How to find out the gender of a child using a table?
According to legend, Chinese gender determination table
child was found in an ancient royal tomb in China. It predicts the gender of the child based on the Chinese lunar calendar.
In this case, you need to know the age of the mother when conceiving the child.
and
the month of conception
to determine whether you are having a girl or a boy.
There is no scientific evidence to prove whether this method works, but you can test it on your friends and family.
Gender of the child by date of conception
According to this method, the sex of the unborn child is determined
by the date of conception
and depends on the type of sperm.
It is believed that Y sperm, which will lead to the birth of a boy, is faster and less hardy than sperm with the X chromosome, which is slower but more persistent.
Thus, if conception occurred 2-3 days before a woman ovulates, then you are more likely to give birth to a girl
.
If conception took place directly on the day of ovulation or shortly before it, then the likelihood of having a boy is higher
.
The day of ovulation can be determined by measuring your basal temperature or using home ovulation tests.
Ultrasound at 11 weeks during pregnancy
- If a transabdominal ultrasound is planned, you need to drink about 0.5 liters of still water 60-40 minutes before the procedure.
- When examining with a transvaginal probe, no preparation is required.
- But on the day of the examination, in the morning or evening before the procedure, you should try to empty your bowels.
- On the day of diagnosis, you should try not to eat foods that cause increased flatulence.
- You are allowed to eat before the examination.
- At the end of the procedure, screening is done and a research protocol is drawn up.
Calculate the sex of a child by blood
According to this theory, the gender of the unborn child can be determined based on
the renewal of the parents' blood
. It is believed that in women the blood is renewed once every 3 years, and in men - once every 4 years. The gender of the child is determined by which parent has “fresher” blood.
To calculate the gender of the child, you need to divide the age of the woman by 3, and the age of the man by 4.
. The one who has the smaller remainder (younger blood) will have a child of that gender.
For example, a woman is 26 years old and a man is 28 years old. If we divide 26 by 3 we get 8.6, and if we divide 28 by 4 we get 8. Since the remainder of a woman (8.6) is greater than that of a man, the probability of having a boy is greater.
It is also worth remembering that in the case of blood donation and transfusion, operations, childbirth and other blood losses, it is worth taking the date of the last blood loss.
Determining the sex of a child using the “Blood Renewal” method
Embryogenesis
Between 4 and 5 weeks of fetal development, the formation of primary gonads occurs. The karyotype of a healthy person consists of 44 autosomes and 2 sex chromosomes. At the genetic level, the identity of the embryo is determined by the set of sex chromosomes X and Y. Despite the fact that the Y chromosome contains only about 2% of the haploid genome, it contains genes that control sex determination. When an egg is fertilized, the genetic makeup of the unborn child is formed. When an egg is fertilized by a sperm carrying an X chromosome, the genetic sex of the unborn child is female (set of sex chromosomes XX); when an egg is fertilized by a sperm carrying a Y chromosome, the genetic sex of the unborn child is male (set of sex chromosomes XY). Currently, the localization of about 100 genes on the Y chromosome has been determined. The main ones are: SRY (sex determining region Y chromosome), DAX-1 (dosage-sensitive sex-reversal), TDF (testis determining factor), ZFY, TSPY (testis specific protein), AZF (azoospermia factor), HY- histocompatibility factor gene, GBY gene [Chernykh V.B. et al., 2001; Lopez M et al 1995; Cantrell MA et al, 1998]. For the formation of the sex gonad, which is characteristic of men, the presence of the Y chromosome is necessary. It has been established that the gene responsible for the synthesis of a specific surface protein, the HY antigen, is located on the Y chromosome.
So, with a set of sex chromosomes containing a Y chromosome, a testicle is formed, but a full-fledged testicle is formed only in the presence of X and Y chromosomes. For the correct creation of a testicle, the presence of at least two X chromosomes is necessary. A full-fledged female gonad is formed with a karyotype of 46XX.
Subsequently, both internal and external genitalia are formed according to one type or another. The anlage of the internal genital organs are 2 pairs of ducts: Müllerian and Wolffian, which open in the urogenital sinus. The formation of internal and external genitalia in the fetus is an active process. Sertoli cells in the embryonic testicles begin to actively synthesize a factor that suppresses the development of Müllerian ducts in a male fetus. Leydig cells in the testes increasingly secrete testosterone under the influence of which the Wolffian ducts differentiate into the seminal vesicles, vas deferens and epididymis. In the absence of the active influence of a factor that inhibits the Müllerian ducts, the Müllerian ducts mature, further differentiating into the uterus, upper part of the vagina and fallopian tubes. The Wolffian ducts regress. The external genitalia and urethra in fetuses of both sexes develop from a common anlage - the urogenital sinus and genital tubercle, genital folds and elevations.
Formation of internal genital organs
Starting from the 10th week of intrauterine development, the fetal testicle, first under the influence of human chorionic gonadotropin (CG), then its own luteinizing hormone (LH), synthesizes a large amount of testosterone, which affects the formation of the external genitalia. In addition to testosterone, differentiation of the external genitalia also requires exposure to the active metabolite of testosterone - dihydrotestosterone, which is formed directly in the tissues under the influence of the enzyme 5-alpha reductase. Under the influence of hormones, the urogenital sinus is transformed into the prostate and the inner part of the urethra. The urethral folds and ridges are transformed into the penial urethra and the cavernous bodies of the penis. The genital tubercle forms the head of the penis. The meatus of the head is formed by retraction of epithelial tissue, which then connects to the urethral groove in the area of the scaphoid fossa. At the end of the first trimester, the final formation of the genitals occurs.
Formation of external genitalia
Thus, by the time of birth, the child’s reproductive apparatus is fully formed. In healthy children, the sex of the gonads, the structure of the internal and external organs, i.e. the phenotype or morphological sex fully corresponds to the karyotype, i.e. genetic sex.
In the postnatal period of life, the child still has to go through a very important stage of sexual determination - puberty, the period of puberty. Consequently, only towards the end of puberty does the formation of the reproductive apparatus of a healthy person complete. From this time on, a person is able to perform the main biological function - to reproduce his own kind.
1. Pathology of genital formation
The main cause of impaired sex determination is chromosomal or more subtle genetic abnormalities. In this case, there may be a pathology in the number or structure of sex chromosomes, or direct damage to the genes responsible for puberty. Puberty can also be disrupted due to pathology of autosomes, or rather, genes localized on autosomes but directly involved in puberty. Much less often, malformations of the reproductive apparatus in a child can be caused by a violation of the hormonal balance of the pregnant woman (taking hormonal drugs, hormonally active tumors) and (or) the hormonal function of the placenta.
The impact of the above unfavorable pathological factors that disrupt the normal processes of determining gender can go in two ways:
- Pathological factors prevent the formation of a full-fledged gonad, which in turn disrupts the processes of creating genitalia.
- The development of the gonad is not impaired. In these cases, the pathology of the reproductive system may be caused by a congenital defect in testosterone synthesis or dihydrotestosterone metabolism, impaired sensitivity of target tissues to the action of sex hormones, or an increase in the level of sex hormones of extragonadal origin.
1.1 Gonadal agenesis
Exposure to unfavorable factors in the early stages of embryogenesis can prevent the development of the gonad. Most often, gonadal agenesis is the result of a pathology (change in the number or structure) of sex chromosomes; less often, such patients have a normal set of sex chromosomes for women or men (pure gonadal agenesis).
For any reason that caused the state of gonadal agenesis, the clinical picture of the disease will be largely the same. In place of the gonads, where the ovaries are usually located, these patients have formations that are whitish strips of connective tissue - “streak”. Such a “gonad” is formed before the differentiation of the sexual anlage into a testicle or ovary begins. It goes without saying that such a “gonad,” which does not actually contain functional elements of the gonad, is not capable of secreting sex hormones either during intrauterine life or in subsequent years. This explains the presence of a female phenotype and pronounced symptoms of hypogonadism in all patients with gonadal agenesis. In this case, as a result of the absence of a functioning gonad, the formation of internal and external genitalia is due to the autonomous tendency of the fetus to feminize. All patients have an atrophic uterus with tubes and a narrow vagina. The external genitalia are always female, only the labia minora may be underdeveloped. When such children are born, there is never any doubt about their belonging to the female gender. In childhood, such “girls” do not have obvious symptoms of the disease indicating a pathology of the sexual creation. Pathology of the reproductive system will appear much later. Children will begin to feel uncomfortable with the lack of secondary sexual characteristics. The symptoms of hypogonadism in such patients are pronounced: the mammary glands do not develop, menstruation does not occur, and there is no sexual hair growth. (Kasatkina E.P., 1979, Grumbach MM, 1989).
1.2 Gonadal dysgenesis
A similar pathology occurs at later stages of embryogenesis, at the moment when the gonad begins to form from the reproductive anlage. However, exposure to unfavorable factors prevents the final development of a full-fledged reproductive gland.
With gonadal dysgenesis, in contrast to agenesis, the clinical manifestations of gonadal damage will be different.
1.2.1 Ovarian dysgenesis
The most common cause of ovarian dysgenesis is the mosaic karyotype 45X0/46XX. A cell clone with a normal set of sex chromosomes for a woman guarantees differentiation of the sexual anlage into the ovary. The presence of a pathological cell clone prevents the final maturation of a full-fledged gonad. The degree of underdevelopment of the gonad depends on the percentage of normal and pathological cell clones and their distribution in the body. If the pathological cell clone predominates, the gonad will resemble a connective tissue strip during gonadal agenesis, but with more pronounced cellular elements of the cortical layer. If the normal cell clone predominates, the gonad may represent a hypoplastic ovary.
In some patients with this pathology, a normal female karyotype 46XX is detected.
So, with ovarian dysgenesis, the phenotype of patients is always correct female. Consequently, in childhood there are no obvious symptoms of gender pathology. Only later, against the background of puberty, hypogonadism is revealed.
1.2.1 Testicular dysgenesis
In contrast to previously described pathologies, testicular dysgenesis is clinically characterized by a mixed structure of the genitals.
The cause of intrauterine damage (underdevelopment) of the testicle in some patients with gonadal dysgenesis is a change in the number of sex chromosomes. In some clinical variants of the disease, mosaicism of the 45X0/46XY form is detected or suspected based on clinical manifestations. In rare cases, pronounced structural changes in sex chromosomes are detected. In some patients, the cause of intrauterine testicular damage cannot be identified: the set of sex chromosomes in these patients is normal for healthy men. However, the presence of a familial disease in some clinical variants suggests a genetic pathology. With a significant degree of damage to the testicle, the gonad with testicular dysgenesis can be a poorly differentiated tissue, externally resembling a “streak”, but with a slightly higher content of testicular tissue. In some patients, the gonad is more differentiated and visually appears as a hypoplastic testicle with morphological signs of intrauterine damage.
The phenotype of such patients is almost always closer to female; the internal genitalia are always female. The female structure of the internal genitalia (presence of the uterus, tubes and upper part of the vagina) in these patients is due to underdevelopment of Sertoli cells and deficiency of anti-Mullerian substance. The absence of the vas deferens and the female structure of the external genitalia in these patients is due to testosterone deficiency during intrauterine life. The small amounts of testosterone that these “gonads” synthesize are only capable of forming a virilized clitoris (severely underdeveloped penis), because The genital tubercle is most sensitive to the action of androgens during intrauterine life. In the postnatal period of life, such testicles turn out to be completely incompetent, i.e. there is severe hypogonadism and infertility. A similar pattern of gonadal damage is observed in the following clinical variants of the disease: Shereshevsky-Turner syndrome with hermaphrodite genitalia, pure testicular dysgenesis, rudimentary testicle syndrome.
A rare variant of intrauterine testicular disorder is a condition where only the morphogenetic function of the embryonic testicles is damaged. In this case, only anti-Mullerian substance deficiency occurs more often. The boy's reproductive apparatus, namely the genital ducts and external genitalia, are formed in such patients as in men, but at the same time there is a well-developed uterus and tubes. Typically, such a defect is detected by chance (during surgery). Secondary sexual characteristics in such patients are always well developed (testosterone function is not impaired), and some patients are fertile. A clinical variant of this disorder is Reyer's syndrome.
1.3 Intrauterine testicular atrophy
In a fetus with a normal karyotype, testicular atrophy occurs at different stages of intrauterine development. Depending on the timing of the damage to the testicles, different types of sex disorders are formed. Thus, if the testicles are damaged in the early stages (up to 12 weeks) of intrauterine life, a clinic of hermaphroditism is formed. If the testicles are damaged shortly after 12 weeks - microphalus. Otherwise, the genitals (internal and external) are developed correctly. Atrophy of the gonads in later stages of fetal development does not affect sex differentiation: the genitals are formed in a standard manner, the penis is of normal size. In all types of intrauterine testicular atrophy, pronounced hypogonadism occurs against the background of puberty.
Typically, with testicular dysgenesis, the gonads on both sides are underdeveloped to the same extent. However, asymmetric development of the gonads is quite often observed. In this case, on the one hand there is a dysgenetic testis, on the other there is a rudimentary gonad or the second gonad is completely absent - mixed testicular dysgenesis. In patients with asymmetrical arrangement of the gonads, asymmetric development of the internal genitalia is quite often observed. In the presence of a uterus, there is a tube on the side of the rudimentary gonad, and on the side of the testis, only the vas deferens or ducts of both sexes can be developed simultaneously.
1.4 Development of the mixed gonad
In some patients, the pathology manifests itself in the fact that both zones of the genital anlage develop into gonads, i.e. elements of both gonads are simultaneously formed from the reproductive anlage. The correct female karyotype (46XX) is more often identified, or much less often the correct male karyotype (46XY). Sometimes a mosaic karyotype occurs.
1.5 Prenatal testosterone deficiency
In some patients with a normal karyotype (46XY) and male gonads, the pathology may be due to testosterone deficiency during intrauterine life. Testosterone deficiency may be due to a congenital defect in testosterone steroidogenesis or a congenital deficiency of gonadotropin hormones (GTG).
The defect in testosterone synthesis in most patients is the result of a deficiency of one of the five enzyme systems involved in the synthesis of the hormone in the adrenal glands and gonads. The gonads of such patients, as a rule, are normally developed and do not have morphological signs of damage. The condition is genetically determined, the inheritance biotype is autosomal recessive.
Testosterone deficiency, which occurs in patients with similar defects, during intrauterine life is the cause of the formation of mixed genitalia and hypogonadism. In most patients, the phenotype approaches that of a woman: the penis is underdeveloped, the scrotum is split, there is a blind-ending vagina that opens into a hypospadated urethra. During puberty, secondary sexual characteristics do not develop.
Much less often (with partial enzyme deficiency) the phenotype of patients approaches masculine. Against the background of puberty, such patients may experience spontaneous development of secondary sexual characteristics, as in men. It is noteworthy that in the majority of patients with a congenital defect in testosterone synthesis, gynecomastia of unknown etiology develops against the background of puberty.
Intrauterine testosterone deficiency, in addition to a violation of its synthesis, can be caused by a congenital deficiency of luteinizing hormone (LH) or impaired sensitivity of the gonads to the action of LH. The secretion of testosterone by the Leydig cells of the fetal testes in the early stages of intrauterine life (the first three months) is regulated by human chorionic gonadotropin, and in later stages by fetal LH. Therefore, congenital LH deficiency or inadequate sensitivity of the gonads to the action of LH may be the cause of testosterone deficiency in the later stages of intrauterine life, when sex differentiation is completed and the corpora cavernosa are formed and the penis increases in size. This pathological condition is characterized by the presence of a microphalus; otherwise, the external genitalia are formed like those of a man. Subsequently, the patient develops symptoms of hypogonadism. The internal genitalia are formed according to the male type.
Thus, congenital testosterone deficiency contributes to the development of the clinic of false hermaphroditism or microphalus.
1.6 Inadequacy of testosterone action at the tissue level
This pathological condition is characterized by normal functioning of the testicles and sufficient levels of testosterone during intrauterine life and in subsequent years.
However, testosterone at the level of androgen-dependent tissues does not have a masculinizing effect. This may be due to two reasons: a violation of the sensitivity of the receptors of androgen-dependent tissues to testosterone and a deficiency of the enzyme 5α-reductase, which converts testosterone into its active form - dihydrotestosterone.
For any of these reasons, the lack of testosterone effect at the tissue level during fetal life prevents the development of a male phenotype.
Impaired sensitivity to androgens is the cause of a fairly common variant of false male hermaphroditism - testicular feminization syndrome.
With a complete loss of sensitivity to androgens, a female phenotype is formed. Against the background of puberty, secondary sexual characteristics of the female form are formed. The formation of secondary sexual characteristics of the female form can be explained by the fact that in such patients at the tissue level the competing effect of androgens is removed and under these conditions small amounts of estrogens can have a good feminizing effect.
With partial loss of sensitivity to androgens, mixed genitalia are formed. Against the background of puberty, such patients experience pronounced androgenization to varying degrees.
It should be noted that regardless of the structure of the external genitalia, the internal genitalia in patients are formed like those of men.
Impaired sensitivity to androgens is a genetically determined condition. There is a large percentage of familial cases. Diseases are always transmitted by women, carriers of a pathological gene, and only men get sick.
5α-reductase deficiency is also a cause of mixed genitalia. As a result of deficiency of the active form of testosterone (DHT), the external genitalia of the fetus are formed under the influence of an autonomous tendency towards feminization. The phenotype of such patients is closer to that of women. However, against the background of puberty, spontaneous development of secondary sexual characteristics often occurs.
1.7 High testosterone levels during intrauterine life of extragonadal origin.
Such pathological conditions are the cause of the formation of a common form of hermaphroditism - false female hermaphroditism.
The most common variant of false female hermaphroditism is congenital dysfunction of the adrenal cortex. Congenital dysfunction of the adrenal cortex is caused by pathology of autosomes that manage the enzymatic synthesis of steroid hormones of the adrenal cortex. The disease has a recessive type of inheritance. With this disease, there is a deficiency of enzyme systems involved in the synthesis of gluco- and meneralocorticoids. As a result of disruption of the synthesis of vital hormones, the level of ACTH sharply increases. In response to this, the adrenal glands hyperplasia and secrete in excess those steroids in the synthesis of which defective enzyme systems do not take part, i.e. androgens. Thus, the clinical symptoms of this disease are caused by a deficiency of vital hormones and excess androgens. In a female fetus, the excess content of androgens contributes to the virilization of the external genitalia. In this case, the male external genitalia or mixed genitalia are formed.
High levels of androgens during fetal life may result from the mother taking male sex hormones or from the presence of androgen-producing ovarian or adrenal tumors.
1.8 Taking progestin drugs and estrogens by the mother during pregnancy.
Taking such drugs during pregnancy can cause virilization of the female sex or feminization of the male sex.
Thus, in a genetic male fetus, mixed genital structure may result from the formation of a defective testicle, disruption of the hormonal function of the embryonic testicles, or disturbance in sensitivity to the effects of androgens. In this case, the formation of mixed genitalia occurs.
In a female fetus, the mixed structure of the genitals is caused by an excessive content of androgens during intrauterine life, most often of adrenal origin. In some patients, a mixed gonad is formed and, as a result, a mixed structure of the genitals.
Gender of baby by belly
If you
carry your baby low, you have a boy, if you carry it high, you have a girl
.
There is also an opinion that if the expectant mother has a pointed belly shape, she will have a boy, and a more rounded one, she will have a girl
.
However, according to experts, the shape of the abdomen is determined by the muscles, uterine tone and position of the child, and not by the gender of the baby.
According to the latest data, breast volume is the best indicator of the sex of the unborn child.
. Women carrying girls have larger breasts during pregnancy (an average of 8 cm) than women carrying boys (an average of 6.3 cm). This is because boys produce more testosterone and require more energy from the mother, which suppresses breast growth more.
Gender of the child according to ultrasound
© vadimguzhva/Getty Images
One of the most accurate methods for determining the sex of your baby during pregnancy is an ultrasound, or ultrasonography, which uses high-frequency sound waves to create an image of your baby inside your uterus.
An ultrasound is not performed to determine the sex of the child, but to find out whether the child is developing correctly.
Depending on the length of your pregnancy and the position of the fetus, your doctor can tell you for sure whether you are carrying a boy or a girl.
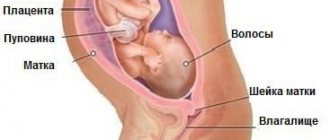
Why is an ultrasound performed in the first trimester?
During the period of bearing a child, each woman undergoes at least 3 ultrasound examinations. The first ultrasound is scheduled at the 11th week. The main purpose for which it is carried out is to confirm the presence of a fertilized egg in the uterus. The fact is that the fertilized egg does not always attach to the walls of this organ.
A pregnancy in which the fertilized egg is present outside the uterine cavity is called ectopic. It is very important to identify this complication in time. In case of ectopic pregnancy, a woman requires emergency medical care. This condition is dangerous to health due to internal bleeding.
When a fertilized egg is detected in the uterine cavity, the purpose of an ultrasound at 11 weeks is to confirm that pregnancy is developing. To do this, the fetus is examined and the functioning of its heart is assessed. If there is no embryo in the fertilized egg, doctors suspect a non-developing pregnancy of the anembryonic type. The woman is prescribed dynamic ultrasound control.
If there is an embryo and there are no contractions of its heart, specialists suspect that the pregnancy is not developing due to the type of fetal death. In such cases, another ultrasound examination is prescribed. It is carried out in order to confirm or refute a non-developing pregnancy.
Ultrasound is also done in order to promptly identify serious pathologies and chromosomal abnormalities. According to some indicators, one can suspect the presence of Down, Patau, and Edwards syndromes in the fetus. Thanks to early diagnosis, future parents receive timely information about the nature of the pathology, they have more time to think about the current situation and make a decision about the fate of the unborn child.
At what time can you determine the sex of a child?
Most often, the method of determining the sex of a child by ultrasound is most accurate
during the period from 18 to 26 weeks of pregnancy
. Although new ultrasound technologies can determine the sex of the child at an earlier period of 12-13 weeks.
Until 18 weeks of intrauterine development, male and female genital organs are more similar and therefore the likelihood of error is high. Later dates also make this task more difficult due to the tighter position of the fetus.
It is worth remembering that if the child is in an awkward examination position or crosses his legs, this may hide the genital area from observation.
When does this happen?
The question of when the child’s gender is determined is important for future parents. It would be correct to say that this happens immediately after conception. After all, it is in the first days that the zygote divides and a blastocyst is formed with a set of genetic material received from both parents. In the future, only the implementation of the program that is encoded in the chromosomes occurs.
The process of intrauterine development occurs in stages. The organs and systems of the future baby are formed in embryogenesis, i.e. at the very beginning of the individual path (ontogenesis). First, the germ cells divide intensively, subsequently forming tissues (ecto-, meso- and endoderm). And those, in turn, undergo complex differentiation with transformation into organs. The reproductive system goes through the following stages of development:
- Formation of the genital tubercle (6th week).
- Development of testes and ovaries (7th week).
- Synthesis of own sex hormones (week 8).
- Division into genital folds and labioscrotal tubercles (week 9).
- Obvious sexual characteristics: penis and scrotum in boys, labia and clitoris in girls (11th week).
Subsequently, further improvement of the external genitalia of the fetus occurs, which occurs under the influence of the hormone dihydrotestosterone. Girls have little of it, so the genitals practically do not change in appearance when compared to 8 weeks. And in boys, development goes further and at 12 weeks the formation of the foreskin of the penis occurs. At this time, the testicles are still in the abdominal cavity, and descend into the scrotum only at 7–8 months of gestation. In girls, the ovaries can be detected from 10 weeks of pregnancy.