In the first place among the anomalies of labor is the weakness of labor. Weak labor is a pathology of the labor process, consisting of weak, short-lived and fading contractions. When labor is weak, contractions are weak, infrequent, short, and the rate of opening of the uterine pharynx is less than 1 cm per hour (and for multiparous women, less than 1.5-2 cm per hour). Smoothing of the cervix and its dilation occurs at a slow pace and therefore therapeutic measures will be required as soon as the diagnosis of weak labor is established. Currently, the Stein-Kurdinovsky birth-stimulating therapy regimen using oral quinine and intramuscular oxytocin is not recommended, which is due to the fact that the effectiveness of oral quinine followed by the administration of oxytocin is very low and poorly regulated.
Therefore, at present, only a scheme of intravenous administration of oxytocin or prostaglandins with a possible combination is used (enzoprost or prostenon is administered for 2 hours, then an ampoule of oxytocin is added and uterotonics are administered within 3-4 hours with an assessment of labor-stimulating therapy, so it is imperative to treat weakness of labor in a timely manner. The diagnosis of weak contractions should be made no later than 3 hours from the onset of contractions and treatment should begin immediately with active drugs.
NB!
Labor induction
is a therapeutic measure in the absence of contractions.
Labor stimulation therapy
- in the presence of weak contractions.
If you stick to medical statistics, then weak labor is a fairly common phenomenon - 10% of all births.
But is this really so? After all, in the average maternity ward, everything is on stream. And they don’t really listen to the inner feelings of women in labor. Doctors quite often, without special need, just to be on the safe side and speed up the process, resort to stimulation of labor, citing its weakness.
Weakness of labor is characterized by the presence of contractions that are weak in strength, short in duration and rare in frequency. During such contractions, the opening of the cervix and the movement of the fetus through the birth canal occurs slowly. It can be primary, secondary and appear only during the period of exile.
Cyclic weakness of labor occurs in the risk group which includes the following pregnant women:
1. elderly and young women
2. women with hyperextension of the uterus (large fetus, multiple births, polyhydramnios).
3. Multiple births, multiple pregnancies, numerous abortions with curettage, that is, in the presence of dystrophic and inflammatory changes in the myometrium.
4. In women with menstrual dysfunction and hormonal balance
5. hypertrichosis obesity
Cyclic weakness of labor develops in the group in which the uterus is not able to respond to normal impulses from the pacemaker. There may be a lack of impulses or a lack of receptors.
The diagnosis of weak labor is made on the basis of:
1. characteristics of contractions: weak, short
2. insufficient dynamics of cervical dilatation (normally 1 cm per hour) - 2-3 cm per hour.
3. To clarify the dynamics, external methods of determination and vaginal examination data are used
4. The diagnosis must be made within 2-3 hours.
Weakness of labor leads to protracted labor, complicated by premature or early discharge of amniotic fluid, leading to fetal hypoxia. Increased risk of purulent-septic complications. In the third stage of labor it causes hypotonic bleeding.
What does weak labor mean?
Weak labor is a condition of the body characterized by insufficient strength of contractile uterine activity, frequency and duration. As a result, contractions are rare and short, and they are ineffective. All this leads to a slow opening of the cervix and the passage of the fetus through the birth canal.
Weak labor can lead to negative consequences
This condition refers to anomalies of generic forces. It is observed in 10% of cases of all unfavorable births. As a rule, pathology is diagnosed during the first birth, less often observed during the second or third.
Reasons why such an anomaly develops
Several factors can lead to the development of weakened labor activity:
- Pathologies of the endocrine glands or metabolism, such as: overweight, underactive thyroid gland, diabetes.
- Excessive stretching of muscle fibers, which is more often observed in multiple pregnancies, large fetuses, and polyhydramnios.
- Changes in the structures of the uterine wall, which can form due to inflammation the woman once suffered in this area.
- Incomplete uterine scar, which formed after the completion of a previous birth by cesarean section or due to the removal of fibroids.
- Abnormal development of the uterus or its underdevelopment, present throughout the life of the expectant mother.
- Post-term pregnancy or, conversely, early onset of labor.
- The presence of Rh conflict, intrauterine infection or delay in the development of the baby.
Weak contractile activity is often associated with the age of the pregnant woman, when she is under 18 or over 30 years old. The impact of psycho-emotional stress associated with the upcoming birth of a baby and the presence of negative emotions, expressed fear and anxiety is also important.
Classification
Pathology is classified depending on the time of its appearance, and there are two types: primary and secondary. The primary form is characterized by short, ineffective contractions from the beginning of the labor process, while the uterus relaxes for a long time. The secondary form is diagnosed when contractions weaken and shorten after some time of sufficient intensity and duration.
The primary form is more common, its frequency is 8-10 percent. Usually the secondary form is detected at the end of the period of dilatation or during the expulsion of the fetus; it occurs only in 2.5% of cases of all births.
Experts also note weakness in pushing, observed in multiple births or in obese women with segmental and convulsive contractions. Convulsive uterine contraction is characterized by a prolonged contraction of the uterus (more than 2 minutes), segmental - the uterus does not contract all, but only in individual segments.
What happens during postterm pregnancy?
With true postterm pregnancy, pathological changes develop in the uterus, placenta, amniotic fluid and in the condition of the fetus, which progress as the gestational age increases and adversely affect the course and outcome of late birth.
Uterus
. There is no biological readiness of the body for childbirth, which, along with the unpreparedness of the central nervous system, is manifested by the unpreparedness of the cervix for childbirth (there is no shortening, loosening, or increase in the patency of the cervical canal) and functionally low activity of the uterine body muscle, which is accompanied by a delayed onset of labor.
Placenta
. After the end of the normal pregnancy period, processes of “aging” of the placenta occur, which is accompanied by changes in its cellular structures: sclerosis, hemorrhage, deposition of calcium salts, a decrease in the functionally active surface of the placenta, a decrease in intraplacental blood flow, which leads to a deterioration in metabolic processes in the placenta. All these disorders lead to a decrease in the transport of oxygen and nutrients, disruption of the normal conditions of intrauterine development of the fetus, which can cause chronic fetal hypoxia, intrauterine growth retardation, or a combination of both. Along with aging, the formation and growth of new structures (villi) of the placenta is noted as a manifestation of compensatory adaptive capabilities. This is why in most cases of post-term pregnancy the fetus continues to develop normally and is born healthy.
Chronic hypoxia (oxygen deficiency) of the fetus
. The main cause of chronic fetal hypoxia during postmaturity is placental insufficiency. It is especially pronounced when the pregnancy is over 2 weeks, which is associated with impaired blood circulation in the placenta, a decrease in oxygen consumption by the placenta and an increase in carbon dioxide content. The fetus is overripe, its need for oxygen increases, in response to hypoxia there is a change in the motor activity of the fetus (it can either increase or decrease), and the fetal heart rhythm is disturbed. Fetal hypoxia can cause increased intestinal motility, relaxation of the anal sphincter and the release of meconium (original feces) into the amniotic fluid. This can also be facilitated by compression of the umbilical cord, which during pregnancy can be “skinny” due to a small amount of Wharton’s jelly, a jelly-like substance that is normally contained in sufficient quantities between the vessels of the umbilical cord.
Meconium is a dark green, viscous substance that fills the fetus's large intestine. When meconium pigments enter the amniotic fluid, they turn it green, which indicates a threatening condition of the fetus. With increasing hypoxia, excitation of the fetal respiratory center may occur, leading to an increase in its intrauterine respiratory movements and the entry of amniotic fluid into the fetal respiratory tract. Subsequently, this necessitates resuscitation measures and provokes the development of pneumonia in the newborn.
Amniotic fluid
. With true postmaturity, the pathological condition of the placenta and fetus, a quantitative and qualitative change in the amniotic fluid occurs. Oligohydramnios is a characteristic complication of post-term pregnancy; the amount of water decreases by 2-3 times and can reach 50-100 ml.
At the early stages, the waters lose their transparency and become cloudy due to the large amount of cheese-like lubricant and fetal skin flakes; at a later stage, the waters turn green or yellow, depending on the duration of the presence of meconium impurities in the amniotic fluid. The bactericidal properties of amniotic fluid, which provide protection against bacteria, are reduced, which can lead to infection of an overripe fetus and even its death.
Fetus
. Depending on the period of post-gestation, the weight of the fetus increases to 4000 g or more, its dimensions increase - length by 2-3 cm, volume of the head by 1.5-2 cm. The bones of the skull become whiter dense and massive, the size of the sutures and fontanelles decreases, resulting in mobility skull bones relative to each other (configuration) is significantly reduced. An increase in metabolic processes in the mother activates metabolic processes in the placenta, and prolongation of pregnancy ensures that the fetus is in favorable environmental conditions, which leads to an increase in height and weight indicators.
In late births, a large fetus is not the rule. Often, low birth weight babies are born with signs of malnutrition (stunted growth) as a consequence of progressive placental insufficiency.
In the case of a post-term pregnancy, the skin of the fetus begins to lose its original lubrication, and with the loss of this protective fatty layer, the skin of the fetus comes into direct contact with the amniotic fluid, begins to peel off and wrinkle.
Who is at risk
The risk of developing pathology increases in the following cases:
- too young age (under 18 years old) and women in labor over 35 years old;
- a large number of abortions with curettage in history;
- multiple births;
- a large number of births in the anamnesis;
- hormonal imbalance and menstrual dysfunction;
- excess body weight;
- hypertrichosis;
- the presence of uterine hyperextension caused by multiple births, polyhydramnios or a large fetus.
Causes
Why is there weak labor? Here are the main factors causing this condition:
- polyhydramnios;
- large fruit;
- post-term pregnancy;
- overweight;
- hormonal disorders;
- fear of the first birth;
- multiple pregnancy;
- metabolic disease;
- problems with the endocrine system;
- physiological features, for example, a narrow pelvis of a woman in labor, a flat bladder;
- pathological processes that occur in the uterus;
- overwork;
- lack of sleep.
- any stress experienced.
Many pregnant women wonder if labor is weak during the first birth, then what to expect from the second? No specialist can definitely answer this question, since each new birth may differ from the previous ones. Even if you are giving birth for the fourth or fifth time, the whole process may be different from your previous experience.
Every woman needs the right attitude for childbirth
Causes of weak contractions
Certain reasons are necessary for the formation of weakness of labor. Factors that contribute to this pathology are divided into a number of groups:
Obstetric complications
This group includes:
- prenatal rupture of water;
- disproportion between the sizes of the fetal head (large) and the mother’s pelvis (narrow);
- changes in the walls of the uterus caused by dystrophic and structural processes (multiple abortions and uterine curettage, uterine endometriosis, fibroids and uterine surgeries);
- rigidity (inextensibility) of the cervix that occurs after surgical treatment of cervical diseases or damage to the cervix during childbirth or abortion;
- polyhydramnios and multiple births;
- large size of the fetus, which overstretches the uterus;
- incorrect location of the placenta (previa);
- presentation of the fetus with the pelvic end;
- anemia;
- gestosis.
In addition, the functionality of the amniotic sac is of great importance in the occurrence of weakness (with a flat amniotic sac, for example, with oligohydramnios, it does not act as a hydraulic wedge, which inhibits cervical dilatation). We should not forget about the woman’s fatigue, asthenic body type, fear of childbirth and mental and physical stress during gestation.
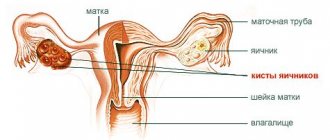
Pathology of the reproductive system
Sexual infantilism and congenital anomalies of the uterus (for example, saddle-shaped or bicornuate), chronic inflammation of the uterus contribute to the development of pathology. In addition, a woman’s age (over 30 and under 18) affects the production of hormones that stimulate uterine contractions.
This group also includes menstrual cycle disorders and endocrine diseases (hormonal imbalance), recurrent miscarriage and disturbances in the formation of the menstrual cycle (early and late menarche).
Extragenital diseases of the mother
This group includes various chronic diseases of women (pathology of the liver, kidneys, heart), endocrine disorders (obesity, diabetes, hypothyroidism), numerous infections and intoxications, including bad habits and industrial hazards.
Factors due to the fetus
Intrauterine infection of the fetus and developmental delay, fetal malformations (anencephaly and others), post-term pregnancy (overripe fetus), as well as premature birth can contribute to weakness. In addition, Rh conflict during pregnancy, fetoplacental insufficiency and fetal hypoxia are important.
Iatrogenic causes
This group includes “hobby” with birth-stimulating drugs that tire a woman and disrupt uterine contractile function, neglect of labor pain relief, unjustified amniotomy, as well as rough vaginal examinations.
As a rule, not one factor, but a combination of them, plays a role in the development of weakness of contractions.
Symptoms
The clinical picture of weak labor is as follows:
- Primary weakness - with it, contractions immediately have a short duration and low efficiency, and are practically painless. The periods of relaxation are quite long and almost do not cause the opening of the uterine pharynx. Most often, these signs appear after a pathological preliminary period. Typically, expectant mothers complain of water breaking and weak contractions, which means premature or early rupture of amniotic fluid.
- Secondary weakness - this symptom is less common; its distinctive feature is the weakening of contractions after an interval of effective labor and dilatation of the cervix. As a rule, it occurs at the end of the active phase when the uterine pharynx opens to 5-6 cm or during pushing. Initially, contractions are intense and frequent, but gradually lose strength and become shorter, and the movement of the presenting part of the fetus slows down.
- Weakness of pushing - this condition is usually characteristic of women who have given birth a lot and often, suffer from obesity or divergence of the abdominal muscles. This symptom can also be triggered by physical or nervous exhaustion. They manifest themselves as ineffective and weak contractions and attempts, as a result of which it is difficult for the fetus to move along the birth canal, which causes hypoxia.
Possible complications
In case of incorrect choice of delivery strategy during weak labor, the following complications are possible:
- abuse of stimulant drugs can lead to discoordinated labor and fetal hypoxia.
- prolonged standing of the presenting part of the fetus in one plane of the small pelvis can lead to compression of the soft tissues, which leads to the risk of genitourinary fistulas. On the part of the fetus, this can lead to impaired cerebral circulation and cerebral hemorrhage.
- Women with weak labor in the postpartum period have a risk of hypo- and atonic bleeding and infectious diseases.
Diagnostics
To make a diagnosis of “weak labor,” doctors take into account:
- the nature of uterine contractions - their strength, duration of contractions and relaxation time between them;
- as the cervix opens, a slowdown in this process is observed;
- advancement of the presenting part - absence of forward movements, the head remains in each plane of the small pelvis for a long time.
An important role in diagnosing weak labor forces is played by maintaining a partogram of labor, thanks to which the process of cervical dilatation and its speed is clearly shown. In primiparous women in the latent phase in the 1st period, the uterine os opens approximately by 0.4-0.5 cm per hour, in multiparous women - 0.6-08 cm per hour. As a result, the latent phase in women who are giving birth for the first time lasts approximately 7 hours, in multiparous women - up to 5 hours. Weakness is diagnosed when the delay in cervical dilatation is about 1-1.2 cm per hour.
Contractions are additionally assessed. In the case when in the 1st period their duration is less than half a minute, and the intervals between them exceed 5 minutes, this means primary weakness. Secondary weakness is said to occur when contractions last less than 40 seconds at the end of the first period and during the process of expulsion of the child. It is also important to monitor the condition of the fetus, since prolonged labor leads to hypoxia.
Diagnosis of pathology
If there is no dynamics of stretching of the uterine pharynx, a partogram is prescribed. The procedure is a graphic recording of the progress of labor, with which you can monitor the dynamics of cervical dilatation, the state of amniotic fluid and the movement of the head through the birth canal.
To prevent oxygen starvation in the fetus, cardiotocography is used. The method allows you to find out the heart rate of the fetus and determine the tone of the uterine muscles.
Cardiotocography
What to do
How does labor begin? If the pregnancy is post-term, but the woman’s body is ready for delivery, then the specialist first performs an amniotomy. This procedure is performed only if the cervix is dilated by 2 cm or more.
As a rule, after opening of the amniotic sac, labor increases. After the procedure, the woman in labor is monitored for several hours, after which, if the amniotomy does not produce any results, drug stimulation is used.
The main method of drug stimulation of uterine contractions is the use of uterotonics: oxytocin and prostaglandins, which are administered intravenously. At the same time, the condition of the fetus is monitored using CTG.
In some cases, medicated sleep can be used, which is aimed at restoring the strength of the woman in labor; its duration is approximately 2 hours. It is carried out with the help of analgesics and only after consultation with an anesthesiologist. This technique is used quite rarely and only when the benefit outweighs the possible harm.
If all the measures taken do not give a positive result, an emergency caesarean section is prescribed.
To minimize the possible negative consequences of weak labor, it is important to listen to the doctor’s recommendations and strictly follow them.
Harbingers of childbirth
The first signals about an imminent meeting with the child appear approximately 4 weeks before his birth.
The main harbingers of an early birth:
- Abdominal prolapse
This phenomenon is usually observed 2 weeks before the onset of labor.
It is due to the fact that the baby's head enters the mother's pelvis. Due to this, the diaphragm lowers and the stomach changes its position.
- Removal of the mucus plug
The time when this phenomenon can occur varies.
The plug has the appearance of a mucous discharge with blood streaks.
For some, it goes away 10 days before giving birth. Sometimes the plug comes off immediately during childbirth.
- Cleansing the body
A few days before giving birth, a woman activates processes aimed at natural cleansing of the body.
Urination and stool become more frequent, during which the woman loses several kg of weight.
- Training contractions.
These are pulling sensations of a girdle nature in the abdomen and lower back.
They are not painful and occur about 3 weeks before the onset of labor.
How to intensify contractions
Sometimes the following actions will help intensify contractions:
- Calm down, breathe correctly, take certain positions during contractions, and if possible, do self-massage.
- Move as much as possible or jump on an exercise ball.
- If you need to be in a horizontal position, then lie on the side where the back of the fetus is located - this will increase the contraction of the uterus.
- Monitor the condition of your bladder and empty it every 2 hours.
- An empty bladder makes contractions worse. If you cannot go to the toilet on your own, use a catheter.
Remember, you can follow these recommendations only with your doctor's permission.
Contraindications
Conservative therapy is prohibited in the following cases:
- the presence of a scar on the uterus, for example, after a caesarean section;
- narrow pelvis of a woman in labor;
- large fruit;
- true post-term pregnancy;
- individual intolerance to uterotonic drugs;
- the child is in a pelvic rather than cephalic presentation;
- intrauterine fetal hypoxia;
- if the woman in labor is over 30 years old and this is her first birth;
- burdened gynecological history;
- burdened obstetric history.
In such cases, birth is carried out using an emergency caesarean section.
Cleaning the house in the last weeks of pregnancy will help speed up the onset of labor
Diagnosis of post-term pregnancy
The diagnosis of true post-term pregnancy is based on the following data: determination of the expected due date, symptoms of post-term pregnancy based on the results of external and internal obstetric examination, as well as indicators of additional research methods (tests, ultrasound diagnostics and Doppler ultrasound - study of blood flow in the vessels of the placenta and fetus, amnioscopy - examination amniotic fluid using an optical device inserted into the cervix). The final diagnosis is confirmed only after birth when examining the baby and placenta.
In a newborn baby during postmaturity, signs of fetal overmaturity are revealed: dryness, sagging and maceration (wrinkling) of the skin, especially on the arms and legs (“bath” feet and palms), absence or reduction of cheese-like lubricant, which is determined only in the neck and inguinal folds, lengthening of the nails, increased density of the cartilage of the auricles, coloring of the skin green in the presence of meconium in the waters, poorly defined configuration of the head, dense bones of the skull, narrow sutures and small size of the fontanels, large size of the fetus, less often - fetal malnutrition, decrease in subcutaneous fatty tissue, formation of folds, decreased skin turgor - “senile” appearance of the child).
When examining the placenta, an increase in the weight of the placenta by 100 g or more, its lobulation, multiple areas of lime deposits and fatty degeneration are noted, the membranes and umbilical cord may be stained green, a decrease in the thickness of the placenta and a decrease in the amount of Wharton's jelly in the umbilical cord.
Prevention
Is it possible to ensure that childbirth takes place without complications? You cannot directly influence the process of childbirth, but you can prepare for it. For this:
- From the last month of pregnancy, start taking vitamins B6 and B9 (folic acid), as well as vitamin C.
- Start mentally setting yourself up for a successful outcome of the birth.
- If possible, attend courses for expectant mothers.
- Remember, during childbirth, not only you experience difficulties, but also the child.
If anyone among your relatives has experienced prolonged labor, follow these recommendations (but only after your doctor’s permission):
- From 34-36 weeks of pregnancy, do what was prohibited during pregnancy: actively clean, wash floors at an angle, lift heavy objects, take a hot bath.
- Drink raspberry leaf tea 2-3 glasses a day.
When does labor begin?
The expected date of birth does not always coincide with the actual day of birth of the child.
Some give birth exactly on time, some earlier, and some much later than the set date. Consequently, the question arises: “What determines the onset of labor?”
The duration of bearing a child is individual for each woman and depends on the length of her menstrual cycle.
- If the cycle is 21 days, then there is a high probability of having a baby at 38 weeks of pregnancy;
- If there are more than 30 days between periods and the cycle is long, then the woman will most likely give birth at about 42 weeks.
The normal period for the birth of a child is considered to be 40 weeks.
From 37 weeks, babies are considered full-term, but there is no need to rush into their birth.
During this period, the active formation and maturation of the child’s lungs still occurs.
A pregnancy period of more than 40 weeks is considered pathological and requires medical supervision.
If the pregnancy proceeds without complications and the child feels well, then doctors will not interfere. However, as a result of transplantation, the risk of intrauterine infection of the fetus increases due to the passage of original feces.
In modern obstetric practice, a pregnancy period of up to 42 weeks is considered normal, and beyond that requires stimulation of labor.