Eosinophils are cells from a group of leukocytes that are highly sensitive to eosin. The level of these cells indicates the presence of parasites in the body, inflammation and a tendency to allergies. Moving, eosinophils enter the inflammatory focus, the injured area. The cells remain in the blood for about an hour, then penetrate into the tissue structure. Scientists call them scavenger cells for their ability to remove pathogens and foreign substances from the body. When performing an analysis, a reduced level of an element may be detected. You should not make a diagnosis yourself; it is better to consult a doctor for a decipherment of the test results.
Why do the human body need eosinophils?
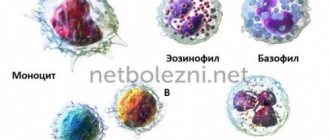
An eosinophil is a blood cell that is a subtype of granulocyte. Leukocytes protect the body from inflammatory processes caused by the presence of foreign pathogens. Eosinophils do not have a specific color. The cell is stained under the influence of an acidic dye, eosin.
Eosinophilic cells form in the bone marrow region. They are produced by stem cells - the precursors of pathogens of the leukocyte group. Elements are characterized by a lack of ability to divide. The formation process takes 3-4 days, after which maturation occurs with gradual penetration into the general blood stream for 6-12 hours.
The lifespan is 10-14 days. Through the bloodstream, genomes penetrate into the tissues of the gastrointestinal tract, lungs, and skin surface. Here they remain until they are completely destroyed.
The main difference is their relationship to microphages - they have the ability to fight pathogens of microscopic size. Cells act as a shield against infection by dangerous pathologies. The presence of inflammation leads to the activity of cells that act against parasites in the blood.
Upon contact with a pathological microorganism, the eosinophil is destroyed and encloses it in a cocoon, preventing further development and spread throughout the body. After the pathogen is enclosed in a cocoon, other cells of the leukocyte group enter into the fight. Eosinophils are responsible for the body's response to the presence of external or internal stimuli. Such a reaction can provoke allergies or become dull in response to external factors.
Eosinopenia is a decrease in the level of eosinophils in the blood to a critical level. A decrease in the parameter can be caused by several internal or external factors. A person more often experiences an increase in this indicator, which is called eosinophilia. The reverse process develops in isolated cases under the influence of various factors.
Reasons for decrease or increase
Normal value in peripheral blood: 120–350/µl. Their share in the leukocyte formula normally accounts for 1–5%. In the analysis of peripheral blood, eosinophils are increased in adults due to allergic diseases and parasitic (helminthic and protozoonotic) invasions. Eosinopenia is a decrease in the absolute or relative number of eosinophils in the peripheral blood. Observed in the initial stage of inflammation.
Eosinophilia in peripheral blood analysis is characteristic of the following conditions:
- Asthma. At the same time, eosinophils are not only elevated in the blood, but are also contained in the mucus of patients, forming Charcot-Leyden crystals in bronchial secretions.
- Helminth infections. Broad tapeworm, echinococcus in the liver, liver fluke, roundworms, pinworms, toxocara, pork and bovine tapeworms cause increased formation of eosinophils in the myeloid lineage of hematopoiesis. They migrate from the bloodstream to the localization of the helminth.
- Protozoonoses are diseases caused by protozoa. Protozoa include Leishmania, Giardia, Toxoplasma, dysentery amoebas, Balantidia, etc.
- Hay fever. This is an allergic runny nose caused by the flowering of certain plants.
- Angioedema of the larynx.
- Allergic dermatoses (atopic dermatitis, psoriasis, erythema multiforme exudative, urticarial rash, eczema).
- Drug allergies.
- Erythematous gastroenterocolitis. Erythema of the gastric and intestinal mucosa are accumulations of eosinophils. In a blood test, these cells will also be elevated.
- Leukemia and lymphoproliferative diseases.
- Rheumatoid connective tissue diseases: periarteritis nodosa, autoimmune arthritis, systemic vasculitis.
- Immunodeficiencies.
- Errors in the determination of eosinophils: the laboratory assistant mistook neutrophils with eosinophilic granules for eosinophils. If the number of neutrophils is reduced against the background of eosinophilia, it is necessary to retake the analysis.
- Oncological diseases.
- Lung diseases: sarcoidosis, histiocytosis.
- Acute phase of chronic infectious diseases: mononucleosis, tuberculosis.
- Viral infections in people prone to allergies. At the same time, an absolute and relative increase in the number of lymphocytes is also observed.
- Scarlet fever in children.
- Infections with cytomegalovirus or Epstein-Barr virus, fungal infections. Eosinophilia is combined with monocytosis.
- Menstrual period. Blood tests may show mild eosinophilia. After ovulation, the number of eosinophils drops, reaching a minimum at the end of the cycle.
Eosinopenia is observed in peripheral blood under the following conditions:
- Drug-induced or endogenous hypercortisolism. As is known, glucocorticoids inhibit hematopoiesis.
- Radiation damage to the bone marrow, including after radiation therapy.
- Cytostatic therapy. Eosinophils in the blood are reduced due to the suppression of hematopoiesis.
- Hypo- and avitaminosis of folic acid and cobalamin.
- Post-infarction state.
- Septic conditions.
- Endocrine pathologies.
- Leukemia.
- Stress: causes suppression of hematopoiesis.
- Gallstone disease, inflammation of the pancreas.
Causes of eosinopenia
Cell levels can change several times during the day. The effect is exerted by the cortisol present in the body. Sharp jumps in the indicator can be observed in absolutely healthy people. The difference can occur with the presence of serious values.
The size of an eosinophilic cell ranges from 12 to 17 µm. The composition contains granules with a specific protein. During activity, the number of granules decreases.
Scientists identify the following causes of eosinopenia:
- Infection with a purulent inflammatory process occurring with the presence of sepsis. The group of mature leukocyte genomes decreases, which is accompanied by a predominance of maturing leukocytes with a gradual decrease in level.
- Inflammation at the initial stage occurs with a decrease in the level in the blood.
- It can provoke an acute attack in the area of the appendix – appendicitis.
- Pancreatic disease.
- Gallstone disease in the acute phase.
- The patient's condition on the first day after myocardial infarction.
- A low level of the parameter is observed in case of poisoning with salts of heavy metals - vapors of mercury, cadmium, bismuth, arsenic, thallium, lead.
- Pathology in bone marrow tissue, which is accompanied by a natural decrease in the production of blood cells.
- A pathological process with a sharp decrease in the parameter is observed while taking myelotoxic medications.
- Irradiation with gamma rays during oncology changes the structure of the blood.
- Anemia caused by vitamin B12 deficiency.
- A state of shock caused by pain or other external factors.
- Stressful situations over a long period of time can cause qualitative disturbances in the composition of the blood flow.
- Pathologies in the area of the adrenal glands.
- Leukemia at the initial stage of formation or stage of acute growth throughout the body.
- For SLE (systemic lupus erythematosus).
- Kaposi's eczema of the herpetiform type.
- Rapidly developing exanthema.
- Diathesis of the neuro-arthritic form.
- Tuberculosis in lung tissues in the disseminated stage.
Any factor of an internal or external nature can provoke the development of eosinopenia. Therefore, doctors advise closely monitoring your health and undergoing regular medical examinations.
Normal indicators
When studying the main biological fluid of a person, hematologists always pay attention to such components and count them. In the structure of leukocytes they have an extremely low concentration - 0.5-5%.
The normal blood level may differ slightly by age, but does not depend in any way on gender.
The following table reflects the acceptable indicators:
From 16 days to 1 year
The norm for women and men is 1-5%. Acceptable values in absolute numbers are 120-350 cells per microliter of blood. Elevated values are called eosinophilia, and low values are called eosinopenia.
Development of the disease in childhood
In children, an acute inflammatory process at the initial stage can provoke the formation of eosinopenia. All genomes are directed to the pathogenic focus, which leads to a decrease in the rate. The level is gradually restored naturally.
Eosinopenia is often diagnosed without the presence of concomitant factors - diseases or areas of inflammation. In childhood, a short-term decrease in the parameter is often observed. Transient eosinopenia is typical for children from one to 12 years of age. Doctors say that this is a normal state of a child’s body, but only in the absence of concomitant pathological symptoms.
Blood with a deficiency of eosinophilic genomes may indicate that the child has a serious illness - Down syndrome. This also occurs in newborns born prematurely and with a number of pathologies of an infectious nature.
Danger is present when the parameter level is low for a long time. This requires an extensive examination of the body with consultation of a specialist doctor.
Eosinophils and monocytes are elevated in the child
The normal limits for reading leukocytes in a child are somewhat different from adult norms:
- monocytes - from 3 to 12% after birth, the upper norm increases to 15% in the first weeks, before a year it decreases to 10%, and after that it is equal to adult (3 - 9%);
- eosinophils - the percentage rate is the same as in adults (up to 5%), but the absolute amount in an adult is not more than 0.4 x 10⁹ per 1 liter, and in a child - 0.7 x 10⁹/l.
Important! When interpreting the results, not only age-related, but also daily fluctuations are taken into account. At night the indicators are higher, and during the day they decrease noticeably.
Most often, eosinophils and monocytes increase in children for the following reasons:
- Worm infestations, other parasitic infections.
- Allergic reactions.
- Staphylococcal sepsis.
- Scarlet fever, chickenpox, whooping cough.
- Any infections, including fungal infections.
Such a shift in the leukogram can warn of more serious pathologies, even malignant processes. But such cases are quite rare; usually, there are no serious illnesses behind the temporary change.
Important to remember! As pediatricians note, changes in the level of leukocytes in babies often provoke teething or any condition with an increase in temperature.
An objective picture is provided by dynamic observation during illness. If the average age norm is exceeded once, a repeat analysis is required.
It is impossible to establish a diagnosis even with the most accurate, detailed blood test. A separate level of lymphocytes, neutrophils, monocytes, eosinophils and basophils in the blood is not informative. When diagnosing, the ESR indicator in dynamics, all symptoms, complaints, the patient’s medical history, and the results of other laboratory tests are taken into account. The result of the analysis in an adult or child only helps to clarify the cause of the ailment or to suspect the presence of a hidden pathology.
Eosinopenia in women during pregnancy
A reduced granulocyte count in a pregnant woman is normal. Doctors associate this phenomenon in the bloodstream with a sharp decrease in the body’s immune functions during pregnancy. The second reason is considered to be a sharp increase in blood volume with signs of severe liquefaction.
After the birth of a child, a maximum decline in the eosinophilic parameter is recorded in the female body. This is caused by a state of extreme stress, accompanied by muscle strain and emotional imbalance. Childbirth is a difficult experience for a woman, so changes in blood flow are inevitable. Everything returns to normal after 2 weeks. Taking hormonal contraceptives immediately after childbirth leaves granulocyte counts low.
Therefore, eosinopenia against the background of normal levels of other blood elements in pregnant women is not considered a dangerous phenomenon. When the entire leukocyte count decreases, a full examination is required to find the cause of the pathology. The absence of leukocytes reduces the body's resistance to external stimuli. This condition poses a certain threat to the woman and to the unborn child.
What are eosinophils capable of?
The study of eosinophils has been going on for almost two centuries, but new biologically active substances with which the cytoplasm and membrane of these cells are “stuffed” are still being discovered.
There are dozens of enzymes, mediators of the immune system, signaling molecules for apoptosis (programmed cell death), and numerous receptors (for cytokines, immunoglobulins, chemotaxis molecules).
Participation in processes
All this suggests that eosinophils are multifunctional cells involved in a wide range of biological processes:
- The high cytotoxic potential of eosinophils makes them one of the most aggressive inflammatory cells. The destruction of foreign (and sometimes one's own) cells occurs due to the action of enzymes (alkaline proteins, peroxidase, neurotoxin). In addition, eosinophils produce an oxygen metabolite that is toxic to microbes. Its interaction with antibodies directed against foreign cells helps activate the destructive potential of the eosinophil;
- Eosinophils are capable of phagocytosis. The phenomenon of “devouring” foreign agents by immune cells was discovered by I.I. Mechnikov, for which the scientist received the Nobel Prize in 1908. Of course, eosinophils are not as actively involved in phagocytosis as macrophages, which are even called “scavengers” of the body. However, they too, migrating to the site of inflammation, absorb small foreign antigens there. At the same time, they not only capture the “enemy”, but also completely split it, using their enviable enzyme arsenal;
- In recent years, it has been discovered that eosinophils can be classified as cells occupying an intermediate position in the system of specific (lymphocyte) and nonspecific immune responses. During bacterial invasion, receptors appear on their membrane that bind unwanted agents. In addition, parts of foreign cells are “exposed” by eosinophils on their membrane for a more effective and specialized attack from an evolutionarily “more modern and accurate weapon” - lymphocytes;
- The eosinophil can be called the “headquarters” for regulating the immune response. These cells secrete about 30 immune modulators. These include pro-inflammatory agents (interleukins, tumor necrosis factor), and the anti-inflammatory group of interleukins, and immunosuppressants. In addition, eosinophils trigger enzymatic reactions, during which the death (apoptosis) of one of the T-lymphocyte populations is accelerated, causing their deactivation. Thus, the eosinophil is capable of not just “cleaning up garbage,” but also of “dictating” response options to a more evolutionarily younger system of specific immunity.
So, at present, traditional ideas about the role of eosinophils in the pathogenesis of allergies and parasitic infestations have expanded significantly.
It turned out that these unique cells regulate the mechanisms of both immune systems (specific and nonspecific), playing a significant role in the response to bacterial and viral infections, and in antitumor immunity. Why does the eosinophil count deviate from the norm?
Signs of the presence of pathology
Eosinopenia as a disease does not exhibit pronounced symptoms that would characterize it. Deviations from the norm in the granulocyte series can be detected based on the signs of the disease that provoked this condition. A number of factors can lower blood cell levels.
Doctors identify the following symptoms:
- Inflammations and pathologies of an infectious nature with purulent inclusions occur against a background of high body temperature, increased sweating, a sharp deterioration in health and chills.
- Diseases of the pancreas are characterized by sharp spasms in the epigastric zone (under the left hypochondrium). There is severe vomiting syndrome with high body temperature. The surface of the skin acquires a yellowish tint.
- Acute appendicitis occurs with symptoms similar to pancreatic pathologies. The difference lies in the localization of pain - this is the umbilical area. Spasms are sudden.
- Oncology is asymptomatic for a long time. The first signs appear when the tumor is large and has metastatic growths. The temperature remains at 37-38 degrees. The skin becomes pale. A person suddenly loses weight and experiences constant dizziness. He may suddenly lose consciousness for a few seconds or minutes. The gums bleed constantly, and nosebleeds are possible. Foreign inclusions of unknown etiology appear on the skin. There is an increased tendency to bruise without good reason. The lymph nodes increase in volume, and pain is felt when pressed.
Lymph node examination
If you have suspicious symptoms, you should consult a doctor for advice. An examination of the body will allow us to identify the cause of a sharp decrease in the level of granulocytes and begin treatment in a timely manner.
How is the disease treated?
This condition is detected by performing a general blood test, the results of which reveal an increased number of eosinophils. Signs of anemia are also recorded - a decrease in hemoglobin and the number of red blood cells. To identify the cause of the disease, a biochemical blood test, a stool test for helminth eggs, and a urine test are performed. The main way to diagnose allergic rhinitis is to analyze the secretions secreted by the mucous membranes of the nose.
It is necessary to conduct an X-ray examination of the lungs if there are indications for this; in case of rheumatism, a puncture of the affected joint is performed. There is no treatment for such an independent disease as eosinophilia.
The cause of this condition must be determined and eliminated.
The choice of drugs that treatment will include depends on the underlying disease, the presence of concomitant pathologies and the general condition of the body. For drug-induced eosinophilia, the main method of therapy is to discontinue previously prescribed medications.
Diagnosis of the pathological condition
An imbalance in the composition of blood elements can be identified through a blood test. The procedure is carried out in the morning. You are not allowed to eat or drink before the event. The last meal is 8-10 hours before.
To ensure an accurate diagnosis, the patient is recommended to follow a number of necessary rules:
- 1-2 days in advance you need to eliminate tea, coffee and alcohol;
- plain water without gas is allowed;
- fried, fatty foods should be excluded;
- Seasonings and smoked meats are also not recommended to be taken 2-3 days before blood sampling;
- when taking medications, you need to warn your doctor and laboratory assistant - this will be indicated in the diagnostic sheet;
- physical activity is prohibited;
- It is necessary to exclude moral overexertion and stress;
- You should not smoke before the blood collection procedure.
The completed recommendations will allow you to conduct a high-quality examination with a minimum of error. A correct diagnosis will speed up the healing process.
Doctors take into account an important point in the decrease in granulocytes - the period of ovulation. At this time, there is a high level of progesterone, which contributes to a natural decrease in eosinophils. A blood draw at this point will indicate the presence of eosinopenia. The same effect will occur under stress and overwork. This requires repeating the procedure.
The norm of eosinophils in the blood is 1 - 5
For adults, the normal content of eosinophils in a clinical blood test is considered to be from 1 to 5% of the total number of leukocytes.
Eosinophils are determined by flow cytometry using a semiconductor laser, and the norm in women is the same as in men. More rare units of measurement are the number of cells in 1 ml of blood. Eosinophils should be from 120 to 350 per milliliter of blood. The number of these cells can fluctuate during the day due to changes in the functioning of the adrenal glands.
- In the morning and evening hours, there are 15% more eosinophils compared to normal
- In the first half of the night 30% more.
For a more reliable analysis result, you should:
- Take a blood test in the early morning hours on an empty stomach.
- For two days you should abstain from alcohol and excessive consumption of sweets.
- Eosinophils may also increase during menstruation in women. From the moment of ovulation until the end of the cycle, their number decreases. The eosinophilic test of ovarian function and determination of the day of ovulation is based on this phenomenon. Estrogens increase the maturation of eosinophils, while progesterone decreases it.
What function do they perform in the body?
Eosinophils perform a variety of functions in the human body. For this reason, most of them are similar to the functions of other blood cells. They take part in many inflammatory processes, and most of all in those of allergic origin. In addition, eosinophils have a specific role during organ formation.
The following functions of the presented cells are distinguished:
- being in the place where inflammatory processes take place;
- preventing the negative impact of potentially hazardous substances;
- cell destruction;
- antiparasitic and bactericidal activity.
Eosinophils in the blood can have not only a positive effect, but also a negative one. They prevent potentially dangerous microorganisms from entering the human body, but there are cases when they are associated with pathological changes. A striking example is Loeffler's disease.
What leads to eosinophilia
When eosinophils are elevated in the blood, the reasons lie in the body’s allergic readiness. This happens when:
- acute allergic conditions (Quincke's edema, urticaria, hay fever)
- allergies to medications, serum sickness
- allergic rhinitis
- skin allergies (contact dermatitis, eczema, atopic dermatitis, pemphigus vulgaris)
- helminthiasis (see signs of worms in humans)
- parasitic diseases (toxoplasmosis, chlamydia, amebiasis)
- acute infections and exacerbations of chronic ones (tuberculosis, gonorrhea, infectious mononucleosis)
- systemic pathologies (systemic lupus erythematosus, eosinophilic fasciitis, rheumatoid arthritis, periarteritis nodosa)
- lung pathologies: bronchial asthma, fibrosing alveolitis, sarcoidosis, eosinophilic pleurisy, histiocytosis, Lefler's disease
- lesions of the gastrointestinal tract: eosinophilic gastritis, eosinophilic colitis
- blood tumors (lymphogranulomatosis, lymphomas)
- malignant neoplasms.
Next, a consultation with an allergist is scheduled:
- For allergic rhinitis, swabs are taken from the nose and throat for eosinophils.
- If bronchial asthma is suspected, spirometry and provocative tests (cold, with Berotec) are performed.
- The allergist then carries out specific diagnostics (determination of allergens using standard serums), clarifies the diagnosis and prescribes treatment (antihistamines, hormonal drugs, serums).
An infectious disease specialist treats helminthic infestations, parasitic diseases and acute infections. A pulmonologist will deal with pulmonary problems.
Classification
Clinicians distinguish three degrees of development of eosinophilia in humans:
- small. The level of these blood cells increases by no more than 10% of their total number;
- moderate. The level increases by 10–20%;
- high. Increase in blood cell content over 20%.
Depending on the reasons that provoked the progression of this condition, as well as the localization of manifestations, the following forms of eosinophilia are distinguished:
- pulmonary eosinophilia;
- eosinophilia with progression of oncological pathologies;
- allergic nature;
- eosinophilic fasciitis;
- eosinophilia in asthma;
- eosinophilic gastroenteritis;
- eosinophilic cystitis;
- parasitic eosinophilia.
Eosinophilia
Structure and activity of eosinophils
Eosinophils are slightly larger in size than neutrophils, reaching 12-14 microns. Their core consists of 2-3 parts, the cytoplasm is dotted with orange-pink inclusions. Color is related to the exposure of blood cells to the dye during study; this type of leukocyte absorbs eosin. Most of their functions are protective.
- Participation in the allergic process. Inflammation and increased blood supply during allergies are caused by histamine and other substances that are released by basophils that encounter an enemy. Attracted by the signal, eosinophils move to the site of inflammation and enter into a fight. At the same time, they can both inactivate histamine and heparin and release them, which allows regulating the process.
- Phagocytosis is the absorption of bacteria and foreign particles. Eosinophils play the role of microphages: they can only capture small cells, and in general, phagocytosis is not their main job.
- Fight against parasites. By activating the receptors, eosinophils cause the cells surrounding the worm to be destroyed. Thus, they block the invader and attract more aggressive participants in the immune system. The granules of the representatives of leukocytes themselves contain a protein that is harmful to helminth larvae and peroxidase that is aggressive towards them.
- Preventing antigens from entering blood vessels.
Half of the mature eosinophils settle in the tissues within an hour. Cells do not live long in the blood, about 3-8 hours. Outside the vascular bed, they can exist for up to 12 days.
Place among blood cells
Leukocytes are the body's natural protectors. Their structure and ability to absorb different dyes during microscopy allowed researchers to divide cells into groups, and the functions of each of these groups may be special. Granular leukocytes include neutrophils, eosinophils, and basophils; They are united by segmentation of the nucleus and granules in the cytoplasm. Lymphocytes and monocytes are considered nongranular. All white blood cells try to be the first to meet any invader, so the body intensively replenishes their number during infections, allergies or parasite invasions. Eosinophils are no exception.