Almost every pregnant woman has heard something about screening in the first trimester of pregnancy (prenatal screening). But often even those who have already completed it do not know what exactly it is prescribed for.
And for expectant mothers who are yet to do this, this phrase sometimes seems frightening. And it scares only because the woman does not know how this is done, how to interpret the results obtained later, and why the doctor needs this. You will find answers to these and many other questions related to this topic in this article.
So, more than once I had to deal with the fact that a woman, having heard the incomprehensible and unfamiliar word screening, began to draw terrible pictures in her head that frightened her, making her want to refuse to undergo this procedure. Therefore, the first thing we will tell you is what the word “screening” means.
Screening (English screening - sorting) are various research methods, which, due to their simplicity, safety and accessibility, can be used en masse in large groups of people to identify a number of signs. Prenatal means prenatal. Thus, we can give the following definition to the concept of “prenatal screening”.
Screening in the first trimester of pregnancy is a set of diagnostic tests used in pregnant women at a certain stage of pregnancy to identify gross malformations of the fetus, as well as the presence or absence of indirect signs of pathologies of fetal development or genetic abnormalities.
The acceptable period for screening in the 1st trimester is 11 weeks - 13 weeks and 6 days (see the calculator for calculating the gestational age by week). Screening is not carried out earlier or later, since in this case the results obtained will not be informative and reliable. The most optimal period is considered to be 11-13 obstetric weeks of pregnancy.
Who is referred for first trimester screening?
According to Order No. 457 of the Ministry of Health of the Russian Federation of 2000, prenatal screening is recommended for all women. A woman can refuse it, no one will force her to do this research, but doing this is extremely reckless and only speaks of the woman’s illiteracy and negligent attitude towards herself and, above all, towards her child.
Risk groups for whom prenatal screening should be mandatory:
- Women whose age is 35 years or more.
- The presence of a threat of termination of pregnancy in the early stages.
- History of spontaneous miscarriage(s).
- History of missed or regressed pregnancy(ies).
- Presence of occupational hazards.
- Previously diagnosed chromosomal abnormalities and (or) malformations in the fetus based on screening results in past pregnancies, or the presence of children born with such anomalies.
- Women who have had an infectious disease in early pregnancy.
- Women who took medications prohibited for pregnant women in the early stages of pregnancy.
- Presence of alcoholism, drug addiction.
- Hereditary diseases in the woman’s family or in the child’s father’s family.
- Close relationship between the mother and father of the child.
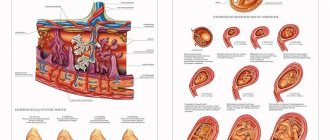
Prenatal screening at 11-13 weeks of pregnancy consists of two research methods - ultrasound screening of the 1st trimester and biochemical screening.
When is the test performed?
An analysis to detect chromosomal pathologies is carried out at the end of the third trimester.
From 11 to 13 weeks of gestation, a pregnant woman must donate blood for three types of hormones and undergo an ultrasound examination.
The combination of two tests allows you to expand the picture of the pathology and take appropriate measures.
It is important to note that the first trimester is a “natural” selection for the fetus, therefore, if severe fetal malformations are detected, termination of pregnancy is proposed.
Questionable results are confirmed by non-invasive diagnostic methods, which confirm or refute the diagnosis with 98% accuracy.
Pregnant women make their own decisions, after consulting with a geneticist and comparing the risks of pathology.
Children with Down syndrome require specialized care and treatment. Sometimes the underlying pathology is combined with defects of the heart muscle, respiratory and nervous systems.
Ultrasound examination as part of screening
Preparation for the study: If the ultrasound is performed transvaginally (the sensor is inserted into the vagina), then no special preparation is required. If the ultrasound is performed transabdominally (the sensor is in contact with the anterior abdominal wall), then the study is carried out with a full bladder. To do this, it is recommended not to urinate 3-4 hours before the test, or drink 500-600 ml of still water an hour and a half before the test.
Necessary conditions for obtaining reliable ultrasound data. According to the norms, screening of the first trimester in the form of ultrasound is carried out:
- No earlier than 11 obstetric weeks and no later than 13 weeks and 6 days.
- The CTP (coccygeal-parietal size) of the fetus is not less than 45 mm.
- The position of the child should allow the doctor to adequately take all measurements; otherwise, it is necessary to cough, move, walk for a while so that the fetus changes its position.
As a result of ultrasound, the following indicators are examined:
- KTR (coccygeal-parietal size) – measured from the parietal bone to the coccyx
- Head circumference
- BDP (biparietal size) - the distance between the parietal tuberosities
- Distance from frontal bone to occipital bone
- Symmetry of the cerebral hemispheres and its structure
- TVP (collar thickness)
- Fetal heart rate (heart rate)
- Length of humerus, femur, forearm and shin bones
- Location of the heart and stomach in the fetus
- Sizes of the heart and great vessels
- Placenta location and thickness
- Water quantity
- Number of vessels in the umbilical cord
- Condition of the internal os of the cervix
- Presence or absence of uterine hypertonicity
Decoding of the received data:
| KTE, mm | TVP, mm | Nasal bone, mm | Heart rate, beats per minute | BPR, mm | |
| 10 weeks | 33-41 | 1,5-2,2 | Visible, size not estimated | 161-179 | 14 |
| 11 weeks | 42-50 | 1,6-2,4 | Visible, size not estimated | 153-177 | 17 |
| 12 weeks | 51-59 | 1,6-2,5 | More than 3 mm | 150-174 | 20 |
| 13 weeks | 62-73 | 1,7-2,7 | More than 3 mm | 147-171 | 26 |
How is screening performed in the 1st trimester?
The best option for screening is to conduct both tests on the same day. This makes preparation easier and reduces the likelihood of erroneous results. Unlike a regular ultrasound at 12 weeks, screening is carried out by sonologists using supersensitive equipment for prenatal examination, most often transvaginal . A day after it, light spots of blood may be observed in the discharge, but do not be alarmed. It’s just that the mucous membrane is unusually sensitive to such interventions.
Carrying out transvaginal ultrasound:
- The woman is asked to undress from the waist down and lie on the couch with her legs bent.
- The sonologist places a condom on a thin sensor and inserts the device into the vagina.
- To get a more complete picture, the sensor is moved in different directions, but the pregnant woman does not feel pain.
Performing an abdominal ultrasound:
- The doctor invites a pregnant woman to lie down on the couch and expose her belly.
- A special lubricant is applied to the surface of the abdomen to improve signal transmission from the sensor to the computer monitor.
- The scanner glides easily over the abdomen without causing discomfort.
The entire screening ultrasound process takes from 20 to 30 minutes . If it is difficult to determine the size, the mother may be asked to move or cough so that the embryo changes position.
Blood from a vein is taken under sterile conditions, and the main discomfort is felt when puncturing to find a suitable vein
In the office where blood is taken from a vein for analysis, the expectant mother will be required to answer several questions to be entered into a questionnaire. This is necessary for subsequent decoding of the results. The blood sampling procedure itself is as follows:
- The expectant mother is seated on a chair or asked to lie down on the couch and asked to free her hand in the elbow area.
- The hand should have a solid support such as a table surface, the veins should be tensed as if by pumping movements of the hand.
- The laboratory assistant disinfects the future puncture site with an alcohol solution and begins collecting the required amount of blood (10 ml).
- Having taken the needle out of the vein, a piece of cotton wool is placed on the puncture site, which must be clamped, and after 5-7 minutes thrown into a specially designated container.
Although I became pregnant at 26 years old, I donated blood from a vein for the first time in the maternity hospital, when I was 23 years old. Therefore, I would not rule out the possibility that expectant mothers may be afraid of an unfamiliar procedure. I remember I walked proudly into the office, sat down on a chair and extended my ring finger to the doctor. Previously, I donated blood for the Wasserman reaction (RW) during a medical examination at the dermatovenerology clinic, where it was taken from a finger. Even there I squinted at the sight of the scarifier, and then the female laboratory assistant said to me, “Well, what is your finger for? Roll up your sleeve and work with your fist.” It turned out that before taking a biopsy in our maternity hospital it is necessary to donate blood for RW from a vein. Apparently, my face changed so much that after announcing a possible fainting, the nurse told me to lie down on the couch and turn to the wall. My veins are good, my auntie is a professional, and after 5 minutes they told me that “That’s it, artist, you can go, the doctor will have the results.” So, girls, don't be afraid, everything will be fine.
Detailed screening results will be ready in a few weeks. Usually they are delivered immediately to the office of the gynecologist leading the pregnancy, but it is advisable to clarify.
Video: what the doctor sees during an ultrasound during the first screening
Features of screening for multiple pregnancies
To date, there is no reliable information about what level of hCG can be considered normal when carrying twins, so a biochemical blood test is not included in screening for multiple pregnancies.
What pathologies can be detected by ultrasound?
Based on the results of ultrasound screening in the 1st trimester, we can talk about the absence or presence of the following anomalies:
- Down syndrome is trisomy 21, the most common genetic disorder. Detection prevalence 1:700 cases. Thanks to prenatal screening, the birth rate of children with Down syndrome has decreased to 1:1100 cases.
- Pathologies of neural tube development (meningocele, meningomyelocele, encephalocele and others).
- Omphalocele is a pathology in which part of the internal organs is located under the skin of the anterior abdominal wall in the hernial sac.
- Patau syndrome is trisomy on chromosome 13. The incidence is on average 1:10,000 cases. 95% of children born with this syndrome die within a few months due to severe damage to internal organs. Ultrasound shows increased fetal heart rate, impaired brain development, omphalocele, and delayed development of tubular bones.
- Edwards syndrome is trisomy on chromosome 18. The incidence rate is 1:7000 cases. It is more common in children whose mothers are over 35 years old. An ultrasound shows a decrease in the fetal heartbeat, an omphalocele, the nasal bones are not visible, and one umbilical artery instead of two.
- Triploidy is a genetic abnormality in which there is a triple set of chromosomes instead of a double set. Accompanied by multiple developmental defects in the fetus.
- Cornelia de Lange syndrome is a genetic anomaly in which the fetus experiences various developmental defects, and in the future, mental retardation. The incidence rate is 1:10,000 cases.
- Smith-Opitz syndrome is an autosomal recessive genetic disease manifested by metabolic disorders. As a result, the child experiences multiple pathologies, mental retardation, autism and other symptoms. The average incidence is 1:30,000 cases.
Down syndrome: causes during pregnancy
The causes of Down syndrome during pregnancy lie in the occurrence of chromosome pathologies. This pathology can develop even in completely healthy parents. The cause of Down syndrome during pregnancy is the formation of an additional copy of the genetic material of the 21st chromosome, or all chromosomes, or some parts of the chromosome. The causes of Down syndrome during pregnancy have nothing to do with the environment, the lifestyle of the parents, taking medications and other negative phenomena. Down syndrome in pregnancy is the result of a random chromosomal abnormality that cannot be prevented or changed in the future. Therefore, if Down syndrome develops during pregnancy, you should not look for someone to blame or blame loved ones for the appearance of this chromosomal abnormality.
However, according to many studies, there are a number of factors that increase the risk of developing Down syndrome during pregnancy:
- woman's age over 35 years;
- the man's age is over 42 years;
- consanguineous marriages;
- bad habits that can affect the quality of genetic material (smoking, drugs, alcohol).
Learn more about diagnosing Down syndrome
Mainly, an ultrasound examination at 11-13 weeks of pregnancy is performed to identify Down syndrome. The main indicator for diagnosis becomes:
- Neck space thickness (TNT). TVP is the distance between the soft tissues of the neck and the skin. An increase in the thickness of the nuchal translucency may indicate not only an increased risk of having a child with Down syndrome, but also that other genetic pathologies in the fetus are possible.
- In children with Down syndrome, most often the nasal bone is not visualized at 11-14 weeks. The contours of the face are smoothed.
Before 11 weeks of pregnancy, the thickness of the nuchal translucency is so small that it is impossible to adequately and reliably assess it. After the 14th week, the fetus develops a lymphatic system and this space can normally be filled with lymph, so the measurement is also not reliable. The incidence of chromosomal abnormalities in the fetus depending on the thickness of the nuchal translucency.
| TVP, mm | Frequency of anomalies, % | Increased TVP | Normal TVP |
| 3 | 7 | ||
| 4 | 27 | ||
| 5 | 53 | ||
| 6 | 49 | ||
| 7 | 83 | ||
| 8 | 70 | ||
| 9 | 78 |
When deciphering the screening data of the 1st trimester, it should be remembered that the thickness of the nuchal translucency alone is not a guide to action and does not indicate a 100% probability of the presence of the disease in the child.
Therefore, the next stage of screening of the 1st trimester is carried out - taking blood to determine the level of β-hCG and PAPP-A. Based on the obtained indicators, the risk of having a chromosomal pathology is calculated. If the risk based on the results of these studies is high, then amniocentesis is suggested. This is taking amniotic fluid for a more accurate diagnosis.
In particularly difficult cases, cordocentesis may be required - taking cord blood for analysis. Chorionic villus sampling may also be used. All of these methods are invasive and carry risks for the mother and fetus. Therefore, the decision to perform them is decided by the woman and her doctor jointly, taking into account all the risks of carrying out and refusing the procedure.
In what cases is genetic consultation necessary?
Genetic consultation and prenatal diagnosis are recommended in cases where parents have chromosomal abnormalities or congenital diseases and/or if structural/chromosomal abnormalities of the fetus are detected.
What is a risk group?
A patient is at risk if the likelihood of pathologies associated with pregnancy/fetus/childbirth is greater than others. This does not mean that a patient at risk will certainly develop pathology, but still, during pregnancy monitoring, special attention must be paid to the timely diagnosis of pathologies and the prevention of complications during pregnancy.
At the same time, a patient who is not included in the risk group can also develop any pathology of pregnancy/fetus/childbirth, but the risk of this is much lower.
First trimester screening includes measuring nuchal translucency thickness and determining biochemical markers.
Biochemical screening of the first trimester of pregnancy
This stage of the study must be carried out after an ultrasound scan. This is an important condition, because all biochemical indicators depend on the duration of pregnancy, down to the day. Every day the norms of indicators change. And ultrasound allows you to determine the gestational age with the accuracy that is necessary for conducting a correct study. At the time of donating blood, you should already have ultrasound results with the indicated gestational age based on CTE. Also, an ultrasound may reveal a frozen pregnancy or a regressing pregnancy, in which case further examination does not make sense.
Preparing for the study
Blood is drawn on an empty stomach! It is not advisable to even drink water in the morning of this day. If the test is carried out too late, you are allowed to drink some water. It is better to take food with you and have a snack immediately after blood sampling rather than violate this condition.
2 days before the scheduled day of the study, you should exclude from your diet all foods that are strong allergens, even if you have never been allergic to them - these are chocolate, nuts, seafood, as well as very fatty foods and smoked foods.
Otherwise, the risk of obtaining unreliable results increases significantly.
Let's consider what deviations from normal levels of β-hCG and PAPP-A may indicate.
How to prepare for 1st trimester screening
Between the ultrasound and blood sampling from a vein for biochemistry, as little time as possible should pass so that the results correspond in time, this is a maximum of 2-3 days. Advice on preparation based on the experience of other women and the requirements for the procedure would be useful:
- Find out in advance whether both tests can be done at the same diagnostic center. When choosing a medical institution, rely on reviews of the staff. Whether the service was provided for money or free of charge - this does not in any way affect the readings of instruments and reagents;
- Check out the appointment schedule, or better yet, make an appointment for a specific time so as not to wait for a long time in front of the office. Please note that blood for any tests is submitted to the laboratory in the early morning hours, and not whenever you want. You can donate blood in the morning, and in the afternoon get an appointment with an ultrasound specialist or undergo an ultrasound examination the day before visiting the laboratory;
- Follow a diet for a day before screening. Eliminate from the menu foods that can cause allergies - nuts, citrus fruits, brightly colored fruits, seafood, chocolate and smoked, fried or fatty foods. Stop taking multivitamin complexes 3 days before the examination so that the result is undistorted;
- do not forget to weigh yourself at home before going to the medical facility. The laboratory technician will enter this indicator into the questionnaire during the examination;
- on the eve of the screening test, refrain from sexual intercourse, and do not eat anything for at least 4 hours before visiting the doctor’s office;
- take care of comfortable clothes. To donate blood you will need to roll up your sleeve, for an abdominal ultrasound you will need to expose your stomach, and for examination through the vagina you will need to undress below the waist;
- Preparation for transvaginal ultrasound consists of purchasing a special gynecological condom to put on the sensor. Half an hour before the abdominal examination, drink 2-3 glasses of clean water without carbon so that the bladder is full and do not visit the restroom until the end of the examination.
For convenience, during an ultrasound examination through the abdomen, it is better to wear clothes that do not have to be completely removed
β-hCG – human chorionic gonadotropin
This hormone is produced by the chorion (“shell” of the fetus), thanks to this hormone it is possible to determine the presence of pregnancy in the early stages. The level of β-hCG gradually increases in the first months of pregnancy, its maximum level is observed at 11-12 weeks of pregnancy. Then the level of β-hCG gradually decreases, remaining unchanged throughout the second half of pregnancy.
| Normal levels of human chorionic gonadotropin, depending on the stage of pregnancy: | An increase in β-hCG levels is observed in the following cases: | A decrease in β-hCG levels is observed in the following cases: | |
| weeks | β-hCG, ng/ml |
|
|
| 10 | 25,80-181,60 | ||
| 11 | 17,4-130,3 | ||
| 12 | 13,4-128,5 | ||
| 13 | 14,2-114,8 | ||
First screening: preparation for it and results
In order for all results to be accurate, it is important to follow a specific diet. Before the first study, a day, or better yet three days at 11-13 weeks, you must completely eliminate seafood, chocolate, fried foods, and citrus fruits.
If you have your first abdominal ultrasound, you should drink half a liter of liquid an hour before the procedure.
First trimester screening can have varying results depending on many factors. For example, if IVF was done, the hCG level will be slightly higher, but PAPP-A, on the contrary, will be lower.
If the expectant mother is overweight, the content of all substances in the blood will be increased. If the body weight is small, then, on the contrary, it is reduced. If a pregnant woman suffers from diabetes, the hormone levels will be reduced, but the accuracy of the results will be extremely low.
The results of the first screening are quite accurate. The period of pregnancy, starting from the 10th week, is considered the most favorable to identify pathologies, however, blood tests and ultrasound should be checked by a competent specialist. It often happens that women are diagnosed with serious pathologies and are predicted to have a high mortality rate after birth. As a result, they are advised to have an induced birth. But after them, pathologies are discovered in the fetus, with which he could easily live his whole life. Therefore, in perinatal medicine it can be extremely difficult to make an accurate diagnosis.
PAPP-A – pregnancy associated protein-A
This is a protein produced by the placenta in the body of a pregnant woman, responsible for the immune response during pregnancy, and is also responsible for the normal development and functioning of the placenta.
| Normal levels of PAPP-A, depending on the stage of pregnancy: | Indicator deviations | |
| weeks | PAPP-A, honey/ml | “-” As its level decreases, the risk of the following pathologies increases:
“+” An isolated increase in the level of this protein has no clinical or diagnostic significance. |
| 10-11 | 0,45 – 3,73 | |
| 11-12 | 0,78 – 4,77 | |
| 12-13 | 1,03 – 6,02 | |
| 13-14 | 1,47 – 8,55 | |
What does biochemical analysis show?
When studying this biomaterial, doctors first of all look at the content of human chorionic gonadotropin, or hCG. If its level is low, it means there is a pathology of the placenta. If the hCG level, on the contrary, is high, the fetus may have chromosomal abnormalities. It may also indicate a multiple pregnancy.
The analysis also allows you to find out the level of protein A, or PAPP-A. If its content is reduced, there is a possibility that the fetus will develop Down syndrome and other so-called trisomies. A reduced content of PAPP-A may indicate fetoplacental insufficiency or malnutrition. It also indicates a threat of miscarriage.
If the protein level is elevated, it means that the fetus or placenta is too heavy, or the latter is located too low. To find out what exactly is causing the increased or decreased levels of PAPP-A in a woman’s blood during pregnancy, she is sent for amniocentesis, or amniotic fluid testing. It is this analysis that will confirm or exclude gene pathologies.
Is high hCG level dangerous for pregnancy?
The danger of a high hCG level at 1 screening depends on the reasons for its increase. So, if an excess of the hormone norm is caused by diabetes mellitus, then there is a risk of an unfavorable course of pregnancy, disturbances in the development of the fetus, up to and including intrauterine death. With this diagnosis, planned prenatal hospitalization is required.
Toxicosis, being the cause of exceeding the hCG norm, can occur in a mild form, in this case the degree of danger to the health of the mother and fetus is not critical, but you still need to be under the supervision of doctors. Remember that toxicosis sometimes takes a severe course, which affects the general condition of the expectant mother and the normal functioning of her organs and systems.
Tumor diseases of organs and placenta require immediate medical consultation and medical intervention. In particular, with hydatidiform mole, the pregnancy outcome is the most unfavorable with immediate aspiration of the contents of the uterine cavity. After removal 2 weeks later, hCG is almost not detected, but over time it continues to be detected up to three times. There can often be a relapse, so it is necessary to monitor the condition of patients throughout the year.
Choriocarcinoma that develops against the background of a hydatidiform mole or a couple of months after an abortion and childbirth also poses a serious threat to a woman’s health. Unfortunately, the consequences can be sad, but often the uterus is preserved. With this pathology, observation of patients continues for 2 years.
To prevent the development of complications, a woman is identified as a risk group, so that diagnostic and therapeutic measures can be carried out in a timely manner.
Women at risk include:
- genetic pathology in the family;
- diabetes mellitus in a woman or in the family;
- woman's age over 35 years;
- a history of frozen (non-developing) pregnancy;
- spontaneous abortion.
Do not panic ahead of time after the first test result. Perhaps all the recommendations for passing it correctly were not followed, or an error occurred in the laboratory.
If the hCG level is higher than the due date, then a dynamic test is prescribed. Along with a biochemical blood test, ultrasound, additional methods, and consultations with specialists are performed.
Important! The examination must be carried out in the same laboratory. If you donate blood in different laboratories, the values may differ.
If there is a suspicion that the cause of high hCG levels is chromosomal abnormalities, the woman may be offered to undergo an amniocentesis procedure. This procedure is surrounded by many myths and fears of expectant mothers, but in reality it causes more psychological than physical harm. The amyocentesis procedure for more than 16 weeks carries virtually no risk of negative consequences.
Remember that the result of blood tests does not give an accurate result, and there is always a chance that the child is absolutely healthy even with abnormal tests. The probability of a true result of invasive procedures is quite high (up to 99%).
After additional examinations and consultations, the woman, together with the doctor, will decide whether to continue the pregnancy and the tactics for its management or its termination.
We invite you to read: The first days of pregnancy: what happens in a woman’s body immediately after conception?
Vladlena Razmeritsa, obstetrician-gynecologist, especially for Mirmam.pro
Useful video
During artificial insemination, hormone levels are similar to those during natural conception. After IVF, monitoring the rise of hCG is extremely important. This way, successful implantation can be determined, which will allow continued pregnancy support. If growth of the hormone is not observed, then the support is canceled, and after the body is restored, a new protocol is started.
The IVF procedure has helped many find the joy of motherhood
During IVF, the natural mechanisms of conception are disrupted. Because of this, the results of hCG analysis are often outside the normal range. In each specific case, a doctor should determine the risks. Elevated hormone levels after IVF are not uncommon. The procedure involves the transfer of several embryos. Often two take root, with the result that the analysis results show a doubling of the norm.
HCG analysis can be done on the tenth to fourteenth day after embryo transfer. The exact time of the test is determined by the doctor. It depends on many factors. For example, it is important to consider how many days the embryo spent in vitro.
It is necessary to monitor hCG dynamics after IVF until delivery. After the procedure, there is a high probability of self-abortion (this will be indicated by low hormone levels) and the development of fetal pathologies (high levels).
Sometimes the fixation of the “pregnancy hormone” and its subsequent growth occurs when there has been no conception. This test result is called a false positive. The following factors can contribute to the production of hCG and increase its level in the absence of pregnancy:
- relapse of hydatidiform mole;
- tumor-like neoplasms (on the organs of the reproductive system, in the lungs, kidneys);
- taking hormonal drugs.
The hormone concentration may be a residual phenomenon. The indicator does not immediately return to normal after spontaneous termination of pregnancy or abortion.
The presence of the hormone in the blood, and especially its high concentration in the absence of pregnancy, indicates a malfunction in the body. It is important to identify the exact cause of this phenomenon as soon as possible, so you should not delay going to the doctor.
HCG: definition of the concept
HCG is a specific hormone familiar to all women who are in an “interesting situation.”
Analysis of the concentration of the substance is mandatory for pregnant women. The chemical composition of the hormone is a glycoprotein. It consists of alpha and beta subunits. Beta-hCG allows you to determine pregnancy and monitor its progress. The production of human chorionic gonadotropin begins only after successful conception. The exception is cases of cancer, when hCG is found in the blood of non-pregnant women and even in the blood of men. However, this is a pathological phenomenon, while the presence of the hormone in pregnant women is the norm.
HCG is produced by the fetal membrane. Hormone production begins immediately after implantation of the fertilized egg. By the presence of hCG, you can determine whether conception occurred in this cycle. The detection of a hormone in the blood indicates an “interesting situation” when other methods of determination are still unable to say anything. Test strips also react to hCG. However, the informative amount of the hormone in the urine appears later than in the blood.
The “pregnancy hormone” plays a key role in the successful gestation and development of the fetus. At the beginning of the period, it is important that the concentration of hCG increases. This is necessary for the preservation and normal development of pregnancy. Gonadotropin is responsible for:
- functioning of the corpus luteum;
- production of important hormones - progesterone, estrogens;
- absence of menstruation;
- protection of embryonic cells from attacks by the female immune system (decreased immune functions prevents fetal rejection).
Young mother and newborn baby
After the laying of the organs, the hormone ensures the proper functioning of the baby’s gonads and adrenal glands in the prenatal period. If the egg was fertilized by a Y-sperm, then hCG promotes the synthesis of testosterone. Thanks to this, the fetus is formed according to the male type.
Although hCG should increase until the 11th week, its excessive concentration in the blood is not a good sign. The hormone is a marker of genetic diseases of the fetus: a significant increase increases the likelihood of detecting chromosomal abnormalities in the baby. High levels may indicate pregnancy complications.