Muscular atrophy is a process characterized by a gradual decrease in volume, degeneration and thinning of muscle fibers, and a decrease in their contractility.
All types of atrophy can be divided into 2 large groups:
- hereditary degenerative - muscle atrophy caused by genetic defects of both the muscles themselves and the nerve fibers that regulate their work. They most often develop in childhood, progress quickly and are practically untreatable.
- simple - atrophies that occur against the background of various diseases, intoxications, injuries.
Causes of disease in children
- Hereditary neuromuscular diseases (Erb-Roth myopathy, Duchenne myopathy, Charcot-Marie-Tooth amyotrophy, etc.) are the main cause of muscle atrophy in childhood;
- Birth injuries - damage to peripheral nerves, nerve plexuses during labor;
- Fractures of the limbs, spine;
- Dermatomyositis is an autoimmune inflammation of the skin and muscles;
- Infections (poliomyelitis, tuberculosis).
Causes of the disease in adults
Muscle wasting in adults most often develops under the influence of external damaging factors. As for hereditary diseases, most of them come from childhood, and only rare forms first manifest themselves in middle and old age.
The most common reasons include:
- Paralysis after strokes, cerebral hemorrhages;
- Severe traumatic brain injuries and spinal cord injuries;
- Prolonged immobilization of limbs after fractures, prolonged immobilization of patients after operations, severe concomitant diseases;
- Aging – natural degenerative changes in all organs and tissues;
- Poor nutrition, starvation;
- Digestion and absorption disorders (chronic diarrhea, intestinal resection)
- Infectious diseases - tuberculosis, chronic dysentery, malaria, enterocolitis.
- Parasitic diseases (trichinosis, echinococcosis);
- Malignant tumors (lung, breast, thyroid cancer) – cancerous depletion;
- Endocrine pathology (thyrotoxicosis, myxedema, Itsenko-Cushing's disease, diabetes mellitus, acromegaly);
- Arthritis, arthrosis;
- Polymyositis, dermatomyositis;
- Chronic alcoholism;
- Taking certain medications (glucocorticosteroids, colchicine).
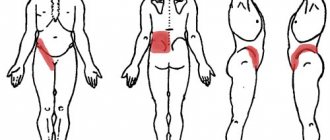
What muscle tissue looks like normally and against the background of various diseases. (see picture)
- Norm
- Diabetes mellitus
- Scleroderma
- Polymyositis
- Collagenosis
- Neoplasms
- Itsenko-Cushing syndrome
- lupus erythematosus
- Thyrotoxicosis
Causes of leg muscle atrophy
Atrophy of the fatty tissue of the lower leg can occur for various reasons:
- Natural aging of the body, in which there is a decrease in metabolic rate.
- Connective tissue pathologies.
- Poor nutrition means the body does not receive the required dose of vitamins and minerals.
- Constant excessive physical activity.
- Diseases of the digestive system.
- Hormonal imbalance, disruption of the endocrine system.
- Tightness in the foot, atrophy of the calf muscle - the causes of these pathologies can be previous surgeries and injuries.
The atrophic process can occur due to injury to the nerve trunks. This most often occurs due to the development of infectious inflammation, which adversely affects the motor cells of the spinal cord. Against this background, the patient loses sensitivity.
Secondary atrophy, in turn, is divided into several main types:
- Progressive – symptoms most often appear in childhood. The disease is very severe, complete loss of tendon reflexes occurs.
- Neural atrophy is damage to the lower leg and feet. A gait disturbance develops; the patient raises his knees high when walking. Subsequently, the foot completely loses its sensitivity, then the disease begins to spread to other parts of the body.
Any infectious disease, physical stress, metabolic disorder or serious injury can trigger the disease.
Disability due to diseases of the gluteal muscles
There are many disability criteria by which the condition of a child with atrophy or dystrophy of the gluteal muscles is assessed:
- Impairment of motor functions, which causes disability, impairment of the ability to move independently and maintain services.
- Social impairment and partial impairment of life functions.
- Impaired motor function of the limbs.
When assessing the health status of persons over 18 years of age, other ITU disability criteria for atrophy of the hip muscle are used:
- Group 1 – inability to move and perform basic self-care activities;
- Group 2 – limited ability to move, ability to work 2-3 degrees;
- Group 3 – moderate atrophy, in which a person is entitled to reduced work time and reduced qualifications.
Disability is given indefinitely to patients who have a progressive course of the disease, as well as when rehabilitation measures are ineffective.
Since atrophy and dystrophy of the muscles of the buttocks can lead to a person’s complete inability to move, it is worth treating all muscle diseases in a timely manner, avoiding hypothermia and overexertion.
Symptoms of the disease
The first symptom is weakness in the legs after the simplest physical activity. The calf muscles increase in size. Restrictions in motor function are felt, for example, the patient cannot climb stairs.
Drying of the calf muscle of the leg occurs gradually, usually the atrophy process lasts several years.
The disease can affect either one calf muscle or two at once.
In addition, it can occur both symmetrically and asymmetrically. The fat layer on the affected limb gradually decreases.
Over time, a more obvious clinical picture develops:
- Reduction in volume of the calf muscle. The patient's gait changes and it becomes difficult to move without assistance.
- Periods of exacerbation occur. Sometimes the patient suffers from severe muscle pain, then the symptoms may subside. But this does not mean that the disease goes away.
- The primary form of atrophy is characterized by rapid fatigue in the legs, muscle tone is lost, and twitching of the limbs is observed.
- The secondary form manifests itself as neuropathy. Deformation of the feet and legs occurs. The leg stops obeying the person. The foot seems to hang, because of this, when walking, it catches on the floor. The patient has to raise his leg high to take a step. As the disease progresses, muscle weakness moves from the legs to the hands.
It is important to correctly identify the symptoms in order to correctly prescribe treatment. When making a diagnosis, the general condition of the patient and the symptoms of the disease are taken into account. Treatment methods are always selected individually.
Clinical signs and diagnosis of muscle atrophy of the lower extremities
The development of the disease occurs slowly, with a gradual increase in the severity of the clinical picture. The first symptoms of the disease are the appearance of muscle weakness, changes in the patient’s gait, and rapid fatigue. The gait that occurs at the initial stage of development of atrophy is swaying, reminiscent of a duck.
Over time, a significant decrease in volume of the affected muscles becomes visually visible. They lose tone and become flabby. The patient cannot walk for a long time and gets tired quickly. He needs rest.
With atrophy of the lower leg muscles, deformation and atony of the lower limb occurs. In this case, raising the patient's leg leads to limp sagging of the foot. With disturbances in nerve conduction, which is the cause of atrophy, the limb may lose pain sensitivity and lose previously existing reflexes.
Atrophy itself is extremely rarely accompanied by the development of pain. However, such sensations may occur due to the underlying disease that caused atrophic phenomena (intermittent claudication due to atherosclerotic lesions of the vessels of the legs).
Diagnosis of the disease is carried out on the basis of visual examination, palpation of the muscle formations of the legs, as well as after assessing their functional state. At the same time, it is important to remember about the possible phenomena of pseudohypertrophy, when the subcutaneous tissue volume can be preserved due to fat and connective tissue deposits that arise in the place of the atrophied muscle.
Diagnosis and treatment methods
First of all, a thorough examination of the patient is carried out to determine his hereditary predisposition to atrophy. A full examination is prescribed to identify chronic diseases, as well as a biopsy of nerves and muscles.
Treatment is always prescribed individually. It all depends on the cause and course of the disease, the age of the patient. A complete cure is impossible, but with the help of drugs and physiotherapy it is possible to return the patient to normal life, relieve pain symptoms, and restore metabolic processes.
Be sure to take not only medications, but also vitamins and minerals that help normalize metabolism.
Such patients must be prescribed a massage. It maintains muscle tone and improves blood flow to a weakened lower leg. You can also use special elastic ankle bandages.
Important! Therapeutic massage should only be performed by a specialist. What it will be and how long the course will last can only be decided by the attending physician.
Muscle degeneration begins with 8 early symptoms. Don't ignore them
Guys, we put our hearts into Bright Side. Thank you for revealing this beauty. Thanks for the inspiration and goosebumps. Join us on Facebook and VKontakte
Muscular dystrophy is usually caused by genetic mutations and results in the progressive destruction and loss of muscle cells in the body. It includes more than 150 diseases that manifest themselves in different ways, but almost all of them begin with subtle symptoms. These symptoms gradually worsen if you do not pay attention to them in time.
Bright Side has listed the 8 most common warning signs of muscle degeneration that you should never ignore.
Muscle pain and spasms
The loss of muscle cells usually causes a feeling of weakness in the muscles. So if you have trouble getting out of a chair, combing your hair, lifting objects, or constantly dropping things, then you may be suffering from muscular dystrophy.
You may also feel that your muscles are tight and have lost flexibility, and frequent muscle pain indicates that something is clearly wrong with them. At the same time, symptoms such as prolonged spasms, tightness and tension in the muscles of the arms and legs may be signs of myotonia, a serious disease that requires medical intervention.
Enlarged calf muscles may be a sign of Duchenne muscular dystrophy. This disease usually occurs in boys at an early age and develops very quickly.
If you are affected by Duchenne disease, your calves are the muscles that suffer first, as they bear a lot of the strain of stabilizing the rest of your body. In this case, the muscles are gradually replaced by fat and scar tissue.
If your muscles are not strong enough to keep your back straight , you may have poor posture, which over time will lead to scoliosis. With this disease, your back curves to the right or left, which leads to displacement of internal organs.
Scoliosis usually appears during adolescence and is diagnosed more often in women than in men. This disease has many negative health consequences, including headaches and persistent leg pain.
Breathing problems
In severe cases of scoliosis, progressive muscle weakness can affect the chest muscles associated with the breathing process . While you may not experience difficulty breathing per se, you may suffer from problems that indicate poor respiratory function, including headaches, inability to concentrate and nightmares.
Types of muscle atrophy
Muscular atrophy is divided into two main groups: primary muscle atrophy and secondary, the latter in turn is divided into several more groups - neural myotrophy, Arand-Duchenne atrophy and progressive atrophy.
- Neural myotrophy is a disease that is associated with changes in the shape of the lower leg and foot. Due to thinning of the muscles, patients' gait is impaired - they are forced to raise their knees high when walking so as not to get caught on the foot, since the muscles responsible for its flexion and extension practically do not work, and the foot simply hangs when raising the leg. When there are practically no foot reflexes, the disease slowly spreads to the upper limbs.
- Progressive atrophy most often occurs in children under five years of age. With this form of the disease, blood pressure decreases, a person's legs twitch, and leg reflexes are gradually lost.
- Arand-Duchenne atrophy is a type of atrophy that first affects the upper extremities; the patient's fingers and interosseous muscles atrophy, and the hand takes on a monkey-like appearance. There are no tendon reflexes, but the sensitivity of the hands is not lost. If the disease is not treated, the muscles of the neck and torso gradually atrophy.
Exercises to restore thigh muscles
A hip fracture is considered one of the most dangerous injuries. The fact is that the bones in this place grow very poorly due to their complex structure. But loss of motor activity in the legs can also be a consequence of surgery in the treatment of arthrosis or arthritis. In any case, exercises for recovery after surgery or a hip fracture will help you get back on your feet faster.
- Sitting or lying down, we raise and lower the toes of our feet.
- In the same pose, rotate the foot in a circle.
- We strain the leg pressed to the bed for 5-10 seconds - this way we restore the quadriceps muscle.
- Without lifting your heels from the bed, pull them towards your buttocks and bend your knees.
- Contract the buttocks and hold them in this state for 5-7 seconds.
- We move our legs to the sides one by one.
- Slowly lift the straightened leg.
Causes
Primary myotrophy is expressed directly in the damage to the muscle tissue itself. This type of atrophy can be caused by:
Endocrine system diseases- Violation of muscle trophism
- Serious disorders in internal organs
- Aging of the body
- Hereditary predisposition
- Congenital defect of muscle enzymes and high levels of membrane permeability
- Damage to muscle tissue by infection
- Injuries
- Lack of physical activity and, conversely, excess of it, when a person overexerts himself in the gym, but does not receive enough protein for the muscles to recover.
- Atrophy can occur due to prolonged lying after an injury, for example, elderly patients after a hip fracture are forced to remain in a horizontal position for many months in a row.
Secondary atrophy develops when the facial horns of the spinal cord, peripheral nerves, roots, stem nerves are damaged, with poliomyelitis and similar diseases. A previous infectious process can also provoke secondary atrophy. Secondary atrophy is characterized by a slower course than primary atrophy.
People suffering from diabetes have a wide variety of problems with their lower extremities, as this disease affects different systems and processes. Muscle atrophy is one of the reasons why legs may hurt in diabetes.
General symptoms
Regardless of the cause, all muscle atrophies have similar manifestations. At the beginning of the disease, slight weakness in the limbs during physical activity is a concern; after a while, difficulties in movement appear, it is difficult to perform usual actions: climbing stairs, running, getting up from a low chair, fastening buttons, carrying a bag, etc.
With hereditary pathology, the first symptoms usually appear in childhood and increase quite quickly. Over the course of several years, and sometimes several months, patients lose the ability to move independently and take care of themselves.
In some diseases, the legs weaken first, in others – the arms, but in all cases, symmetrical damage to the extremities is characteristic. Proximal (located closer to the body) muscle groups are most often affected. At the same time, the muscles of the back, chest, abdomen, and face become thinner.
In hereditary diseases, muscle atrophy is the main symptom that completely determines their clinical picture and further prognosis.
Simple atrophies, as a rule, develop against the background of other long-term chronic diseases. In this case, the symptoms of the underlying disease come to the fore. Muscle wasting increases slowly and is often unnoticed by the patient. Both symmetrical and asymmetrical lesions are possible. The legs are affected first, starting from the feet and legs, later the muscles of the hands and arms as a whole are involved.
With timely treatment, complete recovery can be achieved.
Muscle atrophy: treatment
The sooner treatment is started, the less muscle tissue will be lost. Treatment of atrophy is aimed at slowing down or completely stopping the process of degeneration of muscle fibers rather than at curing it. Since if a large number of muscle fibers have been replaced by connective tissue, it is almost impossible to completely restore motor function. But sometimes, when the patient follows the doctor’s recommendations clearly and carefully, some improvement is still observed. The course is prescribed taking into account the patient’s age and stage of the disease. As a rule, the doctor prescribes Atrifos or Myotrifos (adenosine triphosphoric acid); vitamins E, B1 and B12; Galantamine; Prozerin strongly recommends therapeutic exercises, electrotherapy, and physiotherapeutic procedures. Proper nutrition and quitting smoking and alcohol also play an important role for a good result.
Forms of the disease and characteristic symptoms
It is important to understand the differences between muscle atrophy, dystrophy and hypertrophy. The concepts have a lot of differences:
- Atrophy refers to processes that lead to muscle thinning and loss of functionality. Many hereditary diseases, as well as minimal muscle activity, lead to pathology.
- Dystrophy - the concept describes a group of hereditary diseases that lead to necrosis of muscle fibers. They affect skeletal muscles. As a result of the development of diseases, weakness and degeneration of fibers occurs.
- Hypertrophy. It appears when the volume of muscle fibers increases. The muscles noticeably increase in volume and gain strength. This condition is typical for healthy people. Pathological muscle enlargement is called pseudohypertrophy or false hypertrophy. In fact, such diseases are classified as dystrophic.
Thus, myodystrophy (disease) can lead to atrophy (the process of death of muscle fibers).
The symptoms of various pathologies of the buttock muscles are similar in many cases. The muscles of the lower back weaken and lose functionality. The gait becomes unnatural; it is also called a “duck walk.” Visually, the buttocks become smaller and lose their natural round shape. With dystrophic changes in the muscles, they can increase, but not due to the growth of fibers, but as a result of fat deposition and the proliferation of connective tissue. After 5-8 years, the patient may be completely immobilized.
Common dystrophic changes in muscles are typical for boys, since hereditary diseases affect the male sex chromosome (Duchenne and Becker dystrophy). There are several types of hereditary dystrophic diseases that are characteristic of both sexes.
Causes and symptoms of muscle atrophy in the legs, thighs and lower legs
Causes of atrophy of the muscles of the legs, thighs and lower legs
There may be several reasons for the development of muscle atrophy of the lower extremities:
- decreased metabolism and aging of the body with age;
- as a result of diseases of the endocrine system and hormonal imbalance in the body;
— chronic diseases of the digestive tract, connective tissue;
- dysregulation of muscle tone with damage to peripheral nerves, polyneuritis, as a manifestation of complications of certain infectious and parasitic diseases, chronic poisoning;
- poor heredity - congenital enzymopathy or genetic disorders;
- malnutrition, insufficient nutrition;
- as post-traumatic complications or with constant physical activity.
Diseases associated with muscle atrophy, as a rule, are rare congenital genetic diseases that begin to manifest themselves in childhood.
Symptoms of muscle atrophy in the legs, thighs and lower legs
Muscle atrophy develops slowly and lasts for years. The disease can spread to either one or both sides; the process can be either symmetrical or asymmetrical. All manifestations depend on the causes and form of the disease, age and condition of the patient’s body. Clinical manifestations include increasing weakness in the lower extremities and trembling. Patients experience discomfort, a feeling of goosebumps crawling under the skin.
The primary form of muscle atrophy is characterized by damage to the muscle itself and its motor neurons, caused by unfavorable heredity or a number of other reasons - injuries, bruises, physical overexertion. The patient gets tired very quickly, the muscles lose tone, and involuntary twitching of the limbs is characteristic.
Found an error in the text? Select it and a few more words, press Ctrl + Enter
Sex-linked myotonia, accompanied by atrophy of the leg muscles
As a rule, children with this congenital genetic disease do not live beyond the age of 14.
Found an error in the text? Select it and a few more words, press Ctrl + Enter
In the mid-twentieth century, Becker described a benign variant of sex-linked myopathy; this form of the disease bears his name. The first symptoms of pathology appear after 20 years. At the initial stage, pseudohypertrophy of the calf muscles is noticeable. Atrophy of the leg muscles develops slowly, gradually covering the muscles of the pelvic girdle and hips. Intelligence is preserved in this form. These types of the disease are characterized by damage to various genes located in two loci of the sex X chromosome, being genocopies. Two forms of the disease do not occur in one family at once.
Diagnosis of atrophy of the muscles of the legs, thighs and lower legs
Treatment of muscle atrophy in the legs, thighs and lower legs
When copying materials, an active link to the website www.ayzdorov.ru is required! AyZdorov.ru 2009-
The information on the site is intended for informational purposes only and does not encourage self-treatment; consultation with a doctor is required!
Treatment
For muscle atrophy of any etiology, first of all, the underlying disease is treated.
Muscle wasting in myopathies and amyotrophies is mostly irreversible, so the goal of treatment for such diseases is to slow down the progression of the process.
Simple atrophies are reversible to a certain extent, and with timely initiation of therapy, complete recovery is possible.
Diet
Patients are prescribed a diet high in protein and limited in animal fats and carbohydrates. It is recommended to include fish, liver, low-fat cottage cheese, soy meat, and vegetables in the diet.
Drug treatment
Drug therapy is used to compensate for energy deficiency, improve blood supply and metabolism in atrophied muscles. Prescribed:
- B vitamins, vitamin A and E,
- amino acids,
- anabolic agents (potassium orotate, retabolil, riboxin),
- ATP,
- Drugs that improve peripheral blood circulation (pentoxifylline, nicotinic acid),
- nootropic drugs (Cerebrolysin),
- drugs that improve the conduction of nerve impulses - cholinesterase antagonists (prozerin).
Physiotherapy
Dosed physical training significantly improves the functional state of muscles, increases muscle mass, and has a general strengthening effect.
- The exercises are performed in a gentle manner from a relaxed starting position, avoiding severe muscle fatigue for no more than 30-45 minutes.
- Exercise therapy course 25-30 times, subject to daily classes according to an individual program. Next, the patient should also exercise regularly.
- Both passive and various types of active movements, exercises in water, and stretching exercises are used.
- If necessary, they resort to the help of a methodologist and use various devices.
- Exercises in water (in a bath or pool) have a good effect.
Exercises 1 - 4 are performed passively with the help of a methodologist, exercises 5 - 10 are performed by the patient independently.
- 1 - lying on your side, you need to bend and straighten your legs at the knees,
- 2 - in a position on the side, it is necessary to bend and extend the arms at the elbows,
- 3 - in a supine position, abduction and adduction of the legs are performed;
- 4 - in a supine position, abduction and adduction of the arms are performed;
- 5 - the patient lies on his back, slowly pulls his legs towards the pelvis, and then straightens them back;
- 6 - lying on your back, you need to slowly raise and lower your arms;
- 7 - lying on your side, you need to alternately abduct and adduct your leg;
- 8 - lying on your side, you must alternately abduct and adduct your arm;
- 9 - the patient lies on his stomach with his arms extended along the body, while slowly raising and lowering his head and shoulders;
- 10 - raising the pelvis from a supine position with legs bent at the knees.
If the patient has isolated localized paresis
, which usually covers a large area of a limb or even one or more limbs, but no other pathological changes are detected, this raises suspicion of psychogenic paralysis.
It is characterized by
: • Localization of weakness in a limited area of the body, but not corresponding to the zone of motor innervation of the peripheral nerve or root. • No sensory impairment. If they are detected, the zone of their distribution does not correspond to the area of innervation of the peripheral nerve (often it is a circular area of total analgesia and anesthesia on the limbs or a limited area exactly along the midline of the body).
• Absence of so-called objective signs, namely at least minimal atrophy (lack of activity in a limb for a long time causes mild muscle atrophy), changes in reflexes or pathological reflexes. However, very long-term functional paralysis can lead to decreased tendon reflexes. • Contradictions in showing weakness in different situations. For example, the patient presents with total flaccid plegia of the extensors of the foot during examination and the absence of stepping when walking; total flaccid plegia of the arm and absence of accompanying movement of the arm in accordance with centrifugal force during active or passive rotation of the body around its axis; a complete violation of the extension of the hand and fingers, but a noticeable reflex tension of the extensor muscles when clenching the hand into a fist (this is also possible with organic central paresis of the hand - “main mecanigue”, according to Babinsky, but is accompanied by other objective signs of central spastic paralysis - changes in tone and reflexes).
These features of psychogenic damage
also applicable to patient-reported sensory disorders. They should be paid attention to in case of suspicion of both unconscious somatoform psychogenic disorders and feigning paralysis.
Muscle weakness accompanied by muscle atrophy
Isolated movement disorder
in the form of paresis with muscle atrophy should be analyzed depending on its location and area of distribution.
• Relatively symmetrical lesion
supports primary myopathy. - Primary myopathies are a disease exclusively (or at least predominantly) of muscle fibers (or the motor end plate). Despite some features, all diseases of this group are characterized by a number of common features: symmetry of the lesion (exception - myasthenia gravis), slow progression over many years (exception - myositis), atrophy of the affected muscles (there are also exceptions), weakening of tendon reflexes, absence of sensory impairment , fasciculations, pyramidal signs, in some cases complicated by a hereditary history or the presence of the disease in relatives, a relatively pronounced increase in CPK activity, changes detected when performing needle myography, biopsy and MRI of muscles.
Causes and symptoms of muscle atrophy in the legs, thighs and lower legs
Causes of atrophy of the muscles of the legs, thighs and lower legs
There may be several reasons for the development of muscle atrophy of the lower extremities:
- decreased metabolism and aging of the body with age;
- as a result of diseases of the endocrine system and hormonal imbalance in the body;
— chronic diseases of the digestive tract, connective tissue;
- dysregulation of muscle tone with damage to peripheral nerves, polyneuritis, as a manifestation of complications of certain infectious and parasitic diseases, chronic poisoning;
- poor heredity - congenital enzymopathy or genetic disorders;
- malnutrition, insufficient nutrition;
- as post-traumatic complications or with constant physical activity.
Diseases associated with muscle atrophy, as a rule, are rare congenital genetic diseases that begin to manifest themselves in childhood.
Symptoms of muscle atrophy in the legs, thighs and lower legs
Muscle atrophy develops slowly and lasts for years. The disease can spread to either one or both sides; the process can be either symmetrical or asymmetrical. All manifestations depend on the causes and form of the disease, age and condition of the patient’s body. Clinical manifestations include increasing weakness in the lower extremities and trembling. Patients experience discomfort, a feeling of goosebumps crawling under the skin.
Causes and forms of the disease
Muscle atrophy of the lower extremities can occur as a result of:
- decreased metabolism as a consequence of aging;
- disruptions in the functioning of the endocrine system and disturbances in human hormonal levels;
- chronic diseases of the digestive system and poor nutrition;
- connective tissue problems;
- genetic changes;
- lesions of the peripheral nervous system and other diseases that provoke a decrease in the regulation of muscle tone;
- injuries and improper recovery after surgical intervention.
In most cases recorded in the world, the cause of the development of leg muscle atrophy is genetic changes that manifest themselves at an early age, and various types of injuries, including those received during heavy physical exertion.
At the moment, medicine knows 2 forms of the considered pathology of the muscles of the limbs: primary and secondary. The first is characterized by damage to the motor neurons of the muscular system as a result of injuries or genetic changes and is manifested by a sharp decrease in tone, increased fatigue and more frequent involuntary twitching of the foot.
The second form of the disease has several varieties:
- “Neural amyotrophy” is characterized by deformation of the muscles of the foot and lower leg of both one lower limb and two at the same time. It is not difficult to recognize it, just look at the movements of a person when walking: his foot hangs, the patient has to constantly raise his knees high in order to avoid falling following the inability to control the lower part of the affected leg.
- Progressive - characterized by the absence of tendon reflexes, severe hypotension and frequent twitching of the lower limbs.
- Arana-Duchenne is a type of secondary form of pathology, characteristic of the hands (starts with the hands and gradually spreads to the whole body), in which the patient experiences psychological distress, because his upper limb swells to enormous sizes over time. Sensation in the legs remains, but tendon reflexes disappear.
In the absence of timely help from specialists, the second form of muscle atrophy begins to progress, gradually affecting the arms (it all starts from the lower sections and ends with the shoulder), and then the entire human body. Preserving muscles (avoiding their replacement with connective tissue that is not prone to stretching), returning their contractile abilities and giving the patient a chance to return to a full active life will allow timely diagnosis of the problem. To do this, you need to know the symptoms of leg muscle atrophy that the body exhibits with the disease in question.
Restoration of leg muscles after their atrophy
Causes and forms of the disease
Muscle atrophy of the lower extremities can occur as a result of:
In most cases recorded in the world, the cause of the development of leg muscle atrophy is genetic changes that manifest themselves at an early age, and various types of injuries, including those received during heavy physical exertion.
The second form of the disease has several varieties:
Symptoms
The disease develops over a long period of time, first affecting the proximal parts of the muscle tissue, and then spreading at high speed throughout the body.
Myotonia occurring against the background of muscle atrophy
A terrible consequence is brain damage, manifested in developmental delays and disruptions in the functioning of the cardiovascular system. The activity of the respiratory system is weakened, which leads to pneumonia.
The benign form of the disease, named after the scientist Becker, manifests itself in damage to the muscles of the thigh and pelvic area. A distinctive feature is the absence of an intellectual gap in the patient.
Diagnosis of the disease
How is the disease treated?
Based on the data obtained during diagnostic measures, the doctor will prescribe treatment for leg muscle atrophy, which includes:
- drug therapy;
- physiotherapy;
- exercise therapy;
- development of a special diet.
The health complex is selected individually and depends on the cause of the disease, its form, the patient’s condition (age, presence of chronic diseases, etc.).
Drug therapy
Medications are prescribed to the patient primarily to relieve symptoms. For this purpose use:
Only the attending physician has the right to write prescriptions for drug therapy, because he is fully familiar with the person’s condition, knows the characteristics of the existing illness and is aware of the patient’s allergy to one or another component of the drug.
Physiotherapy
Massage as a type of physiotherapy is the most useful method for improving blood flow to affected areas, restoring cellular nutrition, accelerating tissue regeneration, “breaking” stagnation and relieving excess tension. This procedure should be carried out daily, and if possible, a couple of times a day for a long time (at least 2-3 weeks).
Massage movements should be superficial, so as not to aggravate the situation; the procedure should be started from the periphery (from the foot) and do not forget to work the buttocks. The quadriceps femoris muscle may be subject to a little more manipulation.
Therapeutic exercise is prescribed by the attending physician and should be carried out only under the supervision of an experienced specialist: he will help you recover competently, gradually increasing the load and working out the damaged areas.
The growth of muscle tissue is impossible without proper nutrition. The normalization of metabolic processes, designed to restore normal functioning of the cells of the whole body, is facilitated by following a certain diet. It is developed strictly individually, taking into account all the patient’s characteristics (nutrition recommendations for patients with diabetes and chronic bronchitis will be different).
The diet should include:
The food consumed should be rich in protein (for muscle building) and carbohydrates (energy).
Folk remedies
There are also alternative medicine recipes that can help overcome muscle atrophy of the lower extremities (relieve unpleasant symptoms).
Herbal infusion
Oat kvass
Reed panicles
They are soaked in hot water for 45 minutes, then tied to the sore leg. This is a kind of compress, the effect of which can be enhanced if you wrap your leg in a blanket or blanket. The duration of the procedure is 1-1.5 hours.
Garlic tincture against numbness of extremities
Be sure to discuss with your doctor the possibility of using this or that traditional medicine. If you experience discomfort or allergies, you should immediately stop taking it and consult a doctor.
Prevention
Ways to prevent leg muscle atrophy:
Muscle atrophy is a pathology, which can be completely eliminated and a return to normal life possible only at the initial stage (when the disease manifests itself in a mild form). Therefore, if you notice any unpleasant sensations or visual changes, you should immediately contact a medical facility.
Prevention
Ways to prevent leg muscle atrophy:
- proper nutrition, rich in microelements necessary for the body to function properly;
- timely visits to doctors (medical examinations and medical examinations) and elimination of identified diseases;
- moderate physical activity;
- compliance with rehabilitation tactics after surgical intervention or injury;
- wearing comfortable shoes;
- compliance with healthy lifestyle rules.
Muscle atrophy is a pathology, which can be completely eliminated and a return to normal life possible only at the initial stage (when the disease manifests itself in a mild form). Therefore, if you notice any unpleasant sensations or visual changes, you should immediately contact a medical facility.
Treatment of muscle atrophy
The disease is pseudohypertrophic type of Duchenne. It consists of a frequent manifestation of myopathy, directly depends on gender, and manifests itself exclusively in boys.
Secondary pathology
The pathology affects the body of children in the first 5 years of life. The disease is characterized by atrophy of the pelvic and leg muscles. There is an early development of pseudohypertrophy, including the muscles of the calf area. By checking the knee reflexes, it can be noted that the tendons have undergone retraction. The child has difficulty moving and cannot jump or climb stairs normally. The disease is accompanied by developing weakness; the shoulder muscles are additionally included in the process of atrophy. After a while, the child will not be able to get out of bed.
Further symptoms of the disease, if there was no sufficient timely treatment, are expressed in the manifestation of noticeable contracture due to tendon retraction. The “horse” foot develops.
A dangerous manifestation of the disease is its effect on the child’s brain, which is why the boy begins to lag behind in development. The muscles of the heart change, the respiratory system weakens, accompanied by poor ventilation of the lungs, and pneumonia often develops. Due to the pathological condition of organs, including the heart and cardiac muscle, pneumonia is severe, periodically ending in death.
In the twentieth century, a scientist named Becker was able to describe a benign type of myopathy, which later acquired his name.
The peculiarity of the disease is that it manifests itself after twenty years. Atrophy itself occurs slowly, covering the muscles of the pelvis and hips. A characteristic feature of the type is the constancy of a person’s intellectual abilities. Such types of pathology are associated with damage to different genes located in two loci of the X chromosome, acting as gene copies.
Diagnosis of leg muscle atrophy is carried out by collecting a detailed history of the person, the presence of chronic diseases and hereditary burden. The patient should be referred for a complete blood test to determine the level of ESR, liver function tests, and glucose. An electromyography procedure is performed.
To determine the optimal treatment, doctors prescribe a biopsy of the nerves and muscles. At the same time, additional studies are carried out if the patient has a history of chronic or hereditary diseases.
Today, the diagnosis of this pathology does not present any difficulties. Identification of the underlying cause of the development of the disease is carried out using detailed clinical and biochemical blood tests, functional studies of the liver and thyroid gland. Be sure to do electromyography, a biopsy of muscle tissue, and study nerve conduction. If necessary, additional examination methods are prescribed.
If muscle atrophy occurs, treatment depends on many factors - the form of the disease, the severity of the process, the age of the patient. Drug therapy involves taking medications.
- Medication "Galantamine". The use of this drug greatly facilitates the conduction of nerve impulses. Use the medicine for a long period of time and gradually adjust the dose. Only a doctor should prescribe medication. It is used in the form of intravenous, intramuscular or subcutaneous injections.
- Medicine "Pentoxifylline". This drug dilates peripheral blood vessels and improves blood flow in the lower extremities. Antispasmodic medications - “No-shpa”, “Papaverine” - have a similar effect.
- B vitamins (pyridoxine, thiamine, cyanocobalamin). Vitamins improve the conduction of nerve impulses and the functioning of the peripheral nervous system. In addition, they activate metabolism in tissues and organs, due to which lost muscle volume is restored much faster.
Also in normalizing the condition, an important role is played by: proper nutrition, therapeutic exercises, physiotherapeutic procedures, massage, psychotherapy, and electrotherapy. If the cause of a child’s lagging behind in intellectual development is muscle atrophy, treatment involves neuropsychological sessions that will smooth out problems in learning new things and in communication.
The diagnosis and treatment of muscle atrophy is carried out by therapists and neurologists. If muscle weakness occurs, you should immediately consult a doctor to begin treatment at an early stage. The fact is that atrophy is an incurable pathology that progresses in the absence of treatment. To improve your quality of life, you need to start treatment as early as possible.
The disease is diagnosed quite simply; characteristic abnormalities in muscle tissue are visible. To confirm the diagnosis, the following tests are prescribed:
- Blood tests, general and biochemical;
- Visiting an endocrinologist to monitor the thyroid gland;
- Liver monitoring tests;
- Electromyography;
- Checking nerve patency;
- If necessary, a muscle biopsy may be prescribed.
Depending on the diagnosis, other studies may be recommended, as well as consultations with various specialists.