Why is an anti-Rhesus immunoglobin injection administered during pregnancy?
Today, doctors use immunoglobulin injections during pregnancy, for example, it is given to those who have problems with normal pregnancy. The drug is administered as a dropper or injection. It is made on the basis of plasma, which, in turn, is an active substance that is purified and concentrated. It acts on the process of immunomodulation and immunostimulation. The drug helps the body resist various viruses and other microorganisms that are causative agents of various ailments. Another feature of the drug is that it replenishes the level of special antibodies that reduce the development of infectious diseases in girls with primary and secondary immunodeficiency.
When do they do it?
Anti-Rhesus immunoglobulin is routinely administered as a means of preventing sensitization in the presence of the above indications at 28-30 weeks of pregnancy, and then within 72 hours after birth, if it is confirmed that the newborn has a positive Rh factor.
Normal human immunoglobulin for miscarriage is administered during the conception cycle or in the first weeks after receiving a positive pregnancy test. According to indications, the drug can be administered later at any other time.
Doctors carefully weigh the benefits and harms, trying not to resort to these measures unnecessarily during the patient’s pregnancy.
Antibody preparations must be warmed to room temperature before administration. If a dropper is given, then it is administered very slowly so that a pseudo-allergic reaction does not occur; such consequences, unfortunately, are possible if immunoglobulins are administered quickly. Sometimes it becomes necessary to divide the dose into 2-3 droppers and administer it in several doses - everything is individual, in each specific case the decision is made by the doctor both on the type of administration and on the dosage.
Indications
The drug is administered inside the body using a dropper in a hospital. It is never prescribed on an outpatient basis. The dosage is adjusted depending on the complexity of the case, the duration of pregnancy and the process, the purpose of use. Despite the fact that it is widely used, no studies have been identified on its effect on the fetus. Medical practice says that it generally does not lead to pathological processes.
There are several types of this substance, namely anti-D immunoglobulin and “normal”. These are completely different substances. Each of them has its own indications for use.
One or the other drug is prescribed only in extreme cases, for example, when there is a real threat of premature labor or the risk of losing a child in the early stages. In addition, it is used if there is a risk of a pathological infection, as well as in cases of Rh conflict.
What it is?
Immunoglobulin is antibodies that have been isolated from donor blood, purified and processed in a special way. In the human body, antibodies (or immunoglobulins) are produced as a response to the penetration of a particular infection into this body. For each antigen protein, human immunity is capable of forming its own immunoglobulins, the task of which is to protect the body from a specific pathogen and help killer cells destroy the threat.
There are different immunoglobulins - against infections and parasites, antitoxic antibodies. Rabies vaccine and influenza vaccine are immunoglobulins; anti-Rhesus immunoglobulin is a means of protecting the baby and mother.
If there is a Rh conflict during pregnancy, human immunoglobulin is a broad-spectrum drug that will help a woman bear a child against the background of immunodeficiency.
Immunoglobulin is available in the form of injection solutions. Droppers with it are placed and injections are given exclusively in hospitals; such injections are not performed at home.
Pros and cons of the drug
Like all drugs, anti-Rhesus immunoglobulin during pregnancy has its pros and cons.
The disadvantages of immunoglobin are its side effects, which are noticed by all women in 55% of cases. So she may develop ailments in the form of:
- weaknesses;
- chills;
- increasing body temperature;
- cough;
- sore throat;
- dizziness;
- pain in the back of the head and temples;
- nausea;
- pain in the center of the abdomen;
- mood swings.
In addition, more serious complications may occur in the form of vomiting, diarrhea, aches and pain in the joints and lower back. In addition, a rapid heartbeat and increased pulse may appear. In addition, it has not been proven that the fetus will not have pathological manifestations.
The advantages are that it helps eliminate:
- threat of miscarriage;
- ectopic pregnancy;
- artificial abortion;
- amniocentesis;
- severe injury in the abdominal area;
- immunodeficiency;
- blood in the fetal circulation.
Is an immunoglobulin injection required after childbirth?
It is considered this way: within no more than three days after the birth, a woman needs to be injected with immunoglobulin. The earlier the better. During childbirth, blood cells enter the mother's bloodstream. If this is done, you don’t have to worry that a conflict will arise during your second pregnancy. The fact is that during the first pregnancy the risk of Rh conflict is lower than during the second.
The administration of immunoglobulin is also indicated:
- After completion of an ectopic pregnancy,
- After miscarriages, missed pregnancies and tragic births for the baby,
- After a difficult birth, during which the woman suffered placental abruption.
In this case, the dose of immunoglobulin is adjusted by doctors; it depends on the possible exchange of blood between the woman and the child. The standard dose is considered to be 200-300 mcg, but after surgery (caesarean section), as well as the situation of manual separation of the placenta, the dosage increases by one and a half, or even twice. If the dosage is incorrect, then not all the red blood cells in the mother's blood will be bound, and then the remaining portion will, one way or another, have a dangerous immune response.
What could be the consequences?
Anti-Rhesus immunoglobulin is almost always well tolerated by women. In addition to the symptoms and complications listed above, skin irritation at the injection sites, pain in this area, and rarely anaphylactic shock may also appear.
It is practically safe for healthy women. The consequences of immunoglobulin during pregnancy can be observed in women with individual intolerance to the drug or with severe allergic reactions to similar drugs, antibodies that interfere with the normal course of pregnancy. In the latter case, it makes no sense to start treatment with this drug, since the anomaly that has arisen in the body due to the development of antibodies should be treated.
Contraindications and side effects
The drug is not prescribed in a number of cases:
- hypersensitivity to the drug;
- severe allergy to any blood products;
- Rh negative with sensitization and the presence of antibodies;
- Rh positive.
If during injection or infusion into a vein the dosage and rate of delivery of the medicine are observed, there will be no serious side effects. Within an hour the following are observed:
- malaise;
- headache;
- chills;
- slight increase in temperature.
Immunoglobulin is normally tolerated by patients, but sometimes a woman may be bothered by:
- cough;
- nausea and vomiting;
- dyspnea;
- hyperthermia at the site of needle insertion;
- excessive salivation and sweating;
- chest and stomach pain;
- allergy;
- weakness;
- aching joints, like flu;
- facial hyperemia.
How to use injections for Rhesus conflict
Rhesus conflict, which has not yet led to the development of antibodies that prevent the child from developing in the womb, can still be cured with immunoglobulin injections.
The injections are given in the hospital, before which the drug is kept in the room for about two hours. Then the injection is given according to the instructions given in the instructions. It cannot be stored open or in direct contact with the sun. If it has been stored this way, it cannot be used. If a woman has already given birth, then two days after this, she is injected with this drug in a dose of 350 mcg to 650 mcg. If the substance is used to preserve the fetus, it is administered intramuscularly to the woman lying on the couch. At the same time, doctors recommend that a pregnant woman take vitamin complexes, first consulting a doctor about taking them.
The price of the anti-Rhesus immunoglobulin vaccine used during pregnancy starts from 3,500 rubles.
What is immunoglobulin, in what cases is the drug used?
Blood plasma consists of 5% proteins. 3% of blood proteins are immunoglobulins, substances that support the body's immunity. They also penetrate into other fluids - for example, breast milk, saliva, urine.
A person has 5 classes of immunoglobulins that fight:
- with pathogenic bacteria, viruses and other harmful microbes;
- with toxic substances;
- with allergies.
As soon as the immune “guardians of health” detect foreign cells or pathogenic microorganisms, they attack the “enemies” and destroy them. At the same time, immunoglobulins do not pose any danger to other cells.
Immunoglobulins circulate in the bloodstream and vigilantly monitor the “purity” of the blood; When foreign agents appear, they are mercilessly eliminated
Blood delivers immune proteins (also called antibodies) to distant parts of the body; To combat pests - antigens - a low concentration of antibodies is required.
For the first time, immunoglobulin was obtained from donor blood serum in 1952 - to save the lives of people who completely lacked antibodies. For deciphering the chemical composition of immunoglobulins, scientists J. Edelman and R. Porter were awarded the Nobel Prize in 1972.
The protein fraction responsible for immunity is isolated from the serum or blood plasma of healthy donors (first of all, care is taken to ensure that there are no AIDS, hepatitis B and C). Human immunoglobulin has found wide application in medicine and is used for:
- immunodeficiency;
- severe bacterial and viral infections;
- autoimmune diseases (for example, thyroid pathologies);
- severe allergies;
- AIDS in children.
Immunoglobulin is contained in vaccinations against rubella, measles, and mumps.
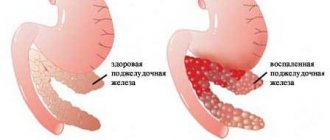
A separate type of drug, informally called anti-Rhesus immunoglobulin, is prescribed exclusively to expectant mothers with an Rh-negative factor if doctors determine a “conflict of interest” in the process of mixing blood that threatens the development of the baby. This drug does not contain antibodies that destroy bacteria or viruses; only immune cells to substances in Rh-positive blood - the so-called D-antigens.
Let’s figure out what the danger of a collision between “plus” and “minus” lies.
Prevention of Rhesus conflict
In order to prevent Rh conflict from occurring, before and during pregnancy you need to donate blood for antibodies, sugar and other important indicators, while doing regular diagnostics and conducting ultrasound examinations that will help determine whether the fetus has abnormalities or not. According to medical statistics, only 15% of the population has a negative Rh factor. The very first injection is the one given at 28 weeks. It is repeated only after six weeks.
Why this particular time? In the seventh month of pregnancy, any woman has a chance to give birth to a premature baby. If there is a risk of this process, then the woman is admitted to hospital and certain actions are taken.
How often is the drug administered? Many doctors act depending on the situation, the general condition of the patient and her body. If a woman is healthy, she is rarely given an injection; if she feels unwell and has some other problems, she is given an injection constantly. If a woman is no longer able to bear a child, she undergoes a caesarean section. The woman monitors the timing of drug administration independently.
What are Fluomizin suppositories used for: indications for use and instructions for the drug.
Find out the instructions for using the drug Clexane from our article.
Should I take Mukaltin during pregnancy: https://mamafarma.wpengine.com/cold/mukaltin.html.
Analogues of the drug
The pharmaceutical market offers a number of products with similar effects; The Russian drug is officially called Anti-Rhesus Human Immunoglobulin. As for the others, the names and countries of origin are different, but the principle of operation is the same. It is difficult to say which medicine is better: imported ones have a reputation of being of higher quality and are usually more expensive, although the active substance is the same everywhere - anti-Rh human immunoglobulin.
All drugs are sold by prescription only.
Table: Human immunoglobulin Antirhesus and its analogues
| Name and country of origin | Release form and composition | Contraindications and adverse reactions | Price in pharmacies in Moscow |
| Human immunoglobulinAnti-Rhesus – Russia | The solution for intramuscular administration is placed in ampoules, packaged in cardboard packs (each containing either 1 or 10); containing only the active substance. | Hypersensitivity to the drug; the presence of Rh antibodies in “negative” blood. Rarely causes allergies, more often - an increase in temperature, difficulties in digesting food. | from 3630 rubles (at 28 weeks it is supposed to be done free of charge for the Rh-negative expectant mother at the antenatal clinic) |
| KamROU – Israel | A solution for intramuscular injection, sold in bottles, along with a needle that has a filter; auxiliary components of the product - glycine, water for injection. Shelf life - 2 years. | The contraindications are the same - plus, according to the instructions, it cannot be used by Rhesus-positive women; the side effects are the same as the Russian drug. | from 5775 rubles |
| HyperROU S/D - USA | The solution is administered intramuscularly, available in disposable syringes with a needle, packaged in cardboard boxes; additional substances - glycine, water for injection. Validity period - 3 years. | The prohibitions and side reactions are the same as for KamROU; | from 3900 rubles |
| Resonant – Austria | Solution for injections intramuscularly, sold in ampoules of 1-5 pieces, placed in plastic packages; auxiliary components - glycine, sodium chloride, sodium acetate, water for injection. Shelf life: 2.5 years. | There is only one contraindication - allergy to substances from the drug; side effects:
| from 3500 rubles |
| Partobulin SDF - Austria | The solution for intramuscular administration is contained in a syringe that is ready for use; auxiliary components are glycine, sodium chloride, macrogol, water for injection. Shelf life is 24 months. | Contraindications are the same as for KamROU; adverse reactions:
| from 5500 rubles |
How to avoid Rh conflict
There is a chance not to have unpleasant symptoms and consequences if:
- find out Rh factors from your parents and identify yours as a result of testing in the clinic;
- start administering the drug to the woman in labor if the born child is Rh positive and she is Rh negative;
- check your blood regularly for antibodies;
- stand in line for antenatal clinic;
- take vitamin complexes so that the child does not need anything in the womb.
Are immunoglobulin injections always necessary for Rhesus conflict? You will find out the answer from the video:
Indications for the use of immunoglobulin during pregnancy
Direct indications for the use of serum are:
- opposite rhesus indicator in the fetus;
- risk of miscarriage;
- high risk of Rh conflict;
- diabetes;
- violation of the placental barrier;
- placental abruption;
- peritoneal injuries;
- late toxicosis in severe form;
- ectopic pregnancy;
- “positive” blood from the father;
- abortion;
- infectious diseases.
Doctors distinguish several forms of the disease:
- The first form is a very severe feature; general edema occurs in the fetus; in the event of complications, the child may die from cardiac arrest, which is provoked by anemia and edema. Unfortunately, such cases do occur, but this does not mean that a woman with negative rhesus cannot give birth.
- The second form is the appearance and manifestation of the so-called “jaundice”. As the substance bilirubin spreads, the newborn's body becomes yellow-gray. The sign is bad - perhaps brain damage due to toxic substances that destroy red blood cells.
- The third form is anemia, which occurs even at the stage of fetal formation. The child is born very pale - this is a sign of anemia. However, this diagnosis does not mean that in the future the child will be severely and often ill. It all depends on the form and ability of specialists to competently provide for the lactation period. It is possible that hemolytic disease does not progress, its mild forms will remain. Now the Rhesus conflict is instantly determined, everything is done to avoid problems in the future.
In general, doctors prescribe treatments that minimize the undesirable consequences of negative Rh. But it is worth remembering that a lot also depends on the psychological mood of the expectant mother. Anxiety and stress are factors that are best excluded, even if the woman received recommendations from a doctor and was informed about negative Rh. When a conflict occurs, there are many preventive measures that will prevent dangerous diseases and death of the child.
It is worth remembering that a second pregnancy with a negative Rhesus in the mother also has its own characteristics. The antibody content increases over the years, especially during the second pregnancy. This means that you need to monitor your health much more scrupulously. Some take drastic measures and do a blood transfusion, which under certain circumstances is simply a forced decision, but it may also happen that there are no indications for this procedure. Again, it is impossible to say about this without examining all the tests.
Side effects
In most cases, the administration of immunoglobulin is tolerated by expectant mothers normally, without unpleasant consequences. In some cases, there may be a slight increase in body temperature, up to a maximum of 37.5 degrees. In one case per hundred administrations, dizziness and headache, nausea, diarrhea, changes in blood pressure, shortness of breath, and redness at the injection site are observed. Even less common are increased sweating, chills, cramps, and muscle pain. Anaphylactic shock in response to vaccination is rather rare; such cases are rare.
Despite the fact that most pregnant women tolerate the injection well, the expectant mother should be under medical supervision for half an hour after administration. Anti-shock therapy should be available in the room in case of rare adverse reactions.