Rubella is an infection that occurs as a result of a virus. Rubella infection occurs through airborne droplets. The disease has no age restrictions, however, it is most dangerous to get it during pregnancy, since the infection will be transmitted to the baby, which can cause pathologies from birth. To find out if you have the disease, you need to get tested for rubella during pregnancy.
Rubella symptoms
Once the virus enters, the incubation period lasts two to three weeks. After this, symptoms reminiscent of a cold appear:
- fever up to 38 °C;
- sore throat;
- redness of the eyes;
- signs of intoxication (nausea, weakness, etc.);
- aching joints;
- soreness of the occipital and cervical lymph nodes;
- conjunctivitis.
Two days later, a flat, pale pink rash appears that does not protrude above the skin surface. It is preceded by a rash on the palate, gradually moving to the tonsil area.
Nature of the rash
Localized small spots no more than 3-5 mm. In adult patients, including pregnant women, the spots tend to merge with each other. Initially, the rash appears on the face, then quickly spreads over the entire surface of the body: to the back, buttocks, stomach, legs and arms, with the exception of the palms.
The rash is usually not accompanied by itching and lasts from two to four days. In rare cases, up to seven days. Then it disappears without residual marks or peeling.
A little about the disease
Rubella is an infectious disease that can be contracted from a sick person through aerosols, or less commonly through toys and household items. After contact with a sick person, 15 to 25 days pass, then the first symptoms of the disease make themselves felt: headache, sore throat, weakness, enlarged lymph nodes. After 48 hours, the patient's body becomes covered with a rash, which first appears on the face and then spreads throughout the body.
Why is it so important to get tested?
The disease itself is not dangerous, but during pregnancy it can lead to fetal death or serious developmental defects. Therefore, doctors must know whether a woman has had this disease or not, and ask her to take a test for rubella. It is included in the list of mandatory TORCH tests for infections that are taken during pregnancy. Usually, a positive test for infection does not make anyone happy, but this is not the case. If a test for rubella shows that there is immunity to this disease, this is good, especially during pregnancy, because confirms that the woman is immune to rubella. We'll talk about this in more detail later.
The danger of rubella for a pregnant woman
Usually, a pregnant woman who has been in contact with a sick person is asked to take a rubella test, but every woman should undergo this test once during pregnancy. It is not always possible to determine that it is rubella based on symptoms; in 90% of cases it occurs like a normal acute respiratory infection, which is why testing for rubella is so important.
If during pregnancy before 16 weeks it is positive, i.e. confirms the presence of the disease, then the pregnancy is terminated. After 16 weeks, they look at the development of the fetus; the longer the period, the less likely it is that the child will become infected. If the expectant mother becomes infected in the 2nd or 3rd trimester, her child will lag behind in physical development. And if it is early, then his vision, hearing, nervous system will suffer, and heart pathologies will be discovered.
Types of rubella
- Classic – all of the listed symptoms and periods of the disease are pronounced.
- The erased form is characterized by partial manifestations. With elevated temperature and inflammation in the throat, the rash may not be observed.
- Asymptomatic , in which all typical signs are absent. Despite this, the rubella virus leaves lifelong immunity, just like in the classic version.
The last two forms are the most dangerous for others, since infected people do not suspect that they are the source of infection.
Some colds and allergic diseases, as well as measles and scarlet fever, have similar symptoms. Only an infectious disease specialist can make a reliable diagnosis, taking into account laboratory diagnostic data. If a woman has not had rubella, she must notify her doctor during the pregnancy.
Forecast
The consequences of rubella that occurs during gestation directly depend on the trimester in which the infection occurred. Based on this, events can develop as follows:
- infection with the virus in the first trimester in 80% of cases ends in the development of serious defects leading to fetal death; even if the woman continues to bear the child, the pregnancy is resolved by stillbirth;
- in 30% of women, the disease during pregnancy ends in spontaneous abortion;
- in 20% of cases, in case of failure to perform an abortion, intrauterine fetal death is recorded.
Based on statistical data, a disease detected in the early stages of gestation is an absolute indication for induced abortion.
If a woman was infected with the rubella virus in the second trimester, there is a chance of saving the baby’s life, but there is a high risk of developing dangerous anomalies. If the disease develops in the third trimester of pregnancy, the prognosis for the child is considered the most favorable.
Rubella during pregnancy: risks and complications
The Australian doctor N. Gregg first described the abnormal consequences for the fetus of rubella infection in the mother in 1941. The insidiousness of the rubella virus lies in the fact that it easily passes through the placenta. At the same time, it inevitably affects the fetus, adversely affecting its development.
It is most dangerous if a woman becomes infected in the first trimester, at the stage of embryo formation. This is the most unfavorable period, since the rubella virus damages the most important systems of the embryo. The most common triple lesion is called Gregg's triad. At the same time, in 95% of cases, a newborn has heart defects, in 85% - eye cataracts, and in 22% - deafness.
Other adverse effects on the fetus include:
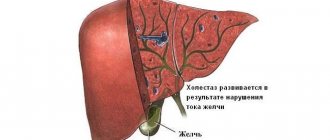
- change in blood formula;
- liver and spleen defects;
- congenital deformities;
- body weight is below normal;
- nervous system disorders.
Mental disabilities do not appear immediately. Developmental delays become noticeable only as the child grows older.
In addition to intrauterine defects, there are other complications, in particular, miscarriage and frozen pregnancy. After the twentieth week the situation changes dramatically. At this stage, rubella rarely has a negative effect on the baby.
Who takes this test
The following categories of people undergo this test:
- A woman who has or plans to have a child.
- A newborn baby whose mother may have contracted the virus during pregnancy (in which case both should be tested).
- Anyone with rubella symptoms.
- Healthcare workers.
- Students entering college.
- Some children with birth defects.
It is important for them to determine the presence or absence of immunity to the rubella virus. A positive response to IgG will indicate that the infection has left its mark on the person.
Probable methods of infection
The rubella virus is extremely contagious, especially through casual contact at home or in children's groups. The susceptibility of unvaccinated people is estimated at 90%, so if rubella is detected, quarantine is declared. A person releases the virus several days before the rash forms, throughout the entire period of illness, and for another week after recovery.
People are most likely to become infected through close contact with an infected person, for example, when living together in an apartment. The maximum likelihood of disease is observed during off-season periods. Epidemic outbreaks are recorded approximately once every 5 years.
At the same time, the rubella virus is highly sensitive to environmental influences and quickly dies when the temperature rises, in sunlight, or when disinfected with chlorine-containing agents.
In most cases, the source of infection is small children. Therefore, the risk of contracting rubella increases in pregnant women, those with younger children, or those in contact with children's groups at work. Especially when the baby and/or woman attend kindergarten, clubs, and sports clubs.
Diagnostics
After suffering from rubella, lifelong immunity remains in the body, preventing secondary infection. If a woman has already had rubella or been vaccinated, there is nothing to worry about during pregnancy.
If you do not have accurate information about childhood diseases, then you need to donate blood for rubella antibodies. However, you should not trust the memories of relatives. Viral diseases in childhood are often accompanied by a rash and have similar symptoms. The only true criterion can be the diagnosis recorded in the medical record.
Recently, doctors quite often note the asymptomatic and mild course of rubella, which makes it difficult to make accurate diagnoses. If there is no entry in the card, it is possible that the woman could have had the disease in an erased form, without pronounced symptoms. There is a small chance that symptoms of another disease may have been mistaken for rubella.
To dispel all doubts, a blood test should be performed for specific antibodies. It is best to do this at the planning stage of pregnancy.
Decoding the results
A positive result for Ig G titers indicates a previous history of rubella. This means that the fetus is 100% guaranteed to be protected from contracting this disease during pregnancy.
Pathogen
The rubella virus is the only member of the Rubivirus genus of the Togavirus family and is not activated when crossing with other members of the group. It has RNA inside, containing all the basic information that is distributed in the cytoplasm.
Initially, rubella is transmitted through contact with a carrier of the infection and enters the body from the upper respiratory organs. The virus replicates locally (in the epithelium, lymph nodes), which leads to viremia and spreads to other tissues. As a result, symptoms of the disease develop and appear after an incubation period of approximately 2 weeks (12 to 23 days) from the initial infection. There is likely an immunological basis for the rash, as it occurs as antibody titers rise.
This virus is relatively unstable and is inactivated using lipid solutions, formalin, low pH, heat, trypsin and amantadine.
Vaccination
Rubella is a controlled infection, the spread of which is regulated by routine vaccination. Specific vaccinations are included in the immunization schedule in many countries. If Ig G is not detected in the blood, rubella vaccination is strictly indicated before a planned pregnancy. Moreover, it should be done no later than the three-month period before conception.
Children are usually vaccinated with the MMR vaccine. Women who do not have Ig G antibodies are administered a specially developed monovaccine, Rudivax.
Pregnancy protection is recommended for the next three months. After their expiration, it is advisable to conduct a control test to confirm the presence of immunity.
Contraindications to vaccination
It is prohibited to vaccinate against rubella under the following conditions:
- malignant processes;
- immunodeficiency states;
- while taking corticosteroids;
- allergy to the drug Neomycin and other vaccinations;
- temperature increase.
How not to get infected
Planning a pregnancy is not only about checking your health and preventing chronic diseases, but also about consulting with a therapist about vaccinations.
Most patients are required to be vaccinated until the age of 18, but some diseases require revaccination, especially if we are talking about a patient over 35 years of age. In this case, revaccination is the prevention of most diseases that negatively affect the fetus and mother. Rubella is a disease that does not require revaccination, but the presence of antibodies in the blood is the key to a safe pregnancy even during an outbreak of the disease. Therefore, vaccination is the only way to prevent complications of fetal development in utero, as well as its death.
If vaccination was not carried out in a timely manner, and pregnancy has already occurred, it is worth remembering that a person who may be a carrier of the infection does not always know about his disease, and therefore the absence of a rash does not mean the absence of the virus in the blood. To protect yourself from possible complications, it is worth taking the following preventive measures:
- limit contact with strangers, especially if there have been cases of rubella outbreak in the area;
- do not visit public places, cinemas, parks and kindergartens with schools;
- if there is a child under 9 years old in the family, be sure to inquire at school or in the kindergarten about outbreaks of the disease, if there is such a fact, do not take the child to the kindergarten or the pregnant woman should temporarily protect herself from contact with the child by moving to relatives in another area;
- carry out quartz treatment of the premises of the house (washing with bleach and other methods of disinfection are ineffective in this case);
- wear a sterile gauze bandage, which should be ironed every 2-3 hours.
Of course, prevention methods are a difficult and complex undertaking that requires effort from a pregnant woman. However, if we are talking about the life of a desired child, then it is worth understanding the likelihood of fetal mortality or injury in utero. However, even if you follow such prevention methods, it is impossible to talk about 100% protection. The best prevention is vaccination.
What to do?
If a pregnant woman who has not previously had rubella and has not been vaccinated finds herself in a hotbed of infection, she should immediately consult an infectious disease specialist. The doctor will write a referral for laboratory testing of rubella virus titers.
Ig M antibodies are specific markers for rubella. They begin to be produced in the blood at the moment of injury. After two to three weeks, their concentration reaches the maximum, and after two months Ig M is eliminated from the body. If Ig M is detected in the blood, then the woman is in the acute phase of the disease. This is the most unfavorable option for pregnant women. To assess the likely risks, it is necessary to find out how long the infection occurred.
If the result is positive before the 17th week, the pregnancy is terminated. Such an exceptional measure is justified even in the absence of symptoms, since in any case the virus will penetrate the placenta and cause dire consequences for the fetus.
At 16-28 weeks, a comprehensive examination is carried out, including ultrasound, genetic analysis, and amniotic fluid sampling. Based on the research results, the question of the presence of fetal anomalies and the need for artificial termination of pregnancy is being considered.
Management of pregnant women with rubella
If the disease is detected after the 28th week, the woman is placed on special medical registration. In this situation, doctors carry out therapeutic measures to maintain the health of the fetus.
Immunoglobulin therapy is indicated. At the same time, measures are being taken to prevent placental insufficiency and prevent miscarriage. Adequate medical care is usually provided in a hospital setting. It helps prevent adverse consequences and avoid miscarriage.
Doctors take into account that rubella during pregnancy can cause complications during childbirth. In particular, there is a risk of abnormal labor. In addition, the born child poses an infectious danger to others for a long period after birth.
Consequences after infection
If infection occurs in the first 2 months of pregnancy, the risk of infection of the fetus is 80%, and the risk of serious pathologies is 25%.
Infection with rubella can kill a child during birth, as well as develop pathologies such as:
- complete deafness;
- heart disease;
- reduced eyeball/brain size;
- critically low weight;
- anemia;
- blindness;
- increased liver size.
Often, if the lesion occurs before 4 months, specialists insist on abortion. If the infection occurs at any other time, the pathology may become a rash on the body, which will disappear completely with age.
Important: if the mother has suffered a severe form of the disease, but the baby is born completely healthy, it is worth considering that the virus remains in his body for two years, so it is extremely necessary to carry out constant monitoring and preventive treatment.