Filling in the ear of children is explained by the origin of the exudate from the external environment or internal secretion. The occurrence of this pathology occurs due to reasons such as:
- chronic advanced purulent otitis media;
- water ingress;
- fungal infection;
- cerebrospinal fluid (through injuries to the head area);
- tympanostomy tube (during contact with water);
- cholesteatoma (perforation of the eardrum);
- the presence of a foreign body (most often in young children);
- necrosis (due to chronic otitis, paralysis of the facial nerve occurs);
- allergic otitis;
- granulomatous form (oral ulcers, rhinorrhea);
- advanced cancer.
- hearing loss;
- pain;
- dizziness;
- the appearance of ear noise;
- black spots are found in the discharge;
- lymph nodes enlarge.
In case of otitis media, it is necessary to provide assistance as quickly as possible to avoid additional complications of the disease. The cause of ear canal diseases in a child is a malfunction. This is due to the presence of adenoids.
The presence of fluid can be detected during examination of the ear cavity. An otolaryngologist uses an otoscope. A cloudy eardrum is observed. The presence of exudate in the ears is indicated by discharge. This causes severe pain, but later the condition improves.
When dark brownish discharge occurs, people think about pathology. After going to the doctor, it turns out that this is sulfur of a liquid consistency - a variant of the normal phenomenon. She has the ability to change her state. Moreover, its amount varies depending on the ambient and body temperature.
White liquid is released during otomycosis; there is a gray discharge with black dots. With bacterial inflammation, a yellow secretion flows out. The inflammatory process of the right ear is the initiator of the unpleasant smell of discharge. An unpleasant odor is accompanied by the malignant course of epitympanitis.
Discharge from the ears is accompanied by:
If your ear suddenly starts to leak, it's otitis media. What should not be done during otitis media?
- Compresses and heating pads are contraindicated before visiting a doctor.
- Do not reduce the course of prescribed medications on your own.
- It is strictly forbidden to use anti-inflammatory or alcohol-based drugs without a doctor’s prescription.
The absence of the appropriate one can be quite dangerous and provoke a decrease in auditory activity. The ears hurt, as a result the child will be restless. It is worth calling your local pediatrician.
Fluid like water may come out of your ears. At the same time, there is a very strong feeling of pain in the ears.
The causes of discharge can be a variety of pathologies of other anatomically related organs.
The ears are interconnected with the throat, nose, nasopharynx and oral cavity. For example, if the teeth are affected, this will affect the ears, so the pain will occur at the same time. In addition to the leaking fluid, the head hurts severely, then you need to urgently call a doctor.
Choice of antibiotics
Antibiotics for the treatment of acute purulent otitis are selected based on the spectrum of the causative bacterial flora. Today, cephalosporins (ceftriaxone, cefaclor, cefazolin), aminopenicillins (Amoxil) and macrolides (Klacid) are widely used in otolaryngology. These antibiotics effectively block with their activity those pathogenic microorganisms that cause inflammatory ear diseases.
Antibiotics for children are prescribed with extreme caution, depending on the severity of the disease and the age of the baby. The most popular antibacterial agents in children: suprax, flemoxin, amoxiclav, amoxicillin. Antibiotics are available in a form convenient for use in the form of soluble tablets, suspensions and syrups.
The duration of the course of these drugs should be at least 7-10 days. If antibiotics are stopped earlier, this may provoke a relapse of the disease, its transition to a chronic form and the development of complications.
Otipax
Otipax ear drops are well known to both patients and doctors. Being a combination of drugs such as phenazone and lidocaine hydrochloride, otipax is a non-steroidal drug that has an anti-inflammatory effect and provides a local analgesic effect.
Otipax is effective as a symptomatic treatment for some forms of chronic purulent otitis, as well as after surgery.
In addition, otipax has found its application in:
- otitis media in the acute period;
- viral otitis;
- barotraumatic otitis.
In adults, Otipax is used 4 drops 3-4 times a day, in children under one year old - 1-2 drops, 1-2 years old - 3 drops, older children - 4 drops three times a day. Treatment with Otipax should be carried out for 3 to 10 days. When using the drug in the recommended dosage, an overdose is unlikely.
Timely use of Otipax prevents the development of purulent complications and perforation of the eardrum.
Activities at the perforation stage
Despite the treatment, several days after the onset of the disease, the patient sometimes has pus flowing from the ear. What to do in this case? It all depends on where the patient is located and how quickly qualified assistance can be provided. In this case, consultation with an otolaryngologist is necessary to adjust treatment tactics.
The peculiarities of the use of drugs in the treatment of the middle ear in this period are that at this stage the use of alcohol-containing drops is contraindicated, since this substance can have a toxic effect on the mucous membrane of the eardrum and lead to a worsening of the condition. Products containing anti-inflammatory components have the same effect. Otipax drops are already contraindicated during this period.
Disease prevention
Everyone knows the truism that it is easier to prevent a disease than to treat it later. To prevent a disease such as acute purulent otitis media, it is necessary to eliminate the main factors that can lead to its occurrence. For this it is important:
- harden the body;
- keep your ear canals clean at home;
- promptly treat infectious and chronic diseases and visit the dentist.
The best preventative measure for infants is breastfeeding.
By making it a rule of life to carry out these simple activities, you can forever forget about such a disease as purulent otitis media and keep your ears healthy and your hearing sensitive.
Author: Mikhail Zagorodnyuk, especially for lechim-gorlo.ru
Diagnostics
The process of diagnosing the disease should be entrusted to an experienced specialist. Initially, the patient is interviewed, his complaints, the possible occurrence of otitis in the past and its treatment are clarified.
After taking a medical history, the doctor examines the ear canal using instruments. Tympanometry and other types of studies may be used. Often, material is collected to study the causative agents of the disease. In some cases, a CT scan of the temporal lobes is performed.
To ensure a complete inspection, rinsing and cleaning is carried out before starting the inspection. The accumulated pus is completely removed so that it does not interfere with the diagnosis.