Cardiopulmonary resuscitation (CPR) is a group of surgical and therapeutic measures that are aimed at preserving human life. Carrying out these actions is possible only in the absence of conditions incompatible with life in the patient. Not only medical workers should know the basic cardiopulmonary resuscitation algorithm. Anyone can face the need to provide first aid.
Given the importance of proper emergency care for a person who is experiencing clinical death, every medical student must be accredited in Basic Cardiopulmonary Resuscitation after graduating from medical school.
When you can and cannot do CPR
The need for resuscitation occurs when the following three symptoms are present:
- It is impossible to feel the pulse in the carotid artery.
- The person is unconscious.
- There are no signs of breathing.
Contraindications to CPR are as follows:
- Terminal stages of severe chronic, incurable diseases (cancer patients).
- Presence of injuries incompatible with life.
- The appearance of signs of biological death, which is irreversible (cadaveric spots, rigor of the body).
Basic principles of CPR
For the greatest effectiveness of resuscitation efforts, it is necessary to adhere to the technique of basic cardiopulmonary resuscitation. Maximum efforts should be directed towards:
- Pressing on the chest to ensure blood supply to the internal organs.
- Blowing air into the airways to bring oxygen into the blood.
- Providing access to a vein for injection of medications.
- Administration of drugs after a certain time when previous resuscitation measures are ineffective.
- Carrying out specific measures (defibrillation, tracheal intubation, tracheostomy).
Basic stages of CPR
For about 50 years, the Safar alphabet has been used to provide first aid to people in a state of clinical death. This is an alphabet made up of English letters that shows the algorithm for basic cardiopulmonary resuscitation step by step.
- A - airway - resumption of airway patency for air flow.
- B - breathing - performing artificial respiration.
- C - circulation - ensuring the flow of blood and oxygen to the internal organs due to indirect cardiac massage.
- D - drugs - intravenous administration of medications.
- E - electrocardiograph - diagnosis of changes in heart rhythm.
- F - fibrillation - use of a defibrillator.
- G - gauging - evaluation of results after the above activities.
- H - hypothermia - cooling the patient's head.
- I - intensive care - hospitalization of the patient in the intensive care unit for further treatment and observation.
Steps D through I are performed only by qualified emergency personnel or hospital inpatient physicians. Basic CPR includes the first three steps: opening the airway, insufflating air into the lungs, and compressing the heart. It is these stages that will be discussed in more detail in this article.
Assessing the need for resuscitation
When performing basic cardiopulmonary resuscitation, you first need to assess whether the victim needs it at all. After all, he can just sleep or lie with his eyes closed.
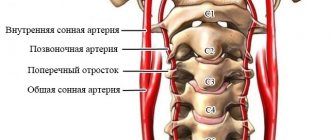
It is necessary to examine the person and assess whether he has any injuries. After all, if there is damage to the cervical vertebrae, it is strictly forbidden to move the patient’s head. Next, you should speak loudly to the victim. If he does not respond and there are no injuries, you need to shake him by the shoulders or hit him on the cheeks. If there is no reaction, it can be confirmed that the victim is unconscious.
The carotid pulse is checked on one side using two fingers located anterior to the sternocleidomastoid muscle. This muscle can be easily felt in the neck if you turn the person’s head in the opposite direction. The muscle immediately tightens and bulges, passing from top to bottom and from back to front. If the pulsation in the carotid artery cannot be felt, it means that the heart is not able to pump blood.
A breathing assessment during basic cardiopulmonary resuscitation is done by placing one hand on the chest and the other on the victim's abdomen. If there is no oscillatory movement of the arms up and down, then he is not breathing. You can also assess breathing by placing your ear to the patient's mouth. By concentrating carefully and breathing, you can feel the warmth of the exhaled air.
The presence of all those signs listed above provides the basis for basic cardiopulmonary resuscitation.
How to determine if resuscitation is being performed correctly
Signs of effectiveness when following the rules for performing artificial respiration are as follows.
When artificial respiration is performed correctly, you may notice the chest moving up and down during passive inspiration.
| How to press | Pressing point | Depth of pressing | Velocity | 2 fingers | 1 finger below the nipple line | 1.5–2 cm | 120 and more | 2/15 |
| 100–120 | ||||||||
| Adult | 2 hands | 2 fingers from the sternum | 5–6 cm | 60–100 | 2/30 |
- If the movement of the chest is weak or delayed, you need to understand the reasons. Probably a loose fit of the mouth to the mouth or nose, a shallow breath, a foreign body preventing the air from reaching the lungs.
- If, when you inhale air, it is not the chest that rises, but the stomach, then this means that the air did not go through the airways, but through the esophagus. In this case, you need to press on the stomach and turn the patient's head to the side, as vomiting is possible.
The effectiveness of cardiac massage also needs to be checked every minute.
- If, when performing an indirect cardiac massage, a push appears on the carotid artery, similar to a pulse, then the pressing force is sufficient for blood to flow to the brain.
- If resuscitation measures are performed correctly, the victim will soon experience heart contractions, blood pressure will rise, spontaneous breathing will appear, the skin will become less pale, and the pupils will narrow.
All actions must be completed for at least 10 minutes, or better yet, before the ambulance arrives. If the heartbeat persists, artificial respiration must be performed for a long time, up to 1.5 hours.
If resuscitation measures are ineffective within 25 minutes, the victim has cadaveric spots, a symptom of a “cat” pupil (when pressure is applied to the eyeball, the pupil becomes vertical, like a cat’s) or the first signs of rigor - all actions can be stopped, since biological death has occurred.
The sooner resuscitation is started, the greater the likelihood of a person returning to life. Their correct implementation will help not only restore life, but also provide oxygen to vital organs, prevent their death and disability of the victim.
Cardiopulmonary resuscitation (CPR) is a set of measures carried out at the stage of emergency care in order to restore the vital functions of the body. It is necessary to start CPR as early as possible, since this will make it possible to bring the person to his senses without incurable consequences.
Clinical death is the main indication for CPR. If two of the three signs of clinical death are determined (lack of breathing, pulse or consciousness), CPR should be started immediately.
According to wikipedia.org.
The technique of performing CPR depends on the competence of the person providing first aid in medical matters. For non-medics, one option for performing resuscitation is recommended, for people knowledgeable in medicine - another, professional one. It also matters whether CPR is given to a newborn, a younger/older child, or an adult.
Airway assessment
This stage corresponds to the letter A - airway. To carry it out, the victim is placed on a flat surface on his back. If the patient has contents in the mouth, it is necessary to clean it with the index and middle fingers wrapped in a napkin or piece of cloth.
Further ensuring airway patency during basic cardiopulmonary resuscitation involves three rules. They are called the Safar technique:
- Maximum tilting of the head back (if there is a suspicion of damage to the cervical vertebrae, this stage is skipped).
- Shift the lower jaw down using two thumbs.
- The lower jaw must be pushed forward with two fingers.
If you follow the above steps step by step, your airways will be clear.
Afterwards, you need to check again for the patient’s respiratory movements. Sometimes breathing is restored after the airways are cleared. If the victim's breathing resumes, he must be turned on his side to prevent fluid from entering the trachea and bronchi.
Turning an unconscious person on his side is not as easy as it seems at first glance. It needs to not only be turned, but fixed in this position to prevent it from being thrown back onto its back. Therefore, the algorithm for conducting basic cardiopulmonary resuscitation describes in stages how to do this correctly:
- Kneel next to the unconscious person.
- One hand of the person being assisted should lie at a right angle, with the back side to the ground.
- The other hand should hug the patient, that is, go through the body, touching the ear on the opposite side with the palm.
- The patient's far leg should be bent at a 90° angle.
- Only now can you turn a person on his side by pulling the leg bent at the knee.
If the victim's breathing has not resumed after clearing the airways, he should continue to lie on his back. Then proceed to the next stage - artificial respiration.
Artificial respiration
Insufflation of air into the lungs during basic cardiopulmonary resuscitation is carried out using the mouth-to-mouth method. The method is considered the most effective. The ambulance has special equipment for artificial respiration - an Ambu bag. This device consists of a mask that covers the patient's mouth and nose, an air filter and a bag that pumps air.
The main disadvantage of mouth-to-mouth breathing is the person’s reluctance to lean against the patient’s face. This is especially unpleasant if the victim has vomited or drooled from the mouth. In any case, this method is recommended to be done through gauze or a cloth, which is placed between the mouth of the victim and the person providing first aid.
With one hand they hold the patient's head in a thrown position, and with the other they squeeze the nose so that air does not escape from the nasal passages. Next, inhale and blow air into the victim’s mouth. The common belief that the more air you inhale, the better, is not true. The entire volume of air does not enter the lungs; most of it still goes into the gastrointestinal tract. And too much air in the stomach leads to vomiting, which can lead to vomit entering the respiratory tract. Therefore, the inhalation should be virtually the same volume as normal.
Air injections must be carried out at a frequency of 12 cycles per minute, which is 1 injection every 5-6 seconds. When artificial respiration is performed effectively, rhythmic movements of the chest are visible.
The reason for the ineffectiveness of artificial respiration may be the presence of obstruction below the level of the oral cavity. For example, with swelling of the larynx or the presence of a foreign body in the trachea. In such cases, the assistance of qualified emergency medical personnel is necessary. They should perform laryngoscopy followed by tracheal intubation. If this is also ineffective, a conicotomy is performed.
You should not immediately stop providing assistance if independent breathing movements appear. Artificial respiration should be continued until the breathing rate increases to 12-15 times per minute.
Description of cardiopulmonary resuscitation
The standard form of cardiopulmonary resuscitation (CPR) consists of 3 stages of emergency care:
- Chest compressions.
- Clearing/opening the airways.
- Artificial pulmonary ventilation (ALV).
The steps presented should be performed in the order listed in accordance with the 2010 American Heart Association (AHA) guidelines.
CPR was founded by Peter Safar, an American physician who developed the triple maneuver used in intensive care.
Health care providers must perform all three components of CPR. Non-medical practitioners can use 30 chest compressions. It is important to perform a head tilt maneuver to open the airway and determine whether the victim is breathing.
Before starting artificial ventilation, airway obstruction must be excluded. To do this, you need to look into the patient’s mouth in order to remove it if there is a foreign body. Otherwise, airway obstruction results in ineffective ventilation/oxygenation and may lead to worsening of the condition.
In the hospital setting or in the presence of a paramedic or other health care provider, as well as in the community setting, Advanced Cardiac Life Support (ACLS) guidelines require a more aggressive approach to the management of cardiac arrest, including interventions with narcotic analgesics, electrocardiographic (ECG) monitoring, defibrillation, and invasive airway procedures.
Trying CPR is better than doing nothing at all, even if you are not sure that the correct actions to take help. This especially applies to the aversion of many people to performing mechanical ventilation using the mouth-to-mouth method. If there is no desire to perform mechanical ventilation at all, performing chest compressions alone is still better than doing nothing.
Indirect cardiac massage
The main stage of the algorithm of actions during basic cardiopulmonary resuscitation is chest compressions. The massage is called indirect because it is performed through the chest tissue. Direct massage on the open heart is possible when it stops during cardiac surgery when the chest is open.
To restore blood circulation, you need to place your hands correctly on your chest. Conventionally divide the sternum into two parts, place your hands between the lower and middle third. A less accurate but simpler method is to place your hands two fingers above the end of the sternum. The hands are placed parallel to the ribs, one on top of the other or in a “lock”.
If a person is unconscious and receives first aid within the first 30 seconds, a pericardial shock may be effective. It is carried out using a sharp blow with a fist on the area of the projection of the heart on the chest. This method can be effective, but only if it is provided to the victim immediately after loss of consciousness.
Basic rules for applying a precordial blow:
- Before striking, you need to make sure that there is no pulse in the carotid artery. It is forbidden to strike even with the slightest pulsation!
- Before striking, remove all clothing from the chest. If this is not possible, you need to make sure there are no buttons or metal objects.
- Cover the xiphoid process with the hand that is not being struck, since it can easily break off if you hit it directly.
- The blow is carried out with a fist above the attachment of the xiphoid process to the sternum. The blow must be sharp and strong enough.
- A precordial beat can only be performed once. Immediately after it, the pulsation in the carotid artery is checked.
- If the pulsation is not detected, proceed to indirect cardiac massage.
The first aid algorithm for basic cardiopulmonary resuscitation states that it is contraindicated to deliver a precordial blow to children under 7 years of age!
The frequency of compressions on the chest is 100 times in 1 minute, carried out to a depth of 2-2.5 cm. In this case, the elbows should be straightened, the main mass is directed towards the hands. When performing indirect massage, you should not take your hands off the patient’s chest.
Compression effectiveness criteria:
- Reduction of pallor and cyanotic skin.
- Constriction of the pupils.
- Palpation of the pulse on the carotid artery.
- The ability to breathe on your own (not always an indicative sign).
Indirect massage is carried out either until the effect appears or until signs of biological death appear. As a rule, if resuscitation measures are ineffective within 30 minutes, they are stopped. The effectiveness of further indirect massage and artificial respiration is practically zero.
Signs of clinical death
It is important to understand what happens to a person after breathing and circulation stop. As cells are no longer supplied with oxygen, they gradually begin to die. You need to understand that this does not happen immediately. While death has not occurred, it remains possible to revive them, provided blood circulation is restored.
The specified period depends on how many minutes the brain cells remain viable. Typically this time is no more than five minutes. In children it is less. Therefore, when performing resuscitation, every second counts.
This state, when a person can still be brought back to life, is called clinical death. Its occurrence can be judged by the following signs:
- After the moment when blood circulation stops, no later than 10 seconds later, loss of consciousness occurs. To check its presence, just contact a person or, for example, stretch your earlobes. You can give a light blow to the cheek with your fingers. Lack of reaction indicates that the patient is unconscious.
- There is no breathing. The technique of its control is based on observation of the movements of the chest. The presence of breathing can be determined by placing your cheek against your mouth to feel the movement of air.
- The functioning of the circulatory system can be checked by feeling the carotid arteries. If there is no pulse in them, it means that the blood circulation is not working.
A person who has these signs needs a resuscitation procedure.
Simultaneous indirect massage and artificial respiration
Most often, these two events are carried out in parallel. Old recommendations say that you should first take two breaths and begin artificial respiration. According to the latest recommendations, if there is only one resuscitator, you only need to do compressions at a frequency of 100 per minute, without wasting time on inhalations. Therefore, the algorithm of actions for basic cardiopulmonary resuscitation ABC is more correctly called ASV.
However, many recommend combining indirect massage with inhalations, even in the presence of only one resuscitator. Then the ratio of the frequency of chest compressions to air inhalations should be 15:2. Therefore, this basic set of cardiopulmonary resuscitation is still controversial.
If there are two resuscitators, then it is necessary to combine compressions with breaths. The frequency in this case is 5:1 (compression:breaths).
Algorithm of resuscitation measures for primary accreditation of specialists
Young doctors must confirm their knowledge at initial accreditation. One of the practical skills tested is basic cardiopulmonary resuscitation. The demonstration of the skill takes place in a separate room, the student demonstrates the principles of providing first aid to a victim on a mannequin. At the same time, he must clearly pronounce all his actions so that the examiner understands what exactly the student is doing.
Below is an algorithm for conducting practical skills in basic cardiopulmonary resuscitation:
- The student enters the room and first examines the place of assistance, turning his head left and right. At the same time, he must say: “I am assessing the danger and inspecting the scene of the incident. There is no danger for me or the patient.”
- Next, it is necessary to check the consciousness of the victim. The student voices that he is testing consciousness, while kneeling on the side of the mannequin. The student takes the mannequin by the shoulders and shakes it gently. You need to make sure his head doesn't hit the floor.
- Calls for help, shouting: “Someone help! The man is unconscious!”
- Determines signs of breathing and circulation. If pulsation in the carotid artery cannot be detected, it clears the airways. One hand is placed on the forehead and tilts the mannequin's head back, and the other picks up the lower jaw using only two fingers.
- The student must determine the ability to breathe independently. To do this, he looks at the mannequin's chest, and then puts his ear to its mouth. At the same time, it further maintains the patency of the airways. The student comments out loud: “I’m checking for breathing.” And counts to 10 out loud.
- The student “calls” an ambulance. He must tell the address, gender and age of the victim. Report that the victim is unconscious and not breathing. The student waits for the response “Challenge accepted.” If it is not there, the next step takes a second.
- The student does not comment on this stage. Kneeling to the side of the mannequin and facing its face, the student unbuttons his shirt to expose his chest. Places one hand with the palm at nipple level. This is the projection of the lower third of the sternum onto the anterior wall of the chest.
- The second palm is placed on the first, the hands are connected like a “lock”. In this case, the fingers do not touch the chest; all efforts fall on the base of the palm.
- The student makes 30 presses, while counting out loud to 30. The arms are not bent at the elbows. It is necessary to ensure that after each press the mannequin’s chest returns to its original position, but the arms cannot be removed. Compressions are carried out to a depth of 5 cm. The frequency is 100 per 1 minute.
- Then the student says: “I’m doing artificial ventilation.” At the same time, he places a mask with a valve over the mannequin’s mouth for his own protection. Use the fingers of one hand to close the nasal passages, the palm of the same hand lies on the victim’s forehead. He holds the lower jaw with the index and middle fingers of his second hand. It takes in air (its standard inhalation volume) and exhales it into the mannequin’s mouth through a special device on the mask.
- Moves his lips away from the mannequin’s mouth for 1 second, and then exhales one more time.
- Repeats the cycle of compressions and artificial ventilation in a ratio of 30:2.
At the end of the basic cardiopulmonary resuscitation accreditation, the first command is: “One minute left.” At the same time, the student continues to provide assistance. When “time is up” sounds, the student leaves the room. This concludes the practical skill demonstration.
6.14. Principles and methods of resuscitationClinical resuscitation (from the Latin re - again, anima - life) is closely related to physiology, pathological anatomy, surgery, therapy and other medical specialties. Its task is to study the mechanisms of those processes that occur in the body during dying, during the development of a terminal state. It has been established that the human body continues to live for some time even after breathing and cardiac activity have stopped, but at the same time the supply of oxygen to the cells, without which the existence of a living organism is impossible, is stopped. Different tissues react differently to the lack of blood and oxygen supply to them, and their death does not occur at the same time. Timely restoration of blood circulation and breathing using a set of measures called resuscitation can bring the patient out of the terminal state. Terminal conditions can be the result of various causes: shock, myocardial infarction, massive blood loss, obstruction of the respiratory tract or asphyxia, electrical trauma, drowning, falling under the ground, etc. In the terminal state, three phases or stages are distinguished: preagonal state; agony; clinical death. In the preagonal state, the patient’s consciousness is still preserved, but it is confused. Blood pressure drops to zero, the pulse increases sharply and becomes thready, breathing is shallow and labored, the skin is pale. During the agony, blood pressure and pulse are not detected, eye reflexes (corneal; reaction of the pupil to light) disappear, breathing takes on the character of swallowing air. Clinical death is a short-term transitional stage between life and death lasting 3-6 minutes. There is no breathing or cardiac activity, the pupils are dilated, the skin is cold, there are no reflexes. During this short period, it is still possible to restore vital functions with the help of resuscitation. At a later date, irreversible changes occur in the tissues, and clinical death turns into biological, true death. Clinical death differs from biological death in the absence of cadaveric spots and rigor. In a terminal condition - regardless of its cause - general changes occur in the body, without understanding which it is impossible to understand the essence and meaning of resuscitation methods. These changes affect all organs and systems of the body (brain, heart, metabolism, etc.) and occur in some organs earlier, in others later. Considering that organs continue to live for some time even after respiratory and cardiac arrest, with timely resuscitation it is possible to revive the patient. The cerebral cortex is the most sensitive to hypoxia (low oxygen content in the blood and tissues), therefore, in terminal conditions, the functions of the higher part of the central nervous system - the cerebral cortex - are switched off first: the person loses consciousness. If the duration of oxygen starvation exceeds 3-4 minutes, then restoration of the activity of this part of the central nervous system becomes impossible. Following the shutdown of the cortex, changes also occur in the subcortical regions of the brain. The last to die is the medulla oblongata, which contains the automatic centers of respiration and blood circulation. Irreversible brain death occurs. Increasing hypoxia and impaired brain function in a terminal state lead to disruption of the cardiovascular system. In the preagonal period, the pumping function of the heart drops sharply and the amount of blood it ejects decreases - the so-called cardiac output. A decrease in blood supply to organs and especially the brain accelerates the development of irreversible changes. Due to the presence of the heart's own automatism system, its contractions can continue for quite a long time. However, these contractions are ineffective: the filling of the pulse decreases, it becomes thread-like; blood pressure drops sharply and then becomes undetectable. Subsequently, the rhythm of heart contractions is significantly disrupted, and cardiac activity stops. In the initial phase of the terminal state—predagonia—breathing becomes faster and deeper. During the period of agony, along with a drop in blood pressure, breathing becomes uneven, shallow and, finally, stops completely - a terminal pause occurs. In the terminal state, sharp changes in metabolism are observed in the body. They are expressed, first of all, in a decrease in oxidative processes, which leads to the accumulation of organic acids (lactic and pyruvic) and carbon dioxide in the body. As a result, the acid-base balance of the body is disrupted. Normally, the reaction of blood and body tissues is neutral. The attenuation of oxidative processes during the terminal state shifts the reaction to the acidic side - acidosis occurs. After the body emerges from the state of clinical death, the activity of the heart is first restored, then spontaneous breathing, and only later, when the sharp changes in metabolism and acid-base state disappear, can brain function be restored. The period of restoration of the function of the cerebral cortex is the longest. Even after short-term hypoxia and clinical death (less than a minute), consciousness may be absent for a long time. The main tasks of resuscitation of a patient in a state of clinical death are the fight against hypoxia and stimulation of fading body functions. According to the degree of urgency, resuscitation measures can be divided into two groups: maintaining artificial respiration and artificial circulation and intensive therapy aimed at restoring independent circulation and breathing, normalizing the functions of the central nervous system, liver, kidneys, and metabolism. Resuscitation in case of respiratory arrest. The need for artificial respiration, or, more correctly, artificial ventilation of the lungs, occurs with asphyxia due to obstruction.
Rice. 85. Freeing the oral cavity and pharynx from foreign bodies, mucus and vomit: a - manually; b - using a suction bulb
flogging of the respiratory tract by foreign bodies, drowning, electric shock, poisoning with various toxic substances or medications, cerebral hemorrhage, traumatic shock. Artificial respiration is the only method of treating all conditions when the patient’s spontaneous breathing cannot provide sufficient oxygen saturation of the blood. Acute respiratory failure can also occur secondarily - due to circulatory disorders, for example, during cardiac arrest. Acute respiratory failure and its extreme degree - respiratory arrest - regardless of the cause, lead to a decrease in oxygen content in the body (hypoxia) and excessive accumulation of carbon dioxide in the blood and tissues (hypercapnia). As a result of hypoxia and hypercapnia, severe dysfunctions of all organs develop in the body, which can only be eliminated with timely resuscitation - mechanical ventilation. There are various methods of mechanical ventilation. Artificial respiration by insufflation of air can be carried out in several ways. The simplest of them is mechanical ventilation using the “mouth to mouth” or “mouth to nose” method. There are hand-held artificial respiration devices in the form of an elastic rubber bag with a mask. The technique of artificial lung ventilation is “mouth-to-court” or “mouth-to-nose”. To carry out artificial respiration, it is necessary to lay the patient on his back, unfasten the clothes that are constricting the chest and ensure free passage of the airways. If there is content in the mouth or throat, it must be quickly removed with a finger, a napkin, a handkerchief, or using any suction (Fig. 85). To clear the airway, the victim's head should be pulled back. It must be remembered that excessive abduction of the head can lead to narrowing of the airways. To more fully open the airways, it is necessary to move the lower jaw forward. To prevent the tongue from retracting during artificial respiration, you should hold your head in an abducted position with your hand, moving the lower jaw forward.
Rice. 86. Artificial ventilation of the lungs using the “mouth to mouth” method: a — position of the victim’s head; b - blowing air through the mouth
When performing mouth-court breathing, the victim’s head is held in a certain position (Fig. 86). The resuscitator, taking a deep breath and pressing his mouth tightly to the patient’s mouth, blows air into his lungs. In this case, you need to hold your nose with your hand near the victim’s forehead. Exhalation is carried out passively, due to the elastic forces of the chest. The number of breaths per minute should be at least 16-20. Insufflation must be carried out
Rice. 87. Schematic representation of the installed air duct Fig. 88. Artificial ventilation through an air duct
Rice. 89. Artificial ventilation of the lungs using the “mouth to nose” method: a — position of the victim’s head; b - blowing air through the nose
quickly and sharply (in children - less sharply), so that the duration of inhalation is 2 times less than the exhalation time. It is necessary to ensure that the exhaled air does not lead to excessive distension of the stomach. In this case, there is a danger of food masses being released from the stomach and entering the bronchi. Of course, mouth-to-mouth breathing creates significant hygienic inconveniences. You can avoid direct contact with the patient’s mouth by blowing air through a gauze pad, handkerchief or any other loose material. With this method of ventilation, air ducts can be used (Fig. 87,88). When using the mouth-to-nose breathing method, air is blown through the nose. In this case, the victim’s mouth should be closed with a hand, which at the same time moves the jaw upward to prevent the tongue from retracting (Fig. 89). Artificial ventilation of the lungs using manual respirators. First, the airway must be secured as described previously and an airway must be inserted. A mask is placed tightly over the patient's nose and mouth. Squeezing the bag, inhale (Fig. 90). Exhalation is carried out through the valve of the bag, and its duration is 2 times longer than the duration of inhalation. With all methods of mechanical ventilation, it is necessary to evaluate its effectiveness by chest excursion. Under no circumstances should artificial respiration be started without clearing the victim’s airways of foreign bodies or food masses! Long-term ventilation of the lungs using the listed methods is impossible; it serves only to provide first aid and assistance during transportation. Therefore, without stopping resuscitation - cardiac massage and artificial respiration, you should call an ambulance or transport the patient to a medical facility to provide qualified assistance.
Rice. 90. Carrying out artificial ventilation of the lungs using a hand-held respirator bag
Resuscitation in case of circulatory arrest. The cessation of heart activity can occur under the influence of a variety of reasons (drowning, suffocation, gas poisoning, electric shock and lightning, cerebral hemorrhage, myocardial infarction and other heart diseases, heat stroke, blood loss, direct blow to the heart, burns, freezing etc.) and in any environment - in a hospital, dental office, at home, on the street, at work. In any of these cases, the resuscitator has only 3-4 minutes to make a diagnosis and restore blood supply to the brain. There are two types of cardiac arrest: asystole (true cardiac arrest) and ventricular fibrillation (fluttering), when the heart muscles contract chaotically and uncoordinated. In both the first and second cases, the heart stops “pumping” blood and the blood flow in the vessels stops. The main symptoms of cardiac arrest, which allow a quick diagnosis, are: - loss of consciousness; - absence of pulse in the carotid and femoral arteries; - absence of heart sounds; - respiratory arrest; - pallor or cyanosis of the skin and mucous membranes; - dilated pupils that do not contract when exposed to light; - convulsions, which may appear at the moment of loss of consciousness and be the first noticeable surrounding symptom of cardiac arrest. These symptoms convincingly indicate circulatory arrest and that not a second should be wasted on additional examination (measuring blood pressure, determining the pulse rate) or searching for a doctor, but it is necessary to immediately begin resuscitation - cardiac massage and artificial respiration. It should be remembered that cardiac massage should always be carried out simultaneously with artificial respiration, as a result of which the circulating blood is supplied with oxygen. Otherwise, resuscitation is pointless. Currently, two types of heart massage are used - open (or direct), which is used only during operations on the organs of the chest cavity, and closed (external), carried out through the unopened chest. Cardiopulmonary resuscitation (CPR) is a set of basic and specialized (medicinal, etc.) measures to revive the body. Survival depends on two main factors: - early recognition of circulatory arrest; — immediate start of main activities. The sequence of performing basic CPR measures: 1. Assess the scene of the incident from the point of view of safety for the person providing assistance. 2. State the absence of reactions to external stimuli (lack of consciousness). 3. Make sure there is no external respiration and no pulse in the carotid artery. 4. Correctly place the person being resuscitated on a hard, flat surface below the lumbar level of the person who will perform resuscitation. 5. Ensure patency of the upper respiratory tract. 6. In case of sudden cardiac arrest (electrical trauma, drowning, etc.), apply a precordial blow. 7. Check for spontaneous breathing and pulse. 8. Call assistants and the resuscitation team. 9. If there is no spontaneous breathing, start mechanical ventilation - perform two full mouth-to-mouth exhalations. 10. Check for the presence of a pulse in the carotid artery (place two fingers on the carotid artery). 11. Start chest compressions in combination with mechanical ventilation and continue until the resuscitation team arrives. Resuscitation measures can be stopped only upon the arrival of a resuscitation team or when reliable signs of biological death appear. Exceptions when it makes sense to continue CPR: - resuscitation of a child; - hypothermia (when death cannot be confirmed until active rewarming is carried out); - drowning (especially in cold water); - repeated cardiac arrest after restoration of cardiac activity. External cardiac massage technique. The meaning of external massage is the rhythmic compression of the heart between the sternum and the spine. In this case, blood is expelled from the left ventricle into the aorta and enters, in particular, into the brain, and from the right ventricle into the lungs, where it is saturated with oxygen. After the pressure on the sternum stops, the cavities of the heart are filled with blood again (Fig. 91). To perform external cardiac massage, the patient is placed on a solid base (floor, ground). Massage cannot be performed on a mattress or soft surface. Reanimator
Rice. 91. The mechanism of external cardiac massage: a - artificial systole (heart contraction); b - diastole (relaxation of the heart and filling of the ventricles with blood)
stands on the side of the patient and, with his palms placed one on top of the other, presses on the sternum with such force as to bend it towards the spine by 4-5 cm. The frequency of pressing is 50-70 per minute. The hands should rest on the lower third of the sternum, two fingers above the xiphoid process (Fig. 92). In children, cardiac massage should be performed with only one hand, and in infants - with the tips of two fingers at a frequency of 100-120 pressures per minute. The point of application of the fingers in children under 1 year of age is at the lower end of the sternum. When giving a massage to adults, it is necessary not only to use arm strength, but also to apply pressure with the whole body. This type of massage requires significant physical exertion and is very tiring. If resuscitation is carried out by one person, then after every 15 compressions of the sternum with an interval of one second, he must, stopping the massage, take two strong breaths using the “mouth to mouth”, “mouth to nose” methods or with a special hand-held respirator. If two people are involved in resuscitation, one lung inflation should be performed after every five sternal compressions (Fig. 93). The effectiveness of cardiac massage is assessed by the following criteria: 1) the appearance of a pulse in the carotid, femoral and radial arteries; 2) increase in blood pressure to 60-80 mm Hg. Art.; 3) constriction of the pupils and the appearance of their reaction to light; 4) disappearance of the bluish color and “dead” pallor; 5) subsequent restoration of spontaneous breathing. It should be remembered that rough external cardiac massage can lead to serious complications - rib fractures with damage to the lungs and heart. With strong pressure on the xiphoid process of the sternum, rupture of the stomach and liver can occur. Particular care should be taken when performing massage on children and the elderly. If, after 30-40 minutes from the start of cardiac massage, artificial respiration and drug therapy, cardiac activity is not restored, the pupils remain
Rice. 92. Technique of external cardiac massage: a - location of hands when performing cardiac massage; b, c - correct placement of hands during massage
Rice. 93. Simultaneous artificial respiration and external cardiac massage
If there is no reaction to light, we can assume that irreversible changes and brain death have occurred in the body, and it is advisable to stop resuscitation. If clear signs of death appear, resuscitation may be stopped earlier. In some severe illnesses and traumatic injuries (malignant tumors with metastases, severe skull trauma with crushing of the brain), resuscitation will not make sense and should not be started. In other cases of sudden death, there is always hope for reviving the patient, and for this all possible measures must be taken. Transportation of a patient with respiratory and cardiac arrest can be carried out only after restoration of cardiac activity and breathing or in a specialized ambulance, in which resuscitation measures can be continued. It should be remembered that resuscitation must be carried out immediately after the cessation of breathing and cardiac activity. Resuscitation at a later date (later than 5 minutes) can restore breathing and cardiac activity, but normal brain activity will not resume. Basic resuscitation measures in children. In newborns and infants, the most common causes of circulatory arrest are sudden neonatal death syndrome, pulmonary diseases (pneumonia, acute bronchospasm), airway obstruction, drowning, sepsis, and neurological diseases. In children of the first years of life (over 1 year), the main cause of circulatory arrest is injuries, most often as a result of car accidents (especially if seat belts are not used), pedestrian injuries (when a child runs out onto the roadway), bicycle injuries (especially head injuries) , drowning, burns and gunshot wounds. In children, basic resuscitation measures are carried out approximately according to the same scheme as in adults, but there are some peculiarities: If the resuscitator acts alone, he carries out basic resuscitation measures until the arrival of the resuscitation team. — When performing mechanical ventilation in children up to 1 month of age. The resuscitator covers the child’s mouth and nose with his mouth at the same time. In children over 6 months. breathing is done “mouth to mouth”, and the child’s nose is pinched with the thumb and forefinger. — Airway patency is ensured by lifting the chin or pushing the child’s lower jaw forward. Air is inhaled slowly (for 1-1.5 seconds), during pauses the resuscitator breathes deeply in order to maximize the oxygen content and reduce the concentration of carbon dioxide in the exhaled air. — In the absence of spontaneous breathing in a child in the first years of life, the most important resuscitation measure is mechanical ventilation. Caution is required regarding the pressure and volume of each airway (this varies significantly depending on the child's age and airway resistance). The volume of each insufflation is considered adequate if it causes a quiet rise of the chest. The rate of mechanical ventilation for children in the first years of life is 20 respiratory movements per minute. Detection of airway obstruction. If the chest does not rise during ventilation, this indicates the need for more tidal volume (or higher pressure) or airway obstruction. Since the most common cause of obstruction is incomplete opening of the airway, the patient's head should be carefully repositioned (unless there is reason to suspect a cervical spine injury) and then mechanical ventilation should be attempted again. Assessment of blood circulation. It is recommended to check the pulse in children under one year of age on the brachial artery, and in children over one year of age - on the carotid artery. Indirect cardiac massage. For infants, apply pressure with the middle and ring fingers on the lower third of the sternum (approximately the thickness of one finger below the level of the nipples); The resuscitator uses the other hand to support the child's head in a position that ensures airway patency. The depth of compression of the sternum is from 1.5 to 2.5 cm, the frequency of compression is 100 times per minute. For children aged 1-8 years, apply pressure to the lower third of the sternum (approximately a finger's width above the xiphoid process) with the proximal part of the palm. The depth of compression of the sternum is from 2.5 to 4 cm, the frequency of compression is 90-80 times per minute. The ratio of compression frequency to mechanical ventilation rate for children in the first years of life is maintained at 5:1, regardless of how many people are involved in resuscitation. The child’s condition is re-evaluated 1 minute after the start of resuscitation, and then every 2-3 minutes.
Monitoring the success of resuscitation
When carrying out basic cardiopulmonary resuscitation measures, its effectiveness must be checked. After making 4 cycles of compressions and air injections, you need to palpate the pulse on the carotid artery for 3-5 seconds. When a pulse appears, compressions are stopped and the patient's ability to breathe independently is checked. If breathing has also resumed, it is necessary to maintain patency of the airway and carefully monitor the patient’s condition until the ambulance arrives.
To maximize the effectiveness of basic cardiopulmonary resuscitation, it is started immediately. Irreversible changes in brain tissue begin within 5-6 minutes after the heartbeat stops. Before resuscitation begins, an ambulance must be called. They provide assistance before her arrival.
Work order
Artificial respiration using the mouth-to-mouth method.
1. On the chest of a mannequin lying on its back, unbutton the clothes and determine the need for breathing through the stationary state of the chest.
2. Examine the oral cavity in order to identify and remove foreign objects that interfere with breathing.
3. Tilt the mannequin's head back as far as possible by placing one hand under the neck and pressing the other on the forehead (this ensures airway patency).
4. Turn the mannequin’s head to one side and, if necessary, remove foreign objects.